1- Non-immune hemolytic anemia
advertisement

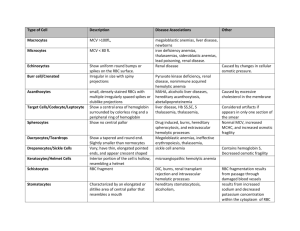
HEMOLYTIC ANEMIA Introduction One of the reasons leading to anemia development is when the rate of red blood cell destruction exceeds the rate of production of normal red blood cell from the bone marrow. In the case of maturational (or developmental) defect within the bone marrow, the resultant anemia is associated with the production of low, normal, (or even increased) numbers of abnormal RBC’s, which do not function properly. In other words, the primary cause of the anemia is the malfunctioning RBC’s, whether accompanied with decreased numbers or not. In hemolytic anemia, the rate of production is usually normal to very increased but anemia arise due to the continuous hemolysis (destruction) of RBC’s. In other words, the BM is going through "effective erythropoiesis" but for some reason, the RBC's produced are still not doing their function properly. This type of anemia is different from anemia resulting from "ineffective erythropoiesis" where the BM is responsible about the production of defective and/or decreased amounts of RBC's. Usually, the causes behind ineffective erythropoiesis are related to BM biological dynamics. So, this group of conditions which results from increased destruction of the RBC, characterized by: Reduced life span of RBS. Lec Tagreed Mohammed Hemolytic Anemia Page 1 of 6 Hb and PCV are both low. Increased Bone Marrow activity. Classification Hemolytic anemia is classified to two major categories according to the cause (etiology) of hemolysis. These reasons for hemolysis are either of: 1- intrinsic, or 2extrinsic natures. I- Intrinsic hemolytic anemia This is a group of anemia where the defect causing the “hemolysis” is an internal one. That is, the defect is caused within the RBC’s themselves usually due to an congenital error in the genetic make up of the cells. In other words, the RBC’s were synthesized defective in one or more of its vital compartments. All of the intrinsic hemolytic anemias are inherited disorders except for one type which is acquired (see below). i- Hereditary: As the name implies, this sub group is passed down from the parents to their children, and it is further sub-divided into three major groups according to the type of defect: 1- Membrane defects: As the name suggests, this group of anemia have a malfunction in their membrane components. These include: A- Hereditary Spherocytosis. B- Hereditary elliptocytosis. C- Hereditary stomatocytosis (Hydrocytosis). Lec Tagreed Mohammed Hemolytic Anemia Page 2 of 6 2- Enzyme defects: The diseases in this group are referred to as “Hereditary Erythrocyte Enzymopathies”. This is a group of anemia caused by the quantitative or qualitative abnormalities of one or more crucial functional enzymes leading to abnormally functioning RBC’s, and hence anemia. This group includes anemia such as: A- Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency. B- Pyruvate Kinase deficiency. C- Glutathione Reductase deficiency. 3- Hemoglobinopathies: This is a group of diseases caused by defective globin chains synthesis usually leading to unstable or very fragile hemoglobins. The group contains a large number of unstable hemoglobins. Some of the most important types of this anemia are: Sickle cell anemia (SS), CC disease , SC disease, and S-β thalassemia. ii- Acquired: Acquired intrinsic hemolytic anemia is not common with only one known anemia called the Paroxysmal Nocturnal hemglobinuria (PNH). II- Extrinsic Hemolytic Anemia This is a group of anemia where the defect causing the “hemolysis” is an external one. That is, the defect is caused by some agent(s) outside the components of the RBC’s themselves. Usually this is caused by: other organ failures (as seen most frequently with the kidneys and liver), an invading organism, auto immune diseases, etc. In other words, the RBC’s were synthesized normally (whether in numbers or in quality and function) but for some reason the cells are being attacked and destructed by other tissues (kidneys, liver, spleen, macrophages, etc.) or some foreign invading organisms. Extrinsic hemolytic anemia is also classified to hereditary and acquired causes however unlike the intrinsic ones, the acquired are the most frequently encountered. 1- Hereditary: Lec Tagreed Mohammed Hemolytic Anemia Page 3 of 6 Rarely seen, there are only two types of this anemia. 2- Acquired: Under this classification, a large number of factors can lead to the development of hemolytic anemia. These include: ABCDEF- Hypersplenism. Hypertension. Liver and/or renal diseases. Auto Immune. Infectious agents. Mechanical, thermal, and/or chemical damage. ACQUIRED HEMOLYTIC ANEMIA Introduction Unlike HS and G6PD deficiency hemolytic anemias, the group of hemolytic anemias under this category, are all acquired (not hereditary transmitted). On contrast, to HS and G6PD the majority of this group of anemias are caused by, an extrinsic defects (factors leading to hemolysis). The group is further sub-divided to the nature of the pathophysiology involved, into two major categories: 1- Those of non-immune nature 2- Those caused by immunologic defects, known as Immune Hemolytic Anemia ( IHA). 1- Non-immune hemolytic anemia The majority of this class of anemia is caused by external factors (outside the RBC’s themselves) affecting the small blood vessels. A- The classical and most frequently known cases are referred to as the MicroAngiopathic Hemolytic Anemia (MAHA). Examples of such hemolytic anemias are seen in: Lec Tagreed Mohammed Hemolytic Anemia Page 4 of 6 1- Disseminated Intravascular Coagulation (DIC) 2- March Hemoglobinurea (very rare with no pb evidence of hemolysis) It is extremely important to distinguish between the above-mentioned types and the Paraxosymal Nocturnal Hemoglobinurea (PNH), which is an acquired defect but of INTRINSIC nature (i.e., the defect is within the RBC’s themselves). 2- Acquired Immune hemolytic Anemia (AIHA) This group is sub-classified to three major classes: A- Alloimmune B- Autoimmune C- Drug Induced 1-ALLOIMMUNE This class includes two types of anemias: 1- Hemolytic Disease of the Newborn (HDN). 2- Hemolytic Transfusion Reactions 2-AUTOIMMUNE This class encompasses a large range of hemolytic anemias, which are sub-categorized according to the nature of the “antibodies” involved to three types: 1- Cold antibody 2- Warm antibody 3- Paraxosymal cold hemoglobinurea (PCH). The anemias of each of these classes could be either Primary (idiopathic, i.e., caused by unknown factors) or Secondary to known factors such as: iiiiiiivvvivii- Chronic Lymphocytic Leukemia (CLL) Viral infections Lymphoma Infectious Mononucleosis (Epstein-Barr Virus) Syphilis Systemic Lupus erythematosus (SLE) Mumps, Measles, and Chicken pox. Lec Tagreed Mohammed Hemolytic Anemia Page 5 of 6 3-DRUG-INDUCED Certain drugs have been associated with hemolytic reactions. Examples of such drugs are Hapten, and alpha-methyldopa. Site of hemolysis Hemolysis of RBC’s can occur either intra-vascularly or extra-vascularly. Most of the destruction of normal or abnormal RBC’s occurs in the Reticulo-Endothelial System (RES), which include the spleen, liver, lymph nodes, lungs, and the bone marrow. Extra-vascular hemolysis is the type of hemolysis where whole intact RBC’s or their fragments are destroyed by macrophages of the RES ending in the release of hemoglobin into the macrophages. Most of the hemolytic anemias are characterized by such hemolysis. Intravascular hemolysis occurs when RBC’s are destroyed within the blood vessels before reaching the RES. This might occur when the damage to the RBC’s is very severe. Such hemolysis is rarely seen in hereditary hemolytic anemias, but is more associated with acquired cases such as hemolytic reaction due to mismatched ABO blood grouping transfusions (transfusion reaction), MicroAngiopathic Hemolytic Anemia (MAHA), heart valves diseases, malarial infestation, clostridium septicemia, severe kidney and liver diseases. Lec Tagreed Mohammed Hemolytic Anemia Page 6 of 6