Testosterone Deficiency and Supplementation for Women: What Do
advertisement

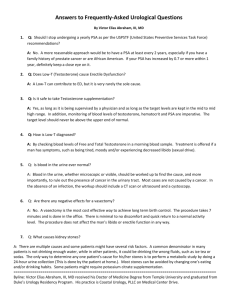
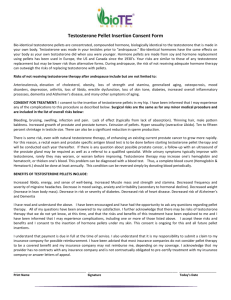
Testosterone Deficiency and Supplementation for Women: What Do We Need to Know Susan Rako, MD Testosterone: The Foundation for Sexual Function Each woman has her own particular adjustment to the sexual aspect of life, with her familiar rhythms of sexual feelings, fantasies, dreams, and activities. Life circumstances can certainly disrupt sexual rhythms, but the bottoming out of sexual desire that results from a critical reduction in testosterone is different from the fluctuations experienced with the various ups and downs of life and relationships. It has been postulated that “No matter how hard a woman might try to assemble the building blocks of healthy sexual functioning – the required amounts of other hormone, a loving partner, adequate stimulation, possibly a good sexual fantasy – it cannot work if she does not have the basic foundations of enough testosterone.” Gallup Survey Data Reflects Patitent/Physician Lack of Knowledge The results of a Gallup survey that was conducted by The North American Menopause Society (NAMS) and polled a random sample of 833 women between the ages of 45 and 60 on women’s knowledge, Information sources, and attitudes to menopause and hormone replacement therapy (HRT) demonstrated that “the majority of women have heard about estrogen and progestins, with only a minority reflecting knowledge about androgens.” This research concluded that “these data may reflect lack of physician knowledge or information about androgen and another area for improved provider and consumer education.” Androgens, rather than estrogens, are responsible for sexual desire in the human female Only 5% of the women polled knew that their bodies make “androgens” and that production of these hormones declines after menopause. Today, increasing numbers of peri- and postmenopausal women (many of whom have had a surgical or chemical menopause) are approaching their healthcare providers with questions about testosterone deficiency and supplementation. The Role of Testosterone in Female Physiology Testosterone plays a vial role in the normal physiology of women. In girls, as well as boys, it is testosterone that triggers the events of puberty. The adolescent girls’ growth of pubic and of axillary hair, the heightened sexual sensitivity in nipples and genitals, and the increased susceptibility to psychosexual stimulation(sexual libido) are all generated by a surge of testosterone at adrenarche ( the markedly increased production of adrenal cortical androgens that occurs at puberty). Groundbreaking research published in 1959 made use of clinical observations of women with advanced breast cancer whose ovaries and adrenal glands had Been removed in the hope of slowing progress of the disease. This research concluded that androgens, rather than estrogens, are responsible for sexual desire in the human female. Two years later, another research study emphasized that “androgen is the libido hormone in both men and women’ and that estrogen was “necessary to abolish vaginal dryness and tenderness and so expedite coitus” – but the androgen was found to increase the sensitivity of the genitals, especially the clitoris, as well as the heighten desire and increase sexual gratification. Other Effects Testosterone, an anabolic steroid and the most potent of the androgens, promotes metabolic efficiency, the physiologic basis for the maintenance of “vital energy”. It has been stated that “testosterone and other androgens have some biological activity on virtually every tissue in the body. Symptoms and Signs of Testosterone Deficiency ……………………………. 1. Global loss of sexual desire: lack of sexual fantasy and sexual dreams. 2. Decreased sensitivity to sexual stimilation in the nipples and in the clitoris. 3. Decreased arousability and capacity for orgasm. 4. Diminished vital energy and sense of well-being. 5. Loss of muscle tone. And in Women 6. Thinning and loss of pubic hair. 7. Genital atrophy not responsive to estrogen. 8. Dry and brittle scalp hair; dry skin. Testosterone and Bone Density Recent research has shown that testosterone contributes substantially to bone density, as well as to muscle tone. Results of a two-year investigation that compared the effects of oral estrogens (1.25 mg of conjugates estrogens) and a combination estrogen/methyltestosterone preparation (2.5 mg of methyltestosterone and 1.25 mg of conjugated estrogens) on menopausal symptoms, lipidlipoprotein profiles, and bone density in surgically menopausal women were published in 1995. This study confirmed the effectiveness of testosterone on menopausal symptoms and demonstrated that the oral combination not only prevented hone loss – as did estrogens alone – but also produced significant increases in spinal hone mineral density – an effect not produced by estrogens alone. Testosterone Production in Women On the average, premenopausal females produce .3 mg of testosterone per day. With the establishment of the menstrual cycle, the hormone primarily produced by the ovaried is androstenedione, most of which is then converted to testosterone and subsequently aromatized to estadiol. However, not all of the ovarian testosterone becomes estradiol. Enough testosterone remains unconverted to amount to 25% of a woman’s daily testosterone production, another 25% is produced by the adrenal cortex, and the remaining 50% by peripheral tissues (including the liver, the skin, and the brain) from precursors produced in the ovaries and the adrenals. In other words, the ovaries and the adrenal glands produce all of a woman’s testosterone – directly or indirectly. Testosterone in the Blood Most of the circulating testosterone (97-99%) is carried in the blood bound to sex hormone binding globulin (SHBG). Only unbound or “free testosterone (1%-3% of the total) can attach to cellular receptors to produce effects on tissues. If a woman is not using supplementary methyltestosterone, accurate values for both total and free testosterone can be obtained when measuring testosterone blood levels. Available assays for total for testosterone are confounded by the presence of methyltestosterone, although the assay for free testosterone are confounded by the assay for free testosterone can be used as an indicator to gauge the serum level of testosterone attained at a given supplemental dosage of methyltestosterone. Sensitivity to testosterone is a variable phenomenon – function of the levels and thresholds for activity of testosterone receptors, which are in turn influenced by estrogen levels. The adequacy of a particular blood level of testosterone can differ from woman to woman. A woman presenting with the clinical symptoms and signs of testosterone deficiency and whose blood levels of total and free testosterone are measured to be in the lower part of the “normal” range may actually be testosterone deficient and will benefit from appropriate supplementation. In this regard, it is preferable to “treat the patient, and not the number.” Physiological Levels of Serum Testosterone in Women Total Testosterone 25 – 70 ng/dl Free Testosterone 0.7 – 2.0 pg/ml Menopause, Adrenopause, and Testosterone Deficiency The postmenopausal ovary produces not only markedly lower amounts of estrogens, but substantially lower amounts of testosterone in 50% of women. Several years before most women reach menopause (by 40-44) adrenal androgen production has already decreased by more than half. Since the function of the adrenal cortex appears to be linked to the function of the ovary, a woman needs fully functioning ovaries in order to maintain fully functioning ovaries in order to maintain fully functioning adrenals. This fascinating fact may be related to an embryological phenomenon: one original group of cells is the source for both the ovaries (or testes) and for the adrenal cortices. In other words, in the developing embryo, cells migrate from one original group – some to form the gonads, and others to form the adrenal cortices. Following menopause women lose not only a significant Portion of their ovarian estrogen and testosterone, but also a significant portion of their adrenal androgens, including testosterone It was long been observed that adrenal cortical hormone production (including testosterone) falls off more quickly in women than in men. This may be due to the fact that, on average, the testes remain functional for decades longer than the ovaries. The consequence of the connection between ovarian function and adrenal function is that, following menopause; women lose not only a significant portion of their ovarian estrogen and testosterone, but also a significant portion of their adrenal androgens, including testosterone. In some naturally menopausal women, testosterone production may decrease to the point where it is unmeasurbale; signs and symptoms of testosterone deficiency can develop for these women even during their perimenopause. More commonly, testosterone deficiency develops during the several years following natural menopause. Since estrogen has the effect of stimulating the production of SHBG (which will bind up more of whatever available testosterone a woman may be producing), when a woman takes estrogen supplemental therapy, she may be tipped into testosterone deficiency – with loss of libido, energy, and other symptoms. Early publications on the role of testosterone in female physiology described menopause as “a catabolic stat.” To maintain healthy tissue and as healthy a metabolic balance as aging allows, for many menopausal women HRT means: Supplementary estrogen, Progestin (if needed to protect against endometrial hyperplasia), and Testosterone Hysterectomy and Testosterone Deficiency In 1993, the most recent year for which statistics are available, 561,000 hysterectomies were performed in the U.S. Today more than 30% of American women have had a hysterectomy – most often before the age of 50. The Gallup survey conducted by NAMS yielded the statistic that of the 833 women polled, 37.5% had a hysterectomy. Even though one or both ovaries may be spared at the time of surgery, ovarian failure (postulated to be a consequence of interruption of the blood supply formerly provided by the uterine artery) follows hysterectomy in a significant number of cases. Within a few days to a few weeks of the surgery, women whose ovaries have been surgically removed or compromised can develop dramatic symptoms both of estrogen and testosterone deficiency. Supplementary estrogen, which is often prescribed, cannot help the symptoms of loss of sexual libido and response, lack of general energy, and diminished sense of well-being that are the consequence of the testosterone deficiency that approximately half of these women develop. Studies have demonstrated that women who had undergone surgical menopause and were treated both with supplemental estrogen and testosterone achieved an optimal balance of sexual energy and wellbeing, as compared with women given wither no hormones or estrogen alone. At a time when they may be enjoying their sexual and vial energies to the fullest, women who undergo hysterectomy in their 30s and early 40s (and occasionally, even in their 20s) are particularly unprepared for the aggrieved by these losses. Too often the diagnosis of testosterone deficiency is missed, and many women reporting loss of libido and energy are prescribed antidepressants or referred for counseling; however, what they actually need it supplementary testosterone. Chemical Menopause and Testosterone Deficiency The 1992 publication of: “A Neglected Issue: The Sexual Side Effects of Current Treatments for Breast Cancer” addressed the fact that women who have lost ovarian function secondary to chemotherapy for cancer develop testosterone deficiency. Symptoms include: Global loss of sexual desire Diminished sexual pleasure and fantasy Decline of clitoral sensations and Markedly diminished orgastic response. Similar to the population of women suffering the hormonal consequences of surgical menopause, a significant number of women who become testosterone deficient following chemotherapy are in their 30s and 40s. On the basis of the available data with regard to estrogen supplemental therapy for women who have had breast cancer, increasing numbers of oncologists believe that the benefits outweigh the risks. While there is controversy among oncologists with regard to the prudence of testosterone replacement for women with breast cancer, the publication noted that some oncologists “do not hesitate to prescribe the low does of testosterone that are libido restorative,” particularly in t he face of the results of several studies that suggest that “androgens may actually be indicated and therapeutic for patients with this neoplasm.” Even though they know that definitive research data is not available, chemically menopausal women can be so distressed by their symptoms of testosterone deficiency and compromised quality of life that they choose to take prudently prescribed supplementary testosterone. To improve the quality of the life they have remaining, some women whose cancer has already metastasized elect to take supplementary testosterone both for sexual and general energy enhancement. A prudent goal of supplemental testosterone therapy is the concept of keeping blood levels within a physiological range Of all available supplemental testosterone preparations, methyltestosterone alone doesn’t readily aromatize to estradiol; therefore, this may be the preferred supplement for women for whom it seems prudent to keep estrogen levels as low as possible. Testosterone Supplementation Dozens of articles have been published in the medical archives documenting and attesting to the effectiveness of testosterone supplemental therapy in restoring sexual libido and in relieving the other symptoms of testosterone deficiency in women. Symptoms of testosterone deficiency are not clinically subtle; however, some women are uncomfortable about initiating discussions about their problems. The most help physician is one who inquires about changes in sexual libido, energy, sense of well-being, and who helps a woman evaluate her particular risk/benefit factors among the options available for treatment. Recognizing the cardioprotective, bone saving, and other benefits of adequate estrogen supplementation, a decision about the risks/benefits of estrogen (with adequate progestion for women with an intact uterus) as a foundation for subsequent testosterone supplementation makes good clinical sense. If a woman has already been using estrogen – and, if indicated, adequate progestin – testosterone supplement can be added to her established hormonal regimen. A prudent goal for supplemental testosterone therapy is the concept of keeping blood levels within a physiological range. Clinical experience has shown the effective range of oral dosage to be .25 mg to .8 mg of methyltestosterone per day, with most women benefiting from .3 mg to .6 mg. Prescriptions for flexible, low enough dosing of oral methyltestosterone must he compounded to order. Methyltestosterone and Liver Function Warnings about the potential hepatotoxicity of oral methyltestosterone have been based on case reports in which the daily oral dosage ranged from 20 mg to 150 mg – dosages hugely in excess of any recommended as supplemental for women. A recent two-year study of women receiving 2.5 mg of oral methyltestosterone (three to ten times the recommended dose range of .25 mg to .8 mg) revealed no clinically significant changes in liver function tests. For women taking the recommended dose of supplemental methyltestosterone, a thoroughly prudent course would be to monitor liver function annually. To Avoid Virilizing Side Effects The possibility of undesirable side effects is naturally a major concern of women deciding about supplemental testosterone. Testosterone supplementation within the physiological range (.25 mg to .8 mg per day) does not produce Virilizing side effects. Only excessive, long-term dosage may result in the development of Virilizing side effects – acne, increased downy facial hair, and (in extreme cases) lowered voice. I have discovered that there is a sensitive” window” of dosage that works best for a particular woman at a particular time. This dose may change – as may the dose of estrogen supplement functions continue to diminish over the decade following menopause. If a woman takes more testosterone than needed, she will not experience stronger stimulation of libido, but will more likely experience irritability – a signal to reduce the dose. Topical Testosterone Because testosterone deficiency can result in genital atrophy (even for women who have been using supplementary estrogen), women who begin supplementing with oral methyltestosterone may sometimes receive benefits to energy and sense of well being without significant improvement in genital sensation and libido. I have discovered that testosterone deficient women sometimes require a once/daily application to the genital mucosa of a small amount of topical testosterone (1%-2%) for an initial few weeks. When the tissue becomes healthy and local testosterone receptors have been well supplied, sensation and libido return. Topical testosterone is very well absorbed by healthy genital tissue and can potentially result in high blood levels – above the physiological range. Intermittent monitoring of testosterone levels will allow for modification of concentration or dose schedule. Once libido has improved and capacity for genital stimulation has been established, a shift to an oral supplement will usually maintain an adequate effect on the genitals. Another caution against longterm daily use of topical testosterone on the genital mucosa is the potential for local overstimulation and gradual clitoral enlargement – both reversible on discontinuation of topical testosterone. Should this ensue, a change to physiological oral dosage is advisable and effective. Testosterone supplementation within the physiological range (.25 mg to .8 mg per day) does not produce Virilizing side effects Testosterone and Cardiovascular Risk Factors predicting increased cardiovascular risk in menopausal women (those not receiving supplemental estrogen or testosterone) include: Increased serum levels of cholesterol, Decreased high-density lipoprotein (HDL) cholesterol, and Increased low-density lipoprotein (LGL) cholesterol. Estrogen therapy counteracts some changes by: Increasing HDL cholesterol, and Decreasing total and LDL cholesterol. However, only 25%-50% of the cardioprotective effects of estrogen are attributable to its effects on the lipid profile; 50%75% of the benefits of estrogen are due to effects on coagulation parameters, vasodilatation, and carbohydrate metabolism. Adding testosterone to estrogen supplemental therapy has been shown to: Reduce total cholesterol Reduce LDL cholesterol, Reduce triglycerides, and also Reduce HDL cholesterol. The three year Postmenopausal Estrogen and Progestin Intervention ural micronized progesterone in an oil suspension did not interfere with the beneficial effects of estrogen on HDL cholesterol levels, as compared with the effects of the use of synthetic progestins. As with formulations for testosterone supplements, formulations of natural micronized progesterone in oil are available only by prescription compounded to order by one of the 1, 500 compounding pharmacies in the U.S. Depending upon patient history for cardiovascular risk factors and lipid profile changes with aging, it appears prudent to monitor serum lipids for women who need and choose to take supplementary testosterone, and to emphasize the need for reasonable diet and healthy exercise. Focus for Further Research For more definitive answers to cardiac and cancer risk/benefits, testosterone supplemental therapy must be included in longer-term research protocols. Shorter- term studies to confirm lowest effective dosage range, comparative effects of routes of delivery, and epidemiologic data are also pressing for attention. As a recent review of the role of androgens in women’s health concluded: “Future research should be aimed at identifying those women who have not undergone surgical or medical castration but have decreased functional androgenic activity… Androgen replacement therapy is a neglected area of medical practice and further research is needed to identify all women who will benefit from it” Susan Rako, MD, is a Boston psychiatrist in private practice and a consultant and lecturer on the subject of testosterone deficiency and supplementation for women. She is also the author of The Hormone of Desire: The Truth About Menopause, Sexuality, and Testosterone. References: 1. Kaplan HS, Barlik B. In: Rako S, ed. The Hormone of Desire. New York, NF: Harmony Books; 1996;13. Introduction. 2. Utian WH,Schiff I. NAMSGallup survey on women’s knowledge, information sources, and attitudes to menopause and hormone replacement therapy. Menopause 1994; 1(1): 39 3. Beas F, Zurbrugg RP, Cara J, Gardner LI. Urinary Cl steroids in normal children and adults. J Clin Endocrinol Metab 1962;22:1090. 4. Money J. Componenets of eroticism in man: I. The horomones in relation to sexual morphology and sexual desire. J Nervous and Mental Diseases 1961;132:239. 5. Waxenberg SE, Drellich MG, Sutherland AM. The role of hormones in human behavior:I. Changes in female sexuality after adrenalectomy. J Clin Endocrinol 1959;19:193. 6. Veldhuis J. The hypothalamicpituitary-testicular axis. In: Yen SSC, Jaffe RB, eds. Reproductive Endoctinology. 3rd ed. Philadelphia, PA: WB Saunders Co;1991:409. 7. Davis SR, McCloud P, Straus BJG, Burger H. Testosterone enhances estradiol’s effects on postmenopausal hone density and sexuality. Maturitas 1995;21:227. 8. Jassal SK, Barrett-Connor E, Edelstein SL. Low bioavailable testosterone levels predict future height loss in postmenopausal women. J Hone and Mineral Research 1995;10(4):650. 9. Watts NB, Notelovitz M, Timmons MC, et al. Comparison of oral estrogens and estrogens plus androgen on bone mineral density, menopausal symptoms, and lipid-lipoprotein progiles in surgical menopause. Obstet Gynecol 1995;85(4):529. 10. O’Malley BW, Strott CA. Steriod hormones:Metabloism and mechanism of action. In:Yen SSC, Jaffe RB, eds. Reproductive Endocrinology. 3rd ed. Philadelphia, PA: WB Saunders Co;1991:156. 11. Adashi EY. The ovarian life cycle. In: Yen SSC, Jaffe RB, eds. Reproductive Endocrinology. 3rd ed. Philadelphia, PA: WB Saunders Co; 1991:181. 12. Yen SSC. Chronic anovulation caused by peripheral endocrine disorders. In:Yen SSC, Jaffe RB, eds. Reproductive Endocrinology. 3rd ed. Philadelphia, PA: WB Saunders Co; 1991:576. 13. Longcope C, Hunter R, Franz C. Steroid secretion by the postmenopausal ovary. Am J Obstet Gynecol 1980;138:564. 14.Orentreich N, Brind JL, Rizer RL, Vogelman JH. Age changes and sex difference in serum dehydroepiandrosterone sulfate concentration throughout adulthood. J Clin Endocrinol Metab 1984;59(3):551. 15.Cumming DC, Rebar RW, Hopper Br, Yen SSC. Evidence for an influence of the ovary on circulation dehydroepiandrosterone sulfate levels. J Clin Endocrinol Metab 1982;54(5):1069. 16. Greenblatt RB. Androgenic therapy in women. J Clin Endocrinol Metab 1942;2:665. Communications To The Editors. 17. Greenblatt RB. The use of androgens in the menopause and other gynecic disorders. Obstet Gynecol Clin of North Am 1987;14(1):251. 18. National Center for Health Statistics, National Institutes of Health, Bethesda, Maryland. Most recent data available as quoted on June 17, 1996. 19. McCoy NL. The menopause and sexuality. In sitruk-Ware R, Utian Wh eds. The Menopause and Hormone Replacement Therapy. New York, NF:Marcel Dekker, Inc;1991:73. 20. Ridel H, LehmannWillenbrock E, SemmK. Ovarian failure phenomena after hysterectomy. J Repro Med 1986;31(7):597. 21. Chakravarti S, Collins WP, Newton JR, et al. Endocrine changes and symptomatology after oophorectomy in premenopausal women. Br J Obstet Gynaecol 1977;84:769. 22. Sherwin BB, Gelfand MM. Sex steroids and affect in the surgical menopause: A doubleblind, cross-over study. Psychoneuroendocrinology 1985;10(3):325. 23.SherwinBB, Gelfand MM, Brender W. Androgen enhances sexual motivation in females: A prospective, crossover study of sex steroid administration in the surgical menopause.Psychosomatic Med 1985;47(4):339. 24. Sherwin BB, Gelfand MM. Differential symptom response to parenteral estrogen and/or androgen administration in the surgical menopause. Am J Obstet Gynecol 1985;151(2):153. 25. Sherwin BB, Gelfand MM. The role of androgen in the maintenance of sexual functioning in oophorectomized women. Psychosomatic Med 1987;49:379. 26. Sherwin BB. Affective changes with estrogen and androgen replacement therapy in surgically menopausal women. J affective Disorders 1988;14:177. 27. Kaplan HS.A neglected issue: the sexual side effects of current treatments for breast cancer. J sex and Marital Therapy 1992;18(1):3. 28. American College of Obstetricians and Gynecologists Committee Opinion. Estrogen replacement therapy in women with previously treated brease cancer. 1994;(135). 29. Sands R, Boshoff C, JonesA, Studd J. Current opinion: Hormone replacement therapy after a diagnosis of breast cance. Menopause 1995 ; 2(2):73 30. Karyads I, Fetiman IS, Tong D, et al. Adjuvant androgen treatment of operable breast cancer – a 20 year analysis. Eur J of Surg Oncol 1987;13;113. 31.Poulin R, Baker D, Labrie F. Androgens inhibit basal and estrogen-induced cell proliferation in the ZR-75-1 human breast cancer cell line. Breast Cancer Research and Treatment 1988;12:213. 32.Salmon UJ, Geist SH. Effect of androgens upon libido in women. J Clin endocrinol 1943;3:235. 33. Bachman GA. Estrogenandrogens therapy for sexual and emotional well-being. The Female Patient 1993;18:15. 34.Cardozo L, Gibb DMF, Tuck SM, et al. The effects of subcutaneous hormone implants during the climacteric. Maturitas 1984;5:177. 35.Greenblatt RB. Hormone factors in libido. J Clin Endocrinol 1943;5:305. Editorials. 36. Greenblatt RB, Barfield WE, Garner JF, et al. Evaluation of an estrogen, androgen, estrogenandrogen combination, and a placebo in the treatment of the menopause. J Clin Endocrinol 1950;2(11):1547. 37. Greenblatt RB, Chaddha JS, Teran AZ, Bezhat CH.Aphrodisiacs. In: Iversom SD, ed. Psychopharmacology: Recent Advances and Future Prospects. New York, NY: Oxford University Press;1985:289. 38. Persky H, Charney N, Lief HI, et al. The relationship of plasma estradiol level to sexual behavior in young women. Psychosomatic Med 1978;40(7):523. 39. Sands R, Studd J. Exogenous androgens in postmenopausal women. Am J Med 1995;98(suppl 1A):76S. 40. Sherwin, BB. Menopause: Myths and realities. In: Stewart CE, Stotland NL, Eds. Motherhood and Mental Illness(2):Causes and Consequences. Washington, DC: American Psychiatric Press, Inc;1993:227. 41. Studd JWW, Collins WP, Chakravarti S, et al. Oestradiol and testosterone implants in the treatment of psychosexual problems in the post-menopausal woman. Brit J obstet Gynaecol 1977;84:314. 42. Young RL Androgens in postmenopausal therapy. Menopause Management 1993;2(5):21. 43.Rako S. The Hormone Desire. New York, NY: Harmony Books;1996. 44. Personal communication with Edward Klaiber, MD, July 1996. 45. Brick IB, Kyle LH. Jaundice of hepatic origin during the course of methyl-testosterone therapy. N Engl J Med 1952;246(5):176. 46. Cocks JR. Methyltestosterone-induced liver-cell tumours. Med J Aust 1981;2:617. 47. Westaby D, Ogle SJ, Paradinas FJ,et al. Liver damage from long-term methyltesosterone.Lancet 1977;ii:261. 48. Gorodeski, GI. The effects of ERT/Hrt on CVD. Menopause Management 1995;4(3):10. 49. Barrett-Connor E, Bush TL Estrogen and coronary heart disease in women. JAMA 1991;265(14):1861. 50. Writing Group for the PEPI Trial. Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women: The postmenopausal estrogen/progestin interventions (PEPI)trial. JAMA 1995;273(3):199.