RESIDENT CURRICULUM FOR ENDOCRINOLOGY, DIABETES
advertisement

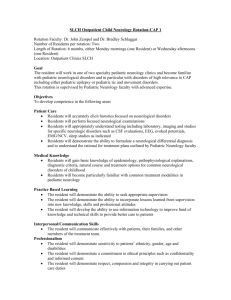
Revised March 23, 2008 GOALS AND OBJECTIVES RESIDENT ROTATION IN NEUROLOGY 2008-2009 Rotation Coordinator: Steven Glyman, M.D. 1707 W. Charleston Blvd. #230 Chief, Division of Neurology University of Nevada School of Medicine Las Vegas, Nevada 89102 OVERVIEW EDUCATIONAL PURPOSE The purpose of this four-week rotation is to provide education and experience in the care of patients with known or suspected neurologic disease. The residents provide inpatient consultations for University Medical Center. Residents see patients with neurologic conditions at the UMC outpatient clinic, the VA ambulatory clinic, and the UNSOM faculty clinic. The general internist should possess a broad range of competency in neurology. He or she should be able to perform and interpret a detailed neurologic examination; should be competent in the primary and secondary prevention of neurologic diseases; and should be familiar with the presenting features, diagnosis and treatment of common neurologic disorders. The general internist may encounter neurologic disorders in various settings, including ambulatory care, hospital, long-term care and home care. In communities where a neurologist is not available, the general internist may be a consultant for some complex neurologic disorders (for example, control of status epilepticus). At the conclusion of this rotation residents will have gained insight into the diagnosis and management of patients with neurologic diseases, their role as subspecialty consultant, diagnostic methods of neurologic diseases, the natural history of neurologic disease, and strategies for cost-effective and evidence-based evaluation and treatment. This curriculum is based, in part, upon the report of the Federated Council for Internal Medicine Task Force on the Internal Medicine Residency Curriculum. Neurology encompasses the prevention and management of disorders of the central and peripheral nervous systems. Other conditions, such as headache, may be caused by non-neural dysfunction but are often considered under the category of neurology. 1 Teaching Methods The resident will see each new consultation first, create a note with recommendations, and then present the patient to the attending neurologist. The attending will evaluate the patient and provide teaching and feedback, after which final recommendations will then be made. The resident will be working closely with the attending neurologist providing daily progress notes and follow-up recommendations for the care of each patient. Daily rounds will occur with the attending physician at which time instruction in the unique aspects of the consultative process will be provided. Residents will be required to continue their regular Morning report and Noon conference core curriculum. The resident and attending will review and discuss each required reading. Patients seen in the neurology clinic will be seen and staffed in an analogous manner. Mix of Diseases The patients seen will represent the very wide spectrum of neurology disorders encountered in our inpatient setting and outpatient clinics. Common Clinical Presentations Residents will become knowledgeable of the diagnosis, management, and complications of the following neurologic disorders encountered in an inpatient setting: central nervous system infections (meningitis, encephalitis, brain abscess, epidural abscess), cerebrovascular disease (stroke, transient ischemic attack), epilepsy, multiple sclerosis, neuromuscular diseases (myopathy, amyotrophy, Guillain-Barre syndrome, Myasthenia gravis), subarachnoid hemorrhage, subdural hematoma, and toxic encephalopathies. The resident will become knowledgeable of the diagnosis, management, and complications of the following neurologic disorders encountered in an outpatient setting: dizziness, vertigo, altered sensation (including localized pain syndromes and radiculopathies), weakness/paresis (both generalized and localized), abnormal speech, abnormal vision, disturbed gait or coordination, headache, seizure, tremor, dementia’s and impaired memory, sleep disorders, hearing loss, Parkinsonism, peripheral neuropathies and spinal disc syndromes. Common presentations include: Abnormal speech Abnormal vision Altered sensation Confusion Disturbed gait or coordination Dizziness, vertigo Headache Hearing loss Localized pain syndromes: facial pain, radiculopathy Loss of consciousness Memory impairment Seizure 2 Sleep disorder Tremor Weakness/paresis (generalized, localized) Common Procedures Caloric stimulation test Tensilon (edrophonium chloride) test (optional) Halsted – Baranay maneuver Lumbar puncture Ordering and Understanding Tests Anticonvulsant drug levels Carotid Doppler echo scans Computed tomography, magnetic resonance imaging of central nervous system Digital intravenous angiography Electroencephalography, evoked potentials (visual, auditory, sensory) Electromyography, nerve conduction studies Muscle biopsy Myelography Screen for toxins, heavy metals Sleep study Patient Characteristics The patient population is diverse, male and female, of all ages from adolescent to geriatric, representing most ethnic and racial backgrounds, from all social and economic strata. The hospital serves primarily the indigent population of the city of Las Vegas. Types of Clinical Encounters All patient encounters are in the inpatient setting on a consultative basis from other clinical services or from an ambulatory physician who has referred a patient for admission. Close interaction with various other healthcare team members including care managers, discharge planners, home health agencies, inpatient nurses, respiratory therapists, physical therapists, and patient care technicians occurs daily. Resident Supervision Residents have constant on site supervision as well as daily personal supervision in their patient care. Didactic Teaching 3 Morning Report Residents rotating on the neurology service are required to maintain greater than 60 % attendance at morning report. Morning Report begins at 8 a.m. on Monday through Thursday and at 8:30 a.m. on Friday. Noon Conference Residents rotating on the neurology service are required to maintain greater than 60% attendance at noon conference. Noon conference occurs daily, Monday through Friday. These sessions cover the basic core curriculum, and other curriculum topics such as ethical issues, geriatrics, computer systems and informatics, health care systems, occupational and environmental health issues, and other topics of concern. An infectious disease topic is presented at least once during each month. Attending Rounds Didactic discussions will be held regarding all consultative activities and patients seen during the month. Teaching rounds by the attending physician will occur every day for 45 - 60 minutes after regular management rounds. Each resident is required to review neurology topics. Core Reading Materials Adams and Victor's Principles of Neurology 8th ed., Ropper AH, editor Harrison’s Principle’s of Internal Medicine, 16th ed., Kasper DL, editor. McGraw Hill The Washington Manual of Medical Therapeutics, 32nd ed. The Washington Manua Neurology Survival Guide, Rengachary D, editor. Lippincott Williams & Wilkins Ancillary Educational Materials Subspecialty Texts of Neurology, Pulmonary Medicine, Nephrology, Endocrinology, Infectious Diseases, Rheumatology as well as General Medical References (Harrison’s Principles of Internal Medicine, Cecil’s Textbook of Medicine) are available 24 hours a day, seven days a week in the resident lounge. Savitt Medical Library On-Line Residents have access to the on-line services of Savitt Library (the main library of the University of Nevada - Reno) via their computer in the resident room, Suite 300 of the 2040 W. Charleston Building. Access to this room is available 24 hours a day, seven days a week. Full text is available for many peer-review journals including, but no limited to: ACP Journal Club Annals of Internal Medicine British Medical Journal Cancer Circulation 4 Journal of the American College of Cardiology The Lancet New England Journal of Medicine Stroke Also available on-line: Harrison’s Principle’s of Internal Medicine, 16th ed. Merck Manual, 17th ed. Guide to Clinical Preventive Services, 2nd ed. The Cochrane Library Medline and Grateful Med Databases Pathological Material and Other Educational Resources Residents are encouraged to review the pathological reports on patients for whom they have consulted and to follow the hospital care of those patients. If a patient with whom the resident has consulted should die and have an autopsy, the resident is encouraged to attend the post-mortem session. Training Sites University Medical Center All of the inpatient endocrine consultation experience occurs at University Medical Center (UMC) under the supervision of one of the full-time neurology faculty. The resident will also participate in the UMC outpatient neurology clinic each Monday. II. Competency-based Goals and Objectives Neurology (Only a single level of competency is described, as this is a resident-level rottion undertaken once during residency) Learning Venues Evaluation Methods 1. Direct patient care/consultations 2. Attending Rounds A. Attending evaluation B. Direct Observation 3. Residency core lecture series C. Nurse evaluations 4. Self study D. Written Examination 5. Morning Reports E. Resident/Self Evaluation F. Patient Evaluation 5 Level Specificity This will occur during either PGY2 or -3 level, with no difference in expectations or standards for each year Competency: Patient Care Learning Venues 1,2 Evaluation Methods A, B, E 1, 2 A, B, E NA 1, 2 A, E NA 1, 2, 3, 4, 5 A, B, D, E NA 1, 2, 3, 4, 5 A, B, D, E Competency : Medical Knowledge Learning Venues Evaluation Methods Demonstrate knowledge of the established basic biomedical, clinical and social sciences Acquire and critically evaluate current medical information and scientific evidence Apply this knowledge toward clinical problem-solving and clinical decisionmaking for individual patients 1, 2, 3, 4, 5 A, B, D, E NA 1, 2, 3, 4 A, B, D, E NA 1, 2 A, B, D, E NA Gather accurate, essential information from the medical interview, physical examination, laboratory data (including blood work, fluid analysis and radiographs), and review of medical records Provide consultation and direct the management of patients with neurologic disease Become familiar with the procedures inherent to the practice of neurology including lumbar puncture, and caloric stimulation tests. Become familiar with the tests common to neurology including electroencephalography, computed tomography and magnetic resonance imaging of the central nervous system, electromyography and nerve conduction studies, muscle biopsy, myelography, anticonvulsant drug levels, and carotid doppler scans. Make informed decisions and recommendations about preventive, diagnostic and therapeutic options and interventions based upon clinical judgment, scientific evidence and patient preference 6 Level NA NA Level Apply this knowledge toward the education of patients, families, medical students, fellow residents and other health professionals 1, 2 A, B, D, E Competencies: Interpersonal and Communication Skills Learning Venues Evaluation Methods Maintain comprehensive, timely and legible medical records Supervise, lead, manage, and teach more junior house staff and medical students Effectively communicate with consultants, peers, other allied health professionals, as well as patients and their families Communicate with patients and their families regarding end-of-life issues, categorization, organ donation, and requests for autopsies Ensure adequate transfer of information when transferring patient to care of another physician or signing out to coverage Communicate efficiently and effectively with referring physician, regarding diagnosis, treatment and follow-up. 1, 2 A, B, C NA 1, 2 A, B, C, D, E NA 1, 2 A, B, C. E NA 1, 2 A, B, C, E, F NA 1, 2 A, B, C, E NA 1, 2 A, B, C, E NA Competency: Professionalism Learning Venues Evaluation Methods Demonstrate respect, compassion, integrity, and altruism in relationships with patients, families, and colleagues Demonstrate sensitivity and responsiveness to the gender, age, culture, religion, sexual preference, socioeconomic status, beliefs, behaviors and disabilities of patients and professional colleagues Always act in a moral, ethical and professional manner Responsibly represent this residency program, the department of Internal Medicine, the University of Nevada 1, 2 A, B, C, E, F NA 1, 2 A, B, C, E, F NA 1, 2 A, B, C, E, F NA 1, 2, 3, 5 A, B, C, E, F NA 7 NA Level Level School of Medicine, the University Medical Center and the profession of medicine Respect and defend each patients’ autonomy and privacy and always act in the patients’ best interest Competency: Practice-Based Learning Access current information from the scientific and practice literature to support and improve your clinical practice Develop and maintain a willingness to learn from errors and use errors to improve the quality of patient care Incorporate case studies with relevant research outcomes and report those findings during clinical rounds. Review the outcomes of patient care in order to reflect on the approach taken in the delivery of care. Utilize established practice guidelines for individual diseases to devise care strategies. Identify limitations of one’s medical knowledge in evaluation and management of patients and use medical literature (primary and reference) to address these gaps in medical knowledge. Competency: System-Based Practice Understand need for effective communication between multiple caregivers (i.e. emergency room, critical care unit, nurses, physicians, transporters, outpatient clinic, radiology, laboratory). Understand clinical trial design and the statistical methods for evaluating scientific studies, in cooperation with attendings and research nurses/personnel. Learn appropriate use of medical and non-medical subspecialties 1, 2 A, B, C, E, F Learning Venuses 1, 2, 4, 5 Evaluation Methods A, D, E 1, 2, 4 A, E NA 1, 2, 3, 4, 5 A, B, E NA 1, 2, 3, 4, 5 A, B, E NA 1, 2, 4 A, B, E NA 1, 2, 4, A, E NA Learning Venues 1, 2, 3, 4 Evaluation Methods A, E Level 1, 2, 3, 4, 5 A, B, C, E NA 1, 2, 4 A, B NA 8 NA Level NA NA Understand and access all resources available and necessary to provide optimal patient care Apply evidence-based and cost-conscious strategies toward disease prevention, diagnosis and disease management Develop lifelong strategies to optimize care for individual patients VI. 1, 2, 4 A, B, E NA 1, 2, 4 A, B, E NA 1, 2, 4 A, B, D, E NA EVALUATION A. Of Residents All clinical faculty are required to complete the standard ABIM resident evaluation form. All clinical faculty are encouraged to provide face-to-face feedback with the residents. B. Of Rotation and Preceptor All residents have the opportunity to evaluate the rotation, and the clinical faculty member, at the completion of the rotation. The form is included at the end of this document. These evaluations are then converted to type and shared anonymously with the clinical faculty. The program director also discusses the rotation with the residents to ensure rotation quality and satisfaction. 9 Neurology Rotation Resident Check List 1. Evaluation reviewed at mid-month and end of rotation by the supervising faculty member and resident. 2. Completed assigned readings. 3. Attended all assigned clinical activities (excluding scheduled time away, required clinics and emergencies). 4. Completed required case report abstracts and/or posters assigned by the supervising faculty member. 5. Demonstrated understanding of the basic principals of neurologic consultation and management. 6. Received verbal feedback at end of rotation. Intern/Resident Signature___________________________ Date_________________ Supervising Faculty_______________________________ Date_________________ All items must be completed for rotation credit and checklist returned to the Department of Medicine by the month’s end. 10