Journal Club Jim Hoehns, Pharm.D. What Adverse Effects Are
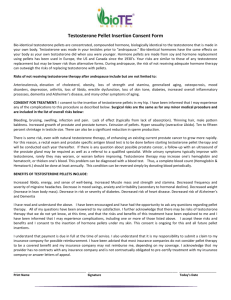
advertisement

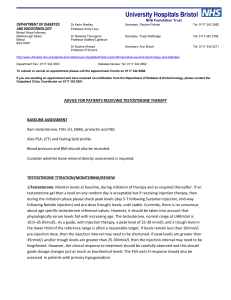
CV: DVT, edema, HTN, vasodilation CNS: aggression, depression, insomnia, anxiety, sleep apnea, memory loss, mood swings Endo: breast pain, gynecomastia, hyperlipidemia, libido change GI: nausea, weight gain, increased appetite GU: priapism, impotence, PSA increased, BPH, impaired urination, testicular atrophy Hepatic: cholestatic jaundice Heme: anemia, bleeding, polycythemia, suppression of clotting factors, Hgb/Hct increased Other: creatinine increased Men have gradual declines in average testosterone as they age Testosterone therapy prescribed for 2.9% of men aged ≥40 years No equivalent of Women’s Health Initiative for men Inadequate information of effect of testosterone replacement on clinical outcomes One recent study of T replacement in older frail men was stopped prematurely due to CV events N Engl J Med 2010;363:109-22. JAMA 2013;310:1829-36. Retrospective national cohort (VA system) 76 VA cath labs Patients Male patients with angiography (2005-2011), had subsequent [testosterone] checked, and had value <300 ng/mL Study comparison: Those that started testosterone Rx vs. those who did not CAD: ≥20% stenosis in epicardial vessel Exclusion criteria Started testosterone before angiography Missing data on coronary anatomy Prescribed testosterone after an MI Hct >50% PSA of 4.0 ng/mL or higher Follow-up Mean: 27.5 months Covariates Weighted adjustment ▪ Age, race, prior MI, CHF, diabetes, renal failure, MDD, PTSD, hyperlipidemia, PAD, COPD, OSA, HTN, cerebrovascular disease, overweight, dialysis, ever smoker, alcohol, anemia, drug abuse, electrolyte abnormalities, AIDS, hypothyroidism, liver disease, lymphoma, cancer, neurological disorder, PUD, RA, and procedures: prior CABG, revascularization, transplant, cardiac MRI, echocardiogram, TEE Primary exposure variable Initiated Rx for testosterone gel, injection, or patch ▪ ?once initiated, assumed to have continued until event or end of follow-up Primary endpoint Time to all-cause mortality or hospitalization for MI or stroke ▪ Obtained from VA inpatient files (ICD-9) ▪ Last day of follow-up: 1/23/12 Statistics Treated testosterone as a time varying covariate Tested for interaction between CAD status and testosterone therapy Statistics (cont.): Separated testosterone exposure ▪ Injections, patch, or gel Sensitivity analyses ▪ Evaluated if results due to differential treatment of CV risk factors ▪ LDL, BP, statin use, beta-blocker use ▪ Included subsequent PCI/CABG as additional outcome ▪ Assessed dose of T prescribed and duration of treatment ▪ Gel (1.1%), injections (35.7%), and patches (63.3%) Group Died MI Stroke No testosterone (N=7,486) 9.1% 5.6% 6.5% Testosterone (N=1,223) 5.4% 1.8% 2.6% Group 1 Year† 2 Years 3 Years No testosterone 10.1% 15.4% 19.9% Testosterone 11.3%* 18.5% 25.7% Abolute Risk Difference 1.3% (-7.1% to 3.1% (-4.9% to 5.8% (-1.4% to 9.7%) 11.0%) 13.1%) † years after coronary angiography * Kaplan-Meier estimated cumulative percentages Same elevated risk observed in patients in those with and without CAD Test for interaction, P=0.41 No difference in risk among types of T replacement T values 60% of those prescribed T had another [T] checked Among them, T increased from mean of 176 ng/dL to 332 ng/dL Potential explanations for results T may increase platelet aggregation T may increase vascular inflammation T may worsen breathing in patients with OSA First observational study to suggest that testosterone is associated with adverse cardiovascular outcomes Unmeasured confounders may exist Outcomes not validated by chart review Used ICD-9 codes Small number of patients with extended follow-up time Uncertain generalizability Sizable burden of comorbidities Poor characterization of testosterone usage from pharmacy claims Uncertain how to rectify the statistics Weighting of comorbidities Complex methodology I am uncertain of validity of this method to adjust for unmeasured confounders Unclear what individual components of composite outcome were driving observed differences in their model Use of testosterone was associated with increased risk of mortality, MI, or ischemic stroke Association was not modified by presence or absence of CAD