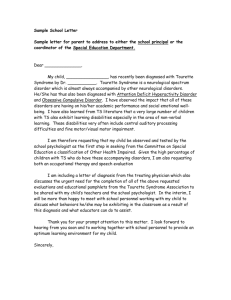
doc - Kleefstra syndrome

Kleefstra syndrome
9q34.3 Deletion syndrome
Questionnaire
(also known as chromosome 9q subtelomere deletion syndrome, 9qSTDS, CHOMS,
9q34 deletion syndrome, deletion 9qter syndrome, hapE1 syndrome, 9q- syndrome)
[1]
1.1 Contact details
1.1.1
Contact name(s)
1.1.2
Address
1.1.3
Post code / Zip code
1.1.4
Country
1.1.5
1.1.6
Telephone
1.2 I am happy to be contacted by other 9q34.3 deletion syndrome families YES NO
1.3
I am happy to be notified of new research studies into the syndrome YES NO
1.4
1.5
1.6
Child’s name:
Sex MALE
Birth date (dd/mm/yyyy)
FEMALE
2 Genetics information
2.1 Karyotype and/or molecular results (chromosomes) / array test results etc.
3 Conception, Pregnancy & Labour
3.1 Conception
[2]
3.1.1 Normal Yes No
3.1.2 Difficulty Conceiving Yes No
3.1.3 IVF Yes No
3.1.4 Other (specify)
3.2 Describe any pregnancy problems, including small size, lack of fetal movement, excessive amniotic fluid, labour problems, or premature birth.
4 Newborn
4.1 Gestational age: weeks
4.2 Apgar Scores (if known)
4.3 Birth weight
4.4 Birth length
4.5 Head circumference at birth days
4.6 Was your baby floppy (hypotonic) at birth? Yes No
4.6.1 If YES, at what age was this first noticed?
4.7 Was your baby jaundiced after birth?
4.7.1 If YES, for how long?
Yes No
4.8 Mother’s blood group
4.9 Child’s blood group
4.10 Describe any problems your baby had in the newborn period.
[3]
5 First signs
5.1 What were the first signs that your baby or child might have a chromosome disorder?
5.2 When in the pregnancy/ after the birth/in later life were these signs noticed?
5.3 Who first noticed these signs? E.g. parent, paediatrician, nurse, geneticist, therapist etc
6 Craniofacial features (appearance of the face and head)
6.1 Head shape
6.1.1 Head circumference in cm: at age years months days
6.1.2 Small head (microcephaly) Yes No
6.1.3 Wide head/flat at the back (brachycephaly)
6.1.4 Craniosyntosis
Yes
Yes
No
No
6.1.5 Delayed closure of fontanels Yes
6.1.6 Other cranial anomalies (head shapes and sizes)(Please describe)
No
[4]
6.2 Nose
6.2.1 Broad nasal bridge
6.2.2 Slightly upturned nose Yes
Yes
No
6.2.3 Baby shape nose Yes
No
No
6.2.4 Other nasal anomalies (describe)
6.3 Eyebrows
6.3.1 Eyebrows that meet in the middle/”Unibrow” (Synophrys)
6.3.2 Arched eyebrows Yes No
No
No
6.3.3 Straight eyebrows Yes
6.3.4 Low set eyebrows Yes
6.3.5 Other eyebrow anomalies (specify)
6.4 Eyelashes
6.4.1 Long eyelashes
6.4.2 Short Eyelashes
Yes
Yes
6.4.3 Other eyelash anomalies (specify)
No
No
6.5 Eyes
6.5.1 Widely spaced eyes (hypertelorism)
6.5.2 Upslanting eyes Yes
Yes
No
6.5.3 Downslanting eyes
6.5.4 Squint (strabismus)
Yes
Yes
[5]
No
No
No
Yes No
6.5.5 Eye colour (describe)
6.5.6 Mother eye colour
6.5.7 Father eye colour
6.5.8 Almond shaped eyes
6.5.9 Other eye anomalies (specify)
6.6 Mouth
6.6.1 Open mouth (in babies)
6.6.2 Open mouth (in older children/adults)
6.6.3 Large tongue/Thick tongue
6.6.4 Protruding tongue (Tongue sticks out)
6.6.5 Tongue tie
6.6.6 Tongue forked at tip
6.6.7 Tongue deeply creased
6.6.8 Other unusual tongue shape (describe)
6.6.9 Widely spaced teeth
6.6.10 Other teeth abnormalities (describe)
6.7 Lips
6.7.1 Cupid’s bow shape upper lip Yes
6.7.2 Everted lower lip Yes
Yes
Yes
Yes
Yes
Yes
No
Yes
Yes
Yes No
No
No
No
No
No
No
No
[6]
Yes
No
No
6.7.3 Thin lips
6.7.4 Other lip anomalies (specify)
6.8 Ears
Yes No
6.8.1 Low set ears
6.8.2 Crumpled ears
Yes
Yes
6.8.3 Other ear anomalies (specify)
6.9 Hair
No
No
6.9.1 Child’s Hair Colour:
6.9.2 Is this a different colour from parents or siblings?
6.9.3 Bald patches (unlike parents or siblings)
6.9.4 Fine Wispy hair (unlike parents or siblings)
6.9.5 Thick hair (unlike parents or siblings)
6.9.6 Flaky scalp (unlike parents or siblings)
6.9.7 Patchy scalp (unlike parents or siblings)
6.9.8 Other hair anomalies (specify)
6.10 Other facial features
6.10.1 High forehead Yes
6.10.2 Flat face
6.10.3 Patches of lighter coloured skin Yes
Yes
No
[7]
Yes
Yes
No
Yes
Yes
No
Yes
Yes
No
No
No
No
No
No
6.10.4 Other feature 1 (describe)
6.10.5 Other feature 2 (describe)
6.10.6 Other feature 3 (describe)
7 Feeding
7.1
Please say whether you tried to breastfeed your baby and how you managed.
7.2
Has your child had any feeding problems - minor and temporary or severe? Describe any treatments
(such as tube feeding or a gastrostomy).
Have any of the following been a problem for your child?
[8]
7.3
Pulmonary Aspiration
7.3.1
If YES: Age(s) Treatment (if any)
7.4
Aspiration pneumonia
7.4.1
If YES Age(s) Treatment (if any)
7.5
Reflux (GORD, GERD)
7.5.1
If YES Age(s) Treatment (if any)
7.6
Fundoplication
7.6.1
If YES Age(s)
7.7
Drooling
7.7.1
If YES Age(s)
Outcome
Treatment (if any)
[9]
Yes
Outcome
No
Yes
Outcome
Yes
Outcome
Yes
Yes
Outcome
No
No
No
No
7.8
Poor chewing/swallowing without chewing
Treatment (if any) 7.8.1
If YES Age(s)
Yes
Outcome
7.9
Storing food in mouth without swallowing until another spoonful arrives Yes
7.9.1
If YES Age(s) Treatment (if any) Outcome
No
No
7.10
Oral defensiveness (Over responsiveness to particular food textures, tastes and smells which may lead to a very limited diet) Yes No
If YES describe
7.10.1 Age(s) Foods WILL eat exclusively
Foods WON’T eat at all
Outcome 7.10.2 Age(s) Treatment (if any)
7.11
Other feeding related problem (please describe)
[10]
7.12
What are your child’s favourite foods/drinks? (Include from what age they have been a favourite)
7.13
What foods/drinks does your child dislike most? (Include from what age they have indicated a dislike for the food/drink)
8 Growth
8.1
Please state whether your child is tall, average or short for their age. Tall Average Short
8.2
Is your child / has your child been overweight? Yes No
8.2.1 If Yes, by what age did the overweight develop?
8.2.2
What steps do/did you take to control his/her weight?
8.2.3
If your child is no longer overweight state at what age this problem was resolved:
8.3
Is your child / has your child been underweight? Yes No
8.3.1 If Yes, by what age did the underweight develop?
8.3.2
What steps do/did you take to control his/her underweight?
[11]
8.3.3
If your child is no longer underweight state at what age this problem was resolved:
8.4
Does your child’s belly tend to be distended regardless of whether (s)he is overweight or not ?
Yes No
8.4.1
If Yes, when would this be noticeable? (e.g. All the time, only after a meal, only when (s)he is constipated)
8.5
Please describe any other growth or weight related problems
8.6
If you have any height/weight measurements from your child’s development please include them here and specify units (e.g. inches, cm, lbs, kg)
Age of child Height Weight
[12]
9 Body systems
9.1 Heart
Has your child been diagnosed with any of the following?
9.1.1
Heart Murmur Yes No
9.1.2
Leaking heart valves Yes
9.1.3
Abnormal heart rhythms Yes
Yes
No
No
No 9.1.4
Tachycardia
9.1.5
ASD Yes No
9.1.6 VSD
9.1.8
PDA
9.1.7
Pulmonary Stenosis
Yes
Yes
Yes
No
No
No
9.1.9
Tetralogy of Fallot
9.1.10 Cardiomyopathy
Yes
Yes
9.1.11
Other heart condition (1) (describe)
9.1.12 Other heart condition (2) (describe)
No
No
[13]
9.1.13
Has your child had any imaging or other investigations of the heart? Yes
9.1.13.1
If Yes, please describe
Type of investigation Age of child
No
Outcome of investigation
9.1.13
If your child has a heart condition, how does this affect him/ her?
9.1.14
What treatment/surgery (if any) has been needed?
9.1.15
What treatment (if any) is anticipated?
[14]
9.2 Seizures
9.2.1
Has your child had any seizures (fits)? Yes No
If Yes, describe below
Type of seizure
9.2.1.1
Infantile spasms
Age Treatment
9.2.1.2
Febrile convulsions
9.2.1.3
Absence seizures
Treatment Type of seizure
9.2.1.4
Grand mal seizures
9.2.1.5
Atonic (drop) seizures
Age
9.2.1.6
Complex partial seizures
9.2.1.7
Simple partial seizures
9.2.1.8
Nocturnal seizures
9.2.1.9
Lennox Gastaud syndrome
9.2.1.10 Other type of seizure 1 (describe)
[15]
Well controlled?
Well controlled?
9.2.1.11
Other type of seizure 2 (describe)
9.2.2
Some families have described a behavior which looks like an absence seizure but which does not produce an epileptic wave form on EEG. Please describe, including age of onset, if this applies to your child.
9.2.3
Has your child had any imaging or other investigations of the head or brain? (E.g. MRI, CAT or
EEG)
Yes No
9.2.3.1
If YES please describe
Age Type of scan Results
9.2.3.2
Would you be willing to share these scans with researchers?
9.3 Tonsils/adenoids and sleep apnoea
Yes No
[16]
9.3.1
Does/did your child have large tonsils? Yes No
9.3.2
Does/did your child have large adenoids? Yes
9.3.3
Has your child been diagnosed with sleep apnoea? Yes
No
No
9.3.4
If YES to any of the above please state at what age the diagnosis was made, any treatments, and the response to them.
9.4 Respiratory (breathing) conditions
Does/did your child suffer from:
9.4.1
Asthma
9.4.2
Hay Fever
9.4.3
Cystic Fibrosis
Age of Onset
9.4.4
Laryngomalacia
9.4.5
Tracheomalacia
Treatment Outcome
[17]
9.4.6
Other respiratory illness (describe)
9.4.7
Other respiratory illness (describe)
9.4.8
Has your child had any respiratory infections? Yes
9.4.8.1 If Yes
Age Type of Infection (if known)
No
Treatment (if any)
[18]
Response
9.4.8.2
Does your child still have respiratory infections? Yes No
9.4.8.2.1
If No , at what age did they cease to be a problem?
9.4.9
Has your child had any imaging or other investigations of the respiratory system? Yes
9.4.9.1
If YES please describe
Age Type of investigation Results
No
9.4.10
Has your child demonstrated: Breath holding/hyperventilating / Air swallowing / irregular breathing issues?
Yes No
[19]
9.4.10.1
If Yes, please describe including age, treatment (if any) and outcome
9.5 Kidneys, bladder and urinary system
Has your child been diagnosed with any of the following:
9.5.1 Renal cysts
9.5.1.1
If YES
Yes No
Age when diagnosed
9.5.2
Urinary Reflux
9.5.2.1
If YES
Age when diagnosed
Treatment (if any)
Treatment (if any)
Yes
9.5.3
Other kidney, bladder or urinary system disorder 1. (Specify):
9.5.3.1 Age when diagnosed Treatment (if any)
No
[20]
Outcome
Outcome
Outcome
9.5.4
Other kidney, bladder or urinary system disorder 2. (Specify):
9.5.4.1 Age when diagnosed Treatment (if any) Outcome
9.5.4.1
Age
9.5.4
Has your child had any infections of the kidneys, bladder or urinary system? Yes
If YES
Type of Infection Treatment
No
Response
9.5.5
Does your child still have kidney/bladder/urinary infections? Yes No
9.5.5.1
If No , at what age did they cease to be a problem?
9.5.6
Has your child had any imaging or other investigations of the kidneys, bladder or urinary system?
(e.g. for duplicate collecting systems of the kidneys) Yes No
9.5.6.1
If YES, please describe
Age Investigation Result Treatment (if any) Outcome
[21]
9.6 Stomach & Bowels
9.6.1
Has your child been diagnosed with a Hernia
If Yes,
9.6.1.1
Was the hernia: inguinal umbilical
9.6.1.2 Age Treatment (if any) Outcome
9.6.2
Has your child been diagnosed with Pyloric stenosis
9.6.2.1
If Yes,
Age Treatment (if any) Outcome
[22]
Yes No other (specify):
Yes No
9.6.3
Has your child been diagnosed with Duodenal atresia
9.6.3.1
If Yes,
Age Treatment (if any) Outcome
Yes No
9.6.4
Does/did your child have Anal Atresia / Imperforate Anus
(the normal opening of the anus is not present)
9.6.4.1
If Yes,
Age Treatment (if any) Outcome
Yes No
9.6.5
Has your child had any other gastrointestinal disorder (eg severe vomiting, reflux)?
9.6.5.1
If Yes,
Disorder Age Treatment (if any) Outcome
9.6.6
Has your child had any imaging or other investigations of the stomach or bowels?
9.6.6.1
If YES
[23]
Yes No
Yes No
Age Investigation Result Treatment (if any)
9.6.7
Does/has your child have/had a problem with constipation ?
9.6.7.1
If YES at what age did the problem begin?
9.6.7.2
Describe how constipation has effected your child
9.6.7.3
What treatments/therapy/surgery has been tried?
Age Treatment/therapy Outcome
[24]
Outcome
Yes No
9.6.8
Does/has your child have/had a problem with diarrhoea ?
9.6.8.1
If YES at what age did the problem begin?
9.6.8.2
Describe how diarrhoea has effected your child
Yes No
9.6.8.3
What treatments/therapy/surgery has been tried?
Age Treatment/therapy Outcome
9.6.9
Have you noticed a correlation between mood/behaviour and constipation/diarrhoea/other gut problems?
Yes No
9.6.9.1
If YES please describe
9.6.10
Has your child been diagnosed with bacterial overgrowth of the small intestines? Yes No
9.6.10.1
If YES, please describe including age when diagnosed
[25]
9.6.11
Has your child been diagnosed with any other stomach/bowel disorder?
If YES, please describe including age when diagnosed 9.6.11.1
9.7 Incontinence
9.7.1
Is your child potty/toilet trained? Yes No
9.7.1.1
If YES please state at what age this happened, and how this was accomplished
If NO is your child incontinent of
9.7.1.2.1
Urine only
Day time
9.7.1.2.2
Faeces only
Night time
[26]
Yes No
9.7.1.2.3
Both Urine & faeces
9.8 Genital area
9.8.1
Does your child have any unusual features in the genital area? Yes No
9.8.1.1
If YES what are they? (include undescended testicles in boys)
9.8.1.2
What treatment/therapy (if any) has been offered?
9.8.1.3
What was the outcome of any treatment/therapy?
9.9 Mouth and palate (roof of the mouth)
9.9.1
Does your child have a cleft (split) in the palate or the lip? Yes No
9.9.1.1
If NO, does your child have a high palate?
9.9.2
How has this affected 1. feeding?
Yes No
[27]
9.9.3
2. speech?
9.9.4
What treatment/therapy (if any) has been given?
Does your child have
9.9.5
Protruding tongue
9.9.6
Large tongue
Yes
Yes
No
No
9.9.7
Hard to understand speech Yes No
9.9.8 Any other problem of the mouth and palate excluding dental problems (see later) Yes No
9.9.8.1
If YES, please describe
9.10 Hands and feet, skin and nails
9.10.1 Hands (including fingernails)
9.10.1.1
Are your child’s fingernails unusual?
Yes No
9.10.1.1.1
If YES please describe (e.g. soft, brittle, thick, turning in, flaking, an unusual shape)
[28]
9.10.1.2
9.10.1.3
Does/did your child have fatty pads on his/her fingers or on other parts of his/her hands
Yes No
Does your child have a single palmar transverse crease (sometimes called a Simian crease) on the palms of his/her hands?
Yes No
9.10.1.4
Are your child’s hands unusual in any other way?
9.10.1.4.1
If Yes, please describe all unusual features
Yes No
9.10.2 Feet (including toenails)
9.10.2.1
Are your child’s toenails unusual?
Yes No
9.10.2.1.1
If YES please describe (e.g. soft, brittle, thick, turning in, flaking, an unusual shape)
9.10.2.2
Does/did your child suffer from flat feet (Pes planus, fallen arches)? Yes No
9.10.2.2.1
If YES what treatment /therapy has been used and how successful has it been?
9.10.2.3
Does/did your child wear orthotics, piedro boots or other specialist footwear? Yes No
9.10.2.3.1
If YES please describe
[29]
9.10.2.4
Does/did your child have fatty pads on his/her toes or on other parts of his/her feet ? Yes No
9.10.2.5
Are your child’s feet unusual in any other way?
Yes No
9.10.2.5.1
If Yes, please describe all unusual features
9.10.3 Skin
9.10.3.1
Does your child’s skin appear unusual in any way? Yes No
9.10.3.1.1
If YES please describe (e.g. very hairy, hairless, patches of lighter pigmentation, very dry, flaky, oily, psoriasis, eczema, prone to boils etc)
9.10.3.1.2
Have any special treatments/therapies been necessary? Yes No
9.10.3.1.2.1
If YES please describe the treatment/therapy and whether it was successful
9.11 Neuropsychiatric/behavioural disorders
9.11.1 Autism/Autistic tendencies
Has your child been diagnosed with
[30]
9.11.1.1
9.11.1.2
9.11.1.3
9.11.1.4
9.11.1.5
Autistic tendencies/Autistic Traits
Autism
ASD (Autism Spectrum Disorder)
PDDNOS (Pervasive Development Disorder Not Otherwise Specified)
Other similar disorder (please specify)
Yes
Yes
Yes
Yes
No
No
No
No
Does your child exhibit any of the following:
9.11.1.6
Sterotypies/stimming e.g. waving a hand in front of his/her face, running sand/beans/peas continually through his/her hands Yes No
9.11.1.7
Have a fascination with fans or other similar spinning objects.
Yes No
9.11.1.8
Lack of imaginative play with other children Yes No
9.11.1.9
Repeating mode where he/she will repeat a phrase/word/song/sound over and over
9.11.1.10
A heavy reliance on routines and structure Yes No
Yes No
9.11.1.11
Avoidance of looking directly at tasks/people Yes No
9.11.1.12
Sudden changes in lighting causing fear/behavioural problems Yes No
9.11.1.13
Phobias of / fascination with specific sounds e.g. telephone ringing Yes No
Yes No 9.11.1.14
Role play with self/talking/singing to self
9.11.1.15
Eye rolling upward Yes No
Yes No 9.11.1.16
Facial or vocal tics
9.11.1.17
Periods of unexplained staring
9.11.1.18
Difficulty coping with change
9.11.1.19
Echolalia (repeating back what you have said)
9.11.1.20
Echopraxia (copying your movements)
Yes
Yes
Yes
Yes
No
No
No
No
9.11.1.21
Walking around on tiptoes
9.11.1.22
Swapping between right and left handedness
Yes No
Yes No
[31]
9.11.1.23
Extremely passive behavior
9.11.1.24
Extremely active behavior
9.11.1.25
Dislike of certain textures
9.11.1.26
Does not seek cuddles and hugs
9.11.1.27
Repetitive behaviours
9.11.1.28
An eye for minute details
9.11.1.29
Preferring to play “in their own world”
9.11.1.30
Laughs inappropriately (e.g. when someone is hurt)
9.11.1.31
Appears not to listen to/ respond to the verbal word
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Yes
No
No
No
No
No
No
No
No
Yes No
9.11.2 Autistic catatonia
Often at or after the onset of puberty, some of the children/adults experience a severe neuropsychiatric disorder which has been described variously as autistic catatonia, chaotic behavior leading to severe apathy syndrome, rapid cycling bipolar disorder with catatonic episodes, post traumatic stress disorder, depression, mania, unspecified mood disorder, and complex dystonia.
Symptoms described often include periods of physical slowing up, difficulty completing even simple tasks which had previously not been a problem, freezing in unusual postures, catatonic/apathetic episodes, and periods of excited, mania like, driven behavior; and periods of extreme phobias/fear or anxiety. Dystonia and other movement disorders may occur, along with a loss of gained skills and an increase in autistic/stereotypical behaviours, repetitive speech (if any), echolalia, lack of eye contact, and some parkinsonian type episodes where EEGs and MRI’s are normal or show no structural changes from earlier scans.
If your child has experienced a severe neuropsychiatric or behavioural deterioration please describe it below
IN AS MUCH DETAIL AS POSSIBLE. (Note: While generally linked to the onset of puberty occasionally families have reported similar episodes triggered by either environmental insults or traumatic episodes such as bereavement.)
[32]
9.11.3 Amnesia
Has your child shown evidence of any periods of amnesia (e.g. not recognizing familiar people/places)
Yes No
9.11.3.1
If Yes, please describe
9.11.4 Other Behaviours
9.11.4.1
Describe your child’s behaviour on a “normal” day.
[33]
9.11.4.2
Describe your child’s behaviour on a “challenging” day.
9.11.4.3
Has your child exhibited any self injurious behavior (e.g. head banging, pulling own hair out, biting back of his/her hand) YES NO
9.11.4.3.1
If YES, please describe (including age and any treatment/therapy/intervention that helped)
If your child has demonstrated any of the following behaviours please describe (including age of onset):
9.11.4.4
Digging into/tearing nappies
9.11.4.5
9.11.4.6
ADD/ADHD (Attention Deficit (Hyperactivity) Disorder)
Biting others
[34]
9.11.4.7
9.11.4.8
Hair pulling of others
Tantrums
9.11.4.9
“Doing a Hulk, for no obvious reason”
9.11.4.10
Bouts of prolonged screaming
9.11.4.11
Throwing things / wrecking the house
9.11.4.12
Fear of lifts (elevators)
9.11.4.13
Other phobias and anxieties (please describe including age of onset, and when (if) resolved)
[35]
9.11.4.14
Does your child have any other behaviours you find difficult? (For example, other challenging behaviour, shyness, restlessness, passivity, inappropriate friendliness). YES NO
9.11.4.14.1
If Yes, please describe the behaviors, including age of onset:
9.11.4.15
Describe any management advice you have received for your child’s behaviours that proved helpful.
[36]
9.11.4.16
Describe any therapy you have received for your child’s behaviours that proved helpful.
9.11.4.17
Has your child been prescribed medication to help their behaviour?
9.11.4.17.1
If YES, please specify (including age, dosage and result)
YES NO
9.12 Issues of temperature regulation
Some families have mentioned the following issues in connection with temperature regulation, Please comment on any that relate to your child.
9.12.1
Tendency to get very high fevers
9.12.2
Febrile Convulsions
[37]
9.12.3
Cold hands/feet
9.12.4
Temperature variations (for different parts of the body)
9.12.5
Temperature regulation problems (can’t maintain a normal temperature)
9.12.6
Problems coping with cold
9.12.7
Problems coping with heat
9.12.8
Does not sweat normally
9.12.9
Other temperature related issue (please describe)
9.13 Blood related disorders
9.13.1
Has your child been diagnosed with any blood related disorders (including anemia)?
Yes
[38]
No
9.13.1.1
If Yes, please describe including name of disorder, age, treatments and outcomes
9.14 Cancer
9.14.1
Has your child been diagnosed with any cancer?
Yes
9.14.1.1
No
If Yes, please describe including type of cancer, age, treatments and outcomes
9,15 Endocrine & Metabolic systems
(Hormonal glands & chemical changes within the body)
9.15.1
Has your child been diagnosed with hypothyroidism ?
9.15.1.1
If Yes, please describe
Age Treatment
Yes No
Outcome
9.15.2
Has your child been diagnosed with hypoparathyroidism ?
Yes
9.15.2.1
If Yes, please describe
Age Treatment
No
Outcome
[39]
9.15.3
Has your child been diagnosed with any other disorder of the endocrine system?
Yes
9.15.3.1
If Yes, please describe including name of disorder, age, treatments and outcomes
9.15.4
Has your child been diagnosed with any metabolic disorder?
Yes No
If Yes, please describe including name of disorder, age, treatments and outcomes 9.15.4.1
9.16 Immune System
9.16.1
Has your child been diagnosed with any disorder of the immune system?
Yes
9.16.1.1
If Yes, please describe including name of disorder, age, treatments and outcomes
No
9.16.2 Immunology parameters
Has your child had blood tests to estimate levels of immunoglobulines, blood lymphocytes, complement factors, etc? Y es No
9.16.2.1
If Yes, please give results (including age of child for each blood test)
No
[40]
9.17 Orthopaedic disorders
9.17.1
Does your child have scoliosis (curvature of the spine)?
Yes
9.17.1.1
If Yes please give measurements and describe treatments
No
Age Measure of scoliosis (in degrees) Treatment/therapy (if any) and outcome
9.17.2
Does your child have lordosis (hollow back/saddle back/ swayback)?
Yes
9.17.2.1
If Yes please give measurements and describe treatments
No
Treatment/therapy (if any) and outcome Age Measure of lordosis
9.17.3
Does your child have kyphosis (hunchback/ hump back)?
Yes No
9.17.3.1
If Yes please give measurements and describe treatments
Age Measure of kyphosis Treatment/therapy (if any) and outcome
[41]
9.17.4
Does your child have any other orthopaedic disorders?
9.17.4.1
Yes
If Yes please describe, including age, treatment (if any) and outcomes
No
9.18 Connective tissue disorders and other musculature disorders
9.18.1
Does your child have joint laxity (looseness)? (E.g. they may be able to get into dislocated looking positions like a contortionist) Yes No
If Yes please describe including treatment received (if any) and any outcome 9.18.1.1
9.18.2
Does your child have joint contractures (tightness)? (E.g. they may be unable to move a limb because of tight or shortened muscles) Yes No
9.18.2.1
If Yes please describe including treatment received (if any) and any outcome
[42]
9.18.3
Does your child have any other disorder of his/her musculature/connective tissue?
9.18.3.1
If Yes please describe including treatment received (if any) and any outcome
9.19 Tolerance of pain/tears
9.19.1
How would you describe your child’s level of pain tolerance?
Low (i.e. feels pain very easily)
Normal
High (Can tolerate high levels of pain)
Don’t Know (e.g. because child cannot express feeling pain)
9.19.2
Does your child
Never cry tears
Rarely cry tears
Cry normal amounts of tears
Cry tears often
9.19.3
Other issues with pain tolerance or tears: (please describe)
9.20 Eyes and Vision
9.20.1
Is your child registered blind?
Yes No
9.20.1.1
If YES at what age were they diagnosed as blind?
Does/did your child have any of the following vision problems?
[43]
Yes No
Vision problem
9.20.2
a squint/cross eyed (strabismus) Yes
9.20.3
eyes not focusing properly Yes
9.20.4
eyes not moving together Yes
9.20.5
eyes not moving smoothly Yes
Yes 9.20.6
a slow blink rate
9.20.7
conjunctivitis Yes
9.20.8
long sightedness
9.20.9
short sightedness
9.20.10
Other vision problem (1)
(please describe)
Yes
Yes
9.20.11
Other vision problem (2)
(please describe)
9.20.12
Other vision problem (3)
(please describe)
[44]
No
No
No
No
No
No
No
No
Treatment (if any)
9.20.13
Does your child wear glasses?
Yes
9.20.13.1
If YES, at what age did (s)he start wearing glasses?
No
9.20.13.2
If YES, describe any approach that helped your child adjust to wearing glasses
9.21 Hearing
9.21.1
Has your child been diagnosed with a hearing impairment?
9.21.1.1
If Yes, is it
Yes No
Mild Moderate Severe
9.21.2
Describe any hearing problems your child has / had (such as glue ear, hearing loss) including age of onset.
9.21.3
How are any hearing problems managed? (e.g. hearing tubes (Grommets), hearing aids, special teaching)
[45]
9.21.4
Some parents have described how their children failed numerous distraction tests but their hearing tested normal after a brainstem test. Did this apply to your child? YES NO
9.22 Olfactory problems (Problems with sense of smell)
9.22.1
Has your child a problem with their sense of smell? Yes No
IF Yes
9.21.2
Please describe including age at diagnosis,and any treatments/therapies you have tried.
9.23 Sense of touch
9.23.1
Does your child have any problems with their sense of touch? (e.g. tactile defensiveness) Yes No
IF Yes
9.21.2
Please describe including age when noticed, and any treatments/therapies you have tried.
[46]
9.24 Teeth & Gums
9.24.1
Please use this space to tell us about your child’s dental development and any special treatment that has been necessary.
9.24.2 Bruxism (teeth grinding)
9.24.2.1
Does your child grind his/her teeth?
9.24.2.1.1
If YES is this teeth grinding while awake only
YES
YES
NO
NO
[47]
9.24.2.1.2
9.24.2.1.3 teeth grinding while asleep only teeth grinding while both awake and asleep
9.24.2.1.4
At what age did the teeth grinding begin?
9.24.2.1.5
Describe any treatments you have tried and their outcome.
YES
YES
NO
NO
10 Puberty
If your child has reached puberty, please describe it and say whether it proceeded as expected. Note any behavioural changes not already mentioned.
[48]
11.2
Thirties
11.3
Forties
11 Later Life:
If applicable note any changes that occurred as your child entered his/her
11.1
Twenties
[49]
11.4
Fifties
11.5
Sixties
12 Mobility & activity: gross motor skills
12.1 Milestones (please mark any that your child has achieved, stating the age in years & months when s/he achieved them)
Rolled Sat Crawled/shuffled Walked Walked alone
Climbed
stairs
12.2
How does your child move around indoors and outdoors? Mention sitting, rolling, crawling, walking, climbing stairs and any other activities
12.3
What treatment, if any, has your child needed for hypotonia (floppiness)?
[50]
12.4
What supports/aids (if any) has your child needed?
13 Hands, coordination and dexterity: fine motor skills
13.1
Describe any delays or difficulties, for example, in holding cutlery/ bottle/ toys
13.2
Describe any therapy/ aids/ special equipment used to help with fine motor skills
[51]
14 Other conditions
14.1
Has your child had any other medical conditions not already mentioned? Yes No
14.1.1
If yes, please say what they are, what treatment/therapy, if any, is being given and if it has been helpful.
Age Medical Condition Treatment/therapy Outcome
[52]
Age Medical Condition Treatment/therapy
15 General wellbeing
15.1
Tell us about your child’s general health and wellbeing.
[53]
Outcome
16 Energy levels
16.1
How would you describe your child’s energy levels when they are well?
Less than those of children of a similar age?
Similar to those of children of a similar age?
Greater than those of other children of a similar age?
16.2
Any other comments on energy levels?
17 Spending time in hospital
17.1
For what procedures/ illnesses has your child spent time in hospital?
Age Procedure/illness requiring hospitalization Duration of stay in hospital
[54]
18 Medicines
18.1 Drug/Supplement history
What medicines (if any) has your child taken in the past? Include any remedies that you buy without a doctor’s prescription.
Age Medicine/Remedy Reason for medicine/remedy Effect (if any)
[55]
Some parents have described negative/unusual reactions to some drugs/therapies by their child.
Unusual / unexpected reactions to drugs or therapies mentioned are listed below.
Anaesthetics – higher than normal dosage required
Muscle relaxants – no response or the opposite of the expected response
Negative reaction to droperidol
Poor reaction to abilify
Very agitated reaction to lorazepam
No reaction at all to diazepam
18.2 Please name any drugs/supplements or therapies that have caused a negative or unusual reaction in YOUR child, and state the age of the child, the dosage given and describe the reaction.
Age Name of drug/supplement/therapy Dosage Reaction
[56]
19 Other personal care
19.1
Can (s)he passively assist with personal care such as toileting? (i.e. not struggling against you)
Yes No
19.2
Can (s)he actively assist with personal care such as toileting? (e.g. by wiping his/her bottom)
Yes No
19.3
Can s/he wash, brush her/his teeth? Yes No
19.4
Can s/he dress him/herself?
19.5
Can s/he manage buttons?
19.6
Can s/he manage shoelaces?
19.7
How much help does s/he need during the day?
Yes No
Yes No
Yes No
[57]
19.8
How much help does s/he need during the night?
20 Communication
Does your child communicate in any of the following ways
Communicates with
20.1
Vocal sounds/noises YES NO
20.2
Eye contact
20.3
Facial Expressions
YES
YES
NO
NO
20.4
Touch
20.5
Laughing
20.6
Crying
20.7
Gestures
20.8
Signing
20.9
With symbols
20.10
With pictures
YES
YES
YES
YES
YES
YES
YES
NO
NO
NO
NO
NO
NO
NO
[58]
Example
20.11
With written words
20.12
With objects
YES
YES
20.13
With speech
20.14
Using body language
YES
YES
20.15
Using electronic equipment YES
20.16
Other way of communicating (describe)
NO
NO
NO
NO
NO
20.17
Describe any difference between what your child understands and what s/he can express
20.18
Does your child need a lot of processing time? Yes No Don’t know
If your child speaks
20.19.1
At what age (years, months) did s/he start?
20.19.2
What sort of speech or sentences does your child use? (e.g. single words, 2/3-word phrases)
20.19.3
Please give examples of what your child might say
[59]
20.19.4
What sounds of speech does your child find it difficult to make clearly?
Is your child’s speech likely to be understood by
20.19.5
No one except your child
Family 20.19.6
20.19.7
Others who meet your child often
20.19.8 Others who meets your child occasionally
Yes No
Yes No
Yes No
Yes No
Sometimes
Sometimes
Sometimes
Sometimes
20.19.9 Others who meets your child for the first time
20.20 Communication Issues
20.20.1
Do communication issues cause your child frustration?
Yes No
Don’t know
20.20.1.1
If Yes please describe
[60]
20.20.2
Has any form of therapy/intervention made a difference to the ability of your child to communicate?
Yes No
Don’t know
20.20.2.1
If Yes, please describe the therapy/intervention and how it helped.
21 Learning & Education
21.1
Does your child have any learning difficulty or intellectual disability?
(In some countries this is referred to as mental retardation) Yes No Unknown
21.1.1
If Yes, describe briefly (e.g. borderline, mild, moderate, severe, profound)
21.2
Describe your child’s overall level of achievement in different learning areas. Please also state your child’s strengths – e.g. great memory, love of music/singing, engaging personality.
[61]
21.3
What helps your child to learn most easily?
21.4
In terms of schooling, what is your child best at?
21.5
What (if anything) does your child read?
21.6
What (if anything) can your child draw or write?
21.7
Does your child have a statement of special educational need/ or equivalent? Yes No
21.7.1
If Yes, what (in summary) does it say?
[62]
21.8
What learning support does your child receive? (e.g. one to one assistance in school)
21.9 Please describe your child’s education to date
Type of school (e.g. special needs kindergarten) Age (from..to..) Outcome for your child
[63]
22 Play and sociability
22.1 Play
What are your child’s favourite activities? (For example: favourite toys, TV, dvds/videos, computers, music, playing with other people, pets, talking to themselves, singing, being in the company of familiar adults.
Please mention what age they were when the activity became a favourite.)
[64]
22.1.1
Could you describe how your child played at different ages?
Age Play (if any)
22.2 Sociability
How would you describe your child’s sociability?
22.2.1
With familiar adults
Too sociable Very Sociable Average Little sociability no interaction
22.2.2
With unfamiliar adults
22.2.3
With familiar children
22.2.4
With unfamiliar children
22.2.5
Have you noticed your child’s level of sociability change as (s)he gets older?
22.2.5.1
If Yes, please describe including what age any change occurred
YES NO
23 Sleep
23.1 Has your child had a sleep study done?
YES NO
23.1.1
If Yes, please describe the results, including the age of your child when the sleep study was undertaken.
[65]
23.2
Has your child had problems getting to sleep? YES NO
23.2.1
Describe your solutions (if any)
23.3
Has your child had problems staying asleep?
23.3.1
Describe your solutions (if any)
YES NO
23.4
Does your child suffer from sleep apnoea (periods where breathing stops during sleep)?
YES
23.5
Does/ did your child stretch/arch his/her neck back when sleeping?
23.6
Does/ did your child stretch/arch his/her neck back when awake?
23.7
Does/ did your child often sleep sitting up, folded forward?
23.8
Does/ did your child sleep in other unusual positions?
23.8.1
If YES, please describe
YES
YES
YES
YES
23.9
Is your child unable to achieve REM (Rapid eye movement/Dream) sleep? YES
23.10
Is your child unable to achieve deep sleep? YES
NO
NO
NO
NO
NO
NO
NO
[66]
23.11
Does/did your child take sleep medication?
23.11.1
IF YES, please specify
Age Dosage Sleep Medication
24 Specialness
24.1
Are there things that your child does that are special to you ?
YES
Outcome
NO
24.2 Your child helping you/others
How has s/he contributed most to your life, and to the lives of those who encounter him/her?
[67]
25 Services and interventions Describe the main interventions and therapies your child has received
Therapy Age Aim Outcome
25.1
Physiotherapy
25.2
Occupational
25.3
Speech therapy
25.4
Massage therapy
25.5
Play therapy
[68]
25.6
Music Therapy
25.7
Hippo therapy (horse therapy)
25.8
Hydrotherapy
Therapy Age Aim
25.9
Aromatherapy
25.10
Swim therapy
25.11
Reflexology
25.12
Vital Stim. Therapy
25.13
Craniosacral therapy
25.14
Osteopathy
[69]
Outcome
25.15
Chiropractic
25.16
ABA
(Applied Behaviour Analysis)
25.17
Hypobaric Oxygen therapy
25.18
Dolphin therapy
25.19
Ozone therapy
25.20
Urine therapy
25.21
Other therapy 1 (specify)
25.22
Other therapy 2 (specify)
[70]
25.23
Other therapy 3 (specify)
25.24
Other therapy 4 (specify)
26 Humour
26.1
How would you describe your child’s sense of humour? (E.g. some parents have mentioned that their child likes slapstick style humour like Laurel and Hardy, and really enjoy exaggerated facial expressions. Others have said their child has a “wicked” sense of humour and loves it when things go wrong, are spilled, make a mess etc.)
27 Siblings
27.1
Does your child have any siblings? Yes No
27.1.1
If YES, then how has having a brother/sister with the syndrome impacted on their lives?
[71]
27.1.2
If YES, then have you found any ways of helping siblings to cope?
28 Respite Care
28.1
Do you receive respite care for your child Yes No
28.1.1
If Yes, please describe the respite care, the age of the child when respite started and whether the respite was helpful to you and your family.
29 Accommodation
29.1
Does your child live in the family home? Yes No
29.1.1
If NO then please describe their type of accommodation and why you chose it (e.g. group home, sheltered dwelling, supported accommodation, psychiatric hospital, other institution)
[72]
29.1.2
At what age did they move to this accommodation?
29.1.3
What helped them to settle in their new accommodation?
30 Summary of studies performed for my child
Studies performed
30.1
MRI/ CT brain
30.2
EEG
Yes
Yes
No
No
30.3
Renal US Yes
30.4
Blood glucose or GTT (Glucose Tolerance Test) Yes
30.5
Other relevant investigations (specify)
No
30.6
Chromosome analysis
30.7
Array CGH study
30.8
Telomere FISH
Yes
Yes
Yes
Genetic workup (previous to diagnosis) to rule out
30.9.1
Angelman/PraderWilli syndrome Yes
30.9.2
SmithMagenis syndrome Yes
No
No
No
No
No
No
[73]
30.9.3
Rett syndrome
30.9.4
Down syndrome
30.9.5
Other syndrome 1 (specify):
30.9.6
Other syndrome 2 (specify):
30.9.7
Other syndrome 3 (specify):
30.9.8
Other syndrome 4 (specify):
30.9.9
Other syndrome 5 (specify):
Yes
Yes
No
No
31 Research
31.1
Have you ever been invited to take part in research related to your child’s chromosome disorder
Yes No
31.1.1 If YES, please write the name of the researcher/ hospital, institution
31.2
Would you consider taking part in (further) research into the syndrome? Yes No
32 Any other information you would like to include
(attach more pages, reports, studies, photographs, short video clips etc. as necessary, but only copies please –NO originals.)
[74]
[75]
Please send the completed questionnaire to:
b.foley1@ntlworld.com
or by post to
Brian Foley
50 Somerton Road
Belfast
Northern Ireland
BT15 3LG
Please only send COPIES not originals of any scans, test results, dvds, photos etc. that you may wish to include.
Thank you for taking the time to fill in the questionnaire.
[76]