Stroke Transient Ischemic Attack TIA Ischemic Stroke
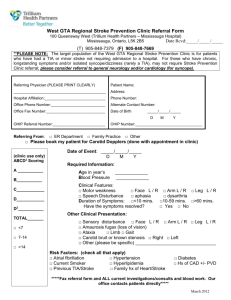
advertisement
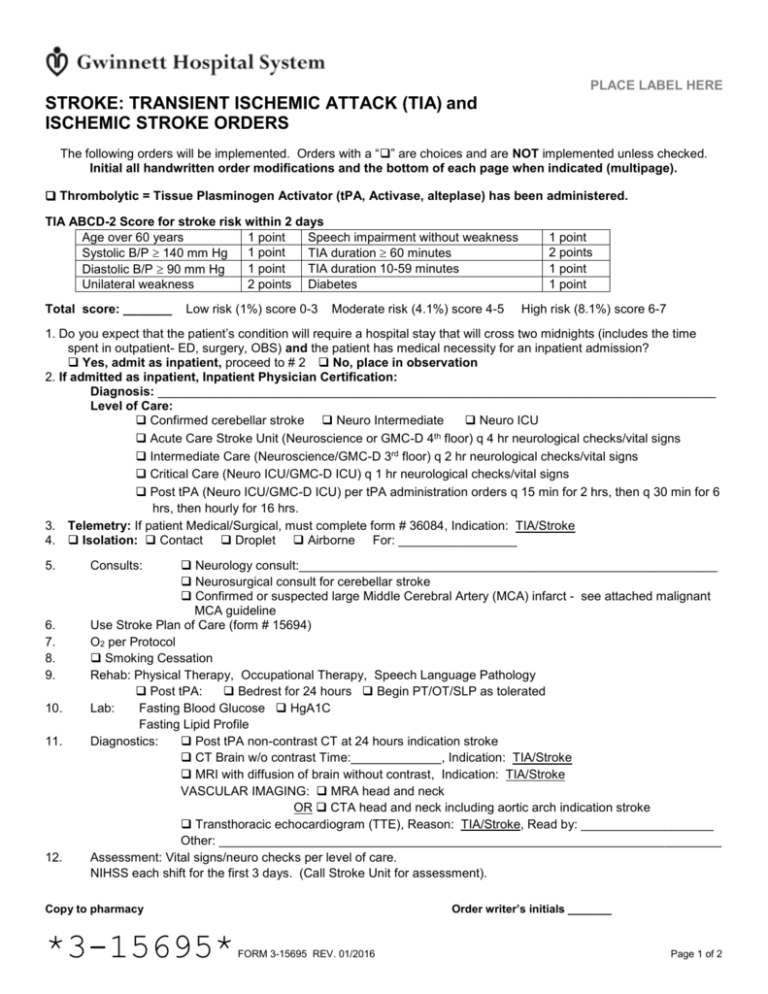
PLACE LABEL HERE STROKE: TRANSIENT ISCHEMIC ATTACK (TIA) and ISCHEMIC STROKE ORDERS The following orders will be implemented. Orders with a “” are choices and are NOT implemented unless checked. Initial all handwritten order modifications and the bottom of each page when indicated (multipage). Thrombolytic = Tissue Plasminogen Activator (tPA, Activase, alteplase) has been administered. TIA ABCD-2 Score for stroke risk within 2 days Age over 60 years 1 point Speech impairment without weakness 1 point Systolic B/P 140 mm Hg TIA duration 60 minutes 1 point TIA duration 10-59 minutes Diastolic B/P 90 mm Hg Unilateral weakness 2 points Diabetes Total score: _______ Low risk (1%) score 0-3 Moderate risk (4.1%) score 4-5 1 point 2 points 1 point 1 point High risk (8.1%) score 6-7 1. Do you expect that the patient’s condition will require a hospital stay that will cross two midnights (includes the time spent in outpatient- ED, surgery, OBS) and the patient has medical necessity for an inpatient admission? Yes, admit as inpatient, proceed to # 2 No, place in observation 2. If admitted as inpatient, Inpatient Physician Certification: Diagnosis: ________________________________________________________________________________ Level of Care: Confirmed cerebellar stroke Neuro Intermediate Neuro ICU th Acute Care Stroke Unit (Neuroscience or GMC-D 4 floor) q 4 hr neurological checks/vital signs Intermediate Care (Neuroscience/GMC-D 3rd floor) q 2 hr neurological checks/vital signs Critical Care (Neuro ICU/GMC-D ICU) q 1 hr neurological checks/vital signs Post tPA (Neuro ICU/GMC-D ICU) per tPA administration orders q 15 min for 2 hrs, then q 30 min for 6 hrs, then hourly for 16 hrs. 3. Telemetry: If patient Medical/Surgical, must complete form # 36084, Indication: TIA/Stroke 4. Isolation: Contact Droplet Airborne For: _________________ 5. 6. 7. 8. 9. 10. 11. 12. Neurology consult:____________________________________________________________ Neurosurgical consult for cerebellar stroke Confirmed or suspected large Middle Cerebral Artery (MCA) infarct - see attached malignant MCA guideline Use Stroke Plan of Care (form # 15694) O2 per Protocol Smoking Cessation Rehab: Physical Therapy, Occupational Therapy, Speech Language Pathology Post tPA: Bedrest for 24 hours Begin PT/OT/SLP as tolerated Lab: Fasting Blood Glucose HgA1C Fasting Lipid Profile Diagnostics: Post tPA non-contrast CT at 24 hours indication stroke CT Brain w/o contrast Time:_____________, Indication: TIA/Stroke MRI with diffusion of brain without contrast, Indication: TIA/Stroke VASCULAR IMAGING: MRA head and neck OR CTA head and neck including aortic arch indication stroke Transthoracic echocardiogram (TTE), Reason: TIA/Stroke, Read by: ___________________ Other: ________________________________________________________________________ Assessment: Vital signs/neuro checks per level of care. NIHSS each shift for the first 3 days. (Call Stroke Unit for assessment). Consults: Order writer’s initials _______ Copy to pharmacy *3-15695* FORM 3-15695 REV. 01/2016 Page 1 of 2 PLACE LABEL HERE STROKE: TRANSIENT ISCHEMIC ATTACK (TIA) and ISCHEMIC STROKE ORDERS The following orders will be implemented. Orders with a “” are choices and are NOT implemented unless checked. Initial all handwritten order modifications and the bottom of each page when indicated (multipage). 13. 14. 15. 16. Diet: NPO until bedside swallow screen per RN If swallow screen normal, begin diet as tolerated: ____________________________________________ If swallow screen abnormal, maintain NPO, elevate head of bed 30°, and await Speech Language Pathology evaluation Nutrition Supplement Orders (form # 31417), initiate if patient meets criteria Foley Catheter Removal and Voiding Assessment/Interventions Standing Orders (form # 31620) Activity: Progress as tolerated MEDICATIONS: 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. IVF: NS LR D5NS D5 ½ NS with 20 KCl at ___________ml/hr Antiplatelet: If tPA administered, hold first dose of all antiplatelet or anticoagulant drugs including, but not limited to: Heparin, Lovenox (enoxaparin), Coumadin (warfarin), Pradaxa (dabigatran), Xarelto (rivaroxaban), Eliquis (Apixaban), Aspirin, Aggrenox (aspirin/dipyridamole), Plavix (clopidogrel), Effient (prasugrel) or Brilinta (ticagrelor) for 24 hrs Aspirin 325 mg po or per rectum daily Aspirin 81 mg po daily Plavix (clopidogrel) 75 mg po daily Other: ___________________________ Blood pressure management: Trandate (labetalol) 10-20 mg IV q 1 hr PRN HTN (see below), Hold for heart rate < 50/min. Recheck BP within 30 min and notify physician if not in parameters. Hydralazine 10 mg IV q _____ hrs PRN HTN (see below), Recheck BP within 30 min and notify physician if not in parameters. ICU only, Cardene (nicardipine): Initial infusion 5 mg/hr, increase by 2.5 mg q 15 min to max of 15 mg/hr, see Titration Protocol (form # 33883) Blood Pressure (BP) Administration Parameters (must be completed): Permissive HTN: Maintain BP ≤ 220 mm Hg systolic and/or ≤ 120 mm Hg diastolic. or Maintain systolic BP < _____ mmHg and/or diastolic BP < _____ mmHg. or DC other parameters if thrombolytic or anticoagulant given, keep systolic B/P ≤ 180 mm Hg and/or diastolic BP ≤ 105 mm Hg. or Notify physician if systolic BP > _____ mmHg and/or diastolic BP _____ mmHg for medication orders. Cholesterol lowering therapy recommended for LDL > 100 mg/dl or consider for diabetics LDL > 70 mg/dl Contraindication to statin therapy Lipitor (atorvastatin) _________________mg po at bedtime Other: _____________________________________________________mg po at bedtime VTE prophylaxis, Initiate Venous Thromboembolism (VTE) Prophylaxis Orders (form # 33058) Heparin 5,000 units SQ q 8 hrs (q 12 hrs if wt < 50 kg or age > 75). Hold for 24 hrs if tPA administered or Lovenox (enoxaparin) 40 mg SQ daily at 1700 (30 mg if CrCl < 30) Hold for 24 hrs if tPA administered and/or Mechanical devices: SCDs Nicotine patch 14 mg once daily prn apply topically after smoking cessation education Mild pain/temp > 99.5F/HA: Tylenol (acetaminophen) 650 mg po or per rectum q 4 hrs prn Stool Softener: Colace (docusate) 100 mg po bid prn; if patient has not had a bowel movement Constipation: Milk of Magnesia (MOM) 30 ml po daily prn Electrolyte Replacement Protocol (form # 21340) ___________ Date ____________ Time _________________________________ Physician Signature ____________ PID Number Copy to pharmacy FORM 3-15695 REV. 01/2016 Page 2 of 2 REFERENCE - Not Part Of Medical Record Guidelines for Neurosurgical Consult and Possible Decompressive Hemicraniectomy in Malignant Middle Cerebral Artery Infarctions Large volume > 50% of MCA territory infarction on CT or DWI volume > 145 ml on MRI after 16 hours of onset of symptoms NIHSS > 16 for non-dominant hemisphere stroke or NIHSS > 20 for dominant hemisphere stroke Patients < 60 yrs with malignant MCA infarction Decompressive hemicraniectomy should preferably be performed within 48 hours of stroke onset Decompressive hemicraniectomy should be offered on a case by case basis for healthy patients > 60 yrs and beyond 48 hrs after stroke onset A thorough discussion with the patient and family about limited evidence of benefit, and likelihood of poor neurologic outcome needs to be addressed. Adequate craniectomy with a target 14 cm anterior, posterior and temporal bone removed down to the middle fossa and duroplasty Above is based on Class 1: Level of Evidence B from the American Stroke Association 2013 Ischemic Stroke Guidelines. Jauch, E et al. (2013). Guidelines for the Early Management of Patients With Acute Ischemic Stroke. Stroke. Jan. 31, 2013 REFERENCE - Not Part Of Medical Record