vaginal fistula
advertisement

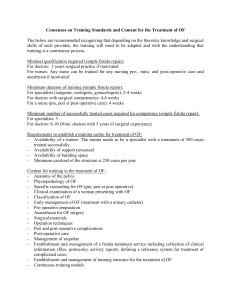
vaginal fistula A vaginal fistula is an abnormal, tortuous opening between the vagina and .)another hollow organ (see Figure 22-2 1 Pathophysiology and Etiology: Causes Obstetric injury, especially in long labors and in countries with inadequate obstetric care. Pelvic surgery ,hysterectomy or vaginal reconstructive procedures. Carcinoma extensive disease or complication of treatment such as radiation therapy. Pelvic radiotherapy - such as for pelvic cancer Types Vesicovaginal fistula is an opening between the bladder and vagina. Rectovaginal fistula is an opening between the rectum and vagina. Ureterovaginal fistula is an opening between the ureter and vagina. Urethrovaginal fistula is an opening between the urethra and vagina. Vaginoperineal fistula is an opening between the vagina and perineum. Clinical Manifestations 1.Vesicovaginal is the most common type of fistula Constant trickling of urine into vagina. Loss of urge to void because bladder is continuously emptying. May cause excoriation and inflammation of vulva. Watery vaginal discharge Constant leakage of urine from vagina 2. Rectovaginal. Fecal incontinence and flatus through the vagina; malodorous. May present as vulvar cancer. 3.Ureterovaginal fistula rare. 2 Urine leaking in vagina during urination but patient still voids regularly. May cause severe UTIs. 4.Urethrovaginal fistula. Dysuria. Urine in vagina on voiding. 5.Vaginoperineal fistula: pain and inflammation of perineum. Diagnostic Evaluation Methylene blue test after instillation of this dye in bladder. Methylene blue appears in vagina in vesicovaginal fistula . Methylene blue does not appear in vagina in ureterovaginal fistula Indigo carmine test after a methylene blue test shows negative results, indigo carmine is injected intravenously. If dye appears in vagina, this indicates ureterovaginal fistula I.V. urography helps detect presence and location of fistula, hydroureter, and hydronephrosis. Cystoscopy performed to determine number and location of fistula . Management Fistulas recognized at time of delivery should be corrected immediately. Treatment of postoperative fistula may be delayed for 2 to 3 months to allow treatment of infection. Surgical closure of opening via Vaginal or abdominal route (when patient's tissues are healthy). Fecal or urinary diversion procedure may be required for large fistula . Rarely, a fistula may heal without surgical intervention. Medical approach. Prosthesis to prevent incontinence and allow tissue to heal; done for patients who are not surgical candidates. 3 Prosthesis is inserted into vagina; it is connected to drainage tubing leading to a leg bag. Complications Hydronephrosis, pyelonephritis, and possible renal failure with ureterovaginal fistula Nursing Assessment Obtain obstetric, gynecologic, and surgical history. Monitor intake and output and voiding pattern. Assess drainage on perineal pads. Watch for signs of infection (fever, chills, flank pain). Nursing Diagnoses Risk for Infection related to contamination of urinary tract by flora or contamination of the vagina by rectal organism Impaired Urinary Elimination related to fistula Nursing Interventions Preventing Infection Encourage frequent sitz baths. Perform Vaginal irrigation as ordered, and teach patient the procedure. Before repair surgery, administer prescribed antibiotics to reduce pathogenic flora in the intestinal tract. After rectovaginal repair Maintain patient on clear liquids as prescribed to limit bowel activity for several days. Encourage rest because of debilitation. Administer warm perineal irrigations to decrease healing time and increase comfort. Maintaining Urinary Drainage 4 Suggest the use of perineal pads or incontinence products preoperatively. After vesicovaginal repair Maintain proper drainage from indwelling catheter to prevent pressure on newly sutured tissue. Administer Vaginal or bladder irrigations gently because of tenderness at operative site. Maintain strict intake and output records. If medical management is indicated, teach patient the use of prosthetic device. Encourage patient to express feelings about her altered route of elimination and share them with significant other. Patient Education and Health Maintenance Teach patient to report signs of infection early. Teach patient to clean perineum gently and to follow surgeon's instructions on when to resume sexual intercourse and strenuous activity. Advise patient to keep regular follow-up appointments. Evaluation: Expected Outcomes No signs of infection a febrile, no complaints of flank pain or difficulty voiding Clear urine flows from catheter postoperatively; voids without difficulty after catheter removal 5