24.Surgical diseases of the SPLEEN
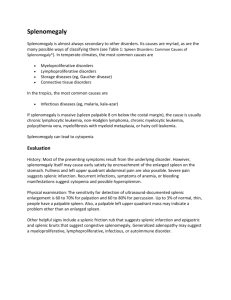
advertisement

THE KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF SURGICAL DISEASES № 1 SURGICAL DISEASES OF THE SPLEEN Information for self-training of English-speaking students The chair of surgical diseases N 1 (Chair-head - prof. S.V.Ivanov) BY ASS. PROFESSOR I.S. IVANOV KURSK-2010 THE SPLEEN ANATOMY Embryonic development of the spleen begins in the fifth week of gestation as a small cluster of mesenchymal cells in the dorsal mesogastrium between the stomach and pancreas. Mesenchymal remnants that do not fuse with the main splenic mass account for the high incidence (15%–30%) of accessory spleens in adjacent tissues. The spleen is the second largest organ of the reticuloendothelial system. It is located in the posterior left upper quadrant of the abdomen where its relationships to the diaphragm, stomach, pancreas, left kidney, and splenic flexure of the colon are maintained by suspensory ligaments. The splenophrenic, splenorenal, and splenocolic ligaments are usually relatively avascular, except in patients with portal hypertension, and their transection allows the spleen to be displaced medially and anteriorly. The gastrosplenic ligament, which extends from the greater curvature of the body and fundus of the stomach to the spleen, contains the short gastric arteries and veins. Located in the most medial aspect of the splenorenal ligament and attached to the spleen at the hilum, the splenic pedicle contains the splenic artery and vein, lymphatic structures, and often the tail of the pancreas . The arterial supply to the spleen is derived from the celiac artery from both the splenic artery and the short gastric arteries, which usually arise as branches of the gastroepiploic or the splenic arteries . The splenic vein is formed by a coalescence of polar veins in the splenic hilum and courses with the splenic artery along the dorsal surface of the pancreas to enter the portal system. The normal adult spleen is a slightly concave, solid, dark red organ that measures approximately 3 × 8 × 14 cm., weighs between 100 and 175 gm., and frequently has fetal lobulations on its anterior edge. A thin peritoneal capsule encloses the deeper organ pulp and easily strips from it. In elderly individuals or in those with prior splenic injury, irradiation, or recurrent infarction, the splenic capsule may become firm and thickly scarred (“sugar coated”) and adherent to the diaphragm. A trabecular connective tissue framework extends into the splenic pulp from the internal capsular surface to subdivide the organ into small communicating compartments. After entering the spleen at the hilum, arterial vessels branch into the trabeculae to enter the pulp. Veins and lymphatics draining the pulp also pass in the trabeculae to leave the spleen at the hilum. The splenic pulp is conventionally divided into three areas: red pulp, white pulp, and an interfacing marginal zone. The red pulp, so designated due to its gross appearance from the presence of blood, is composed almost entirely of large, branching, thin-walled blood vessels, called splenic sinuses or sinusoids, and thin plates or cords of cellular tissue lying between the sinuses to form splenic cords. Within this cordal meshwork, erythrocytes, platelets, and some granulocytes are crowded with macrophages and plasma cells, with macrophages often being the predominant cells. Lying within and surrounded by the red pulp are small gray-white zones of lymphatic tissue consisting of lymphocytes, plasma cells, and macrophages, which constitute the white pulp. The white pulp forms periarterial lymphatic sheaths and lymphatic nodules, which, like those of lymph nodes, may contain germinal centers. The marginal zone constitutes the interface between the red and white pulp and is an ill-defined vascular space where many arterial vessels terminate. Controversy has surrounded the exact nature of the splenic microcirculation for 300 years. Billroth is credited with the open circulation theory, in which either arterioles empty blood directly into tissue spaces or arterial capillaries open into pulp cords, with blood cells then passing through pores in the walls of splenic sinusoids to enter the venous circulation. In the closed circulation theory, splenic blood follows an endothelialized pathway throughout to flow directly into sinusoids. Studies in rabbits using plastic microspheres too large to pass through pores of the venous sinuses confirm the unique open splenic microcirculation. Ninety percent of splenic arterial flow enters the open circulation of the red pulp, with only 10% of the blood in arterial capillaries emptying directly into venous sinuses. Blood cells and particles such as particulate antigens must circulate through the meshwork of splenic cords before squeezing through 0.5 to 2.5 mm. pores between endothelial cells of the sinuses to enter the venous circulation. FUNCTION During early fetal development, the spleen produces red and white blood cells. By the fifth month of gestation, the spleen and other extramedullary sites of blood cell production no longer have hematopoietic function but retain the capability throughout life. As a result of a singular microcirculation, the spleen is a sophisticated filter having both blood cell monitoring and management functions and important immune functions. When the spleen is removed, these functions are lost. Normal red cells usually traverse the splenic circulation but may undergo repair by having surface abnormalities such as pits or spurs removed. Reticulocytes pass through the spleen more slowly than mature red cells and lose nuclear remnants and excess membrane before entering the circulation as mature cells. In reducing the membrane surface area, the spleen converts the red cell from a target appearance to a biconcave disc. The spleen also removes high-molecular-weight surface protein, Howell-Jolly bodies (nuclear remnant), Heinz bodies (denatured hemoglobin), Pappenheimer bodies (iron granules), and spur cells. These cleaned red cells, if they have the deformability to pass through the splenic circulation, reenter the bloodstream. Aged red cells (120 days) that have lost enzymatic activity and membrane plasticity are trapped and destroyed in the spleen The normal filtering function of the spleen also enables it to remove abnormal blood cells. Morphologically abnormal erythrocytes, such as the spherocytes of hereditary spherocytosis, fixed sickled cells, and rigid hemoglobin C cells, are trapped by the splenic filter. Blood cells coated with IgG are destroyed by the splenic monocytes, which have surface receptors for the Fc fragment of the IgG coating the cells. Because the spleen removes cells coated with IgG or IgM, it is the site of destruction in diseases such as autoimmune hemolytic anemia (AIHA), immune thrombocytopenic purpura, and probably Felty's syndrome. Parasites with intraerythrocytic habitation, such as malaria, can be pitted from the red cell by the spleen. 8 Red cells that are unable to deform to pass into the splenic sinuses are eventually destroyed by the histiocytes/macrophages of the red pulp. In addition to blood cell morphology and surface characteristics, rate of blood flow through the splenic microcirculation and alterations of splenic pulp pressure affect the filtering function of the spleen. For example, patients with splenic vein thrombosis have slow red cell passage through the splenic microcirculation due to elevated portal-splenic pulp pressure, with resultant increased red cell sequestration and destruction. The spleen is involved in specific and nonspecific immune responses. Properdin and tuftsin, which are synthesized in the spleen, are opsonins. Tuftsin binds to granulocytes to promote phagocytosis, while properdin can initiate the alternative pathway of complement activation to produce destruction of bacteria as well as foreign and abnormal cells. Because these opsonic proteins are also produced in other organs, the loss of the splenic contribution to their synthesis is probably small. However, serum levels of both tuftsin and properdin are below normal after splenectomy and in some diseases associated with hyposplenism. The macrophages and histiocytes of the spleen remove bacteria and abnormal or foreign cells and are especially effective in removing bacteria coated with antibody or opsonic proteins. If bacteria for which the host lacks pre-existing antibody are present in the bloodstream, the spleen's unique circulation makes it the major site for clearance of these bacteria as well as the initial site for synthesis of IgM. When radioactively labeled bacteria are administered to animals, the liver clears most of the well-opsonized microorganisms while the spleen removes those that are poorly opsonized. When specific antibody is lacking to facilitate bacterial removal by the liver, the spleen becomes the primary site for clearance. Encapsulated bacteria, which resist antibody binding, are less effectively removed in an asplenic individual than in a normal host. 8 The role of the spleen in removing malignant tumor cells is probably underestimated. Although large metastases to the spleen are uncommon, micrometastases occur frequently, with one study reporting 50% of spleens from patients with solid tumors containing neoplastic cells. Experimental evidence suggests that intense destruction of malignant cells in the spleen limits the incidence of clinically apparent metastases. A third important immune function of the spleen is the production of specific antibody, especially IgM. Particulate antigens, such as Salmonella flagella, lodge in the splenic red pulp and are transported by macrophages into the germinal centers where the IgM response is thought to occur. In asplenic individuals, IgM levels fall and the antibody response to a blood-borne antigen diminishes. Because of the anatomy of the splenic microcirculation, humoral and cellular antigens remain in contact with macrophages and lymphocytes for longer periods than in other areas of the reticuloendothelial system. The importance of an adequate time period for interaction of these cells after antigen exposure is becoming apparent as lymphocyte and macrophage subpopulations responsible for humoral and cellular immunity are identified. INDICATIONS FOR SPLENECTOMY Two large series of studies illustrate the changing indications for splenectomy that have accompanied improved diagnosis and therapy of hematologic diseases. In one report of a 30-year experience, splenectomy was performed for primary and secondary hypersplenism (41%), incidental to other operations (30%), for trauma (10.5%), for diagnosis (9%), for Hodgkin's staging (8%), and for non-Hodgkin's lymphoma (NHL) (1.5%). The more recent 5-year experience, at the University of North Carolina, Chapel Hill, showed the indications for splenectomy in 473 cases to be Hodgkin's staging (27%), incidental to other operations (20%), hypersplenism (16%), trauma (14%), NHL (7%), and diagnosis (7%). In a comparison between two series of splenectomies performed for hematologic disorders between 1946 and 1962 and 1963 and 1982, 400 splenectomies (20 per year) were performed between 1963 and 1982, compared with 94 (5.5 per year) during the earlier interval. 50 A sharp decline occurred in the number of splenectomies performed each year between 1974 and 1982. The evolution of the staging laparotomy for lymphomas, particularly Hodgkin's disease, with the decline in the average annual incidence of staging laparotomies since 1974 was the major factor responsible. Contributing to the differences was an increase in the total number of splenectomies for hereditary spherocytosis, idiopathic hypersplenism, and myeloproliferative disorders. The average number of splenectomies for immune thrombocytopenic purpura increased significantly between the two time periods. Hairy cell leukemia (HCL) and Felty's syndrome emerged as indications for splenectomy during the second time period. Of the 400 splenectomies performed for hematologic disorders between 1963 and 1982, the indications were therapeutic splenectomy (57%), Hodgkin's staging (40%), and diagnosis (3%). An improved understanding of immune anemia, thrombocytopenia, and neutrocytopenia has clarified the role of splenectomy in many hematologic diseases. Some diseases, such as immune thrombocytopenic purpura, appear to be increasing in incidence. Splenectomy as a means of staging Hodgkin's disease is no longer such an important diagnostic test in the overall approach to that disease, which now can be controlled in most patients using radiation therapy and chemotherapy. Splenectomy for splenomegaly associated with selected leukemias and NHLs is less commonly indicated because chemotherapy and radiation therapy have become more effective. Hypersplenism, both primary and secondary, is now diagnosed less commonly because of better definition and classification of diseases that previously were labeled as hypersplenic syndromes. The most frequent indications for splenectomy are now traumatic injury, immune thrombocytopenic purpura, and hypersplenism. In another report of splenectomy for hematologic disease, 81% of the patients underwent splenectomy to control anemia, thrombocytopenia, neutropenia, or discomfort from splenomegaly. 36 In 19%, splenectomy was performed for diagnostic purposes, most commonly Hodgkin's disease staging. The morbidity rate of 25% accurately reflects the frequency of complications that are related primarily to bleeding and infection. Sepsis is the usual cause of death after splenectomy for hematologic disease, and the mortality rate ranges from 5% to 27% Splenic Trauma The spleen is the most common intra-abdominal organ injured in blunt trauma and is frequently injured in penetrating abdominal injury. Selected older reports reveal mortality rates for splenic injury as high as 20%. Although some recent series report no deaths from splenic trauma, others still show a mortality rate approaching 10% because of the frequent association of other major organ injuries. Diagnosis. Injury to the spleen should be suspected in blunt upper abdominal injuries, which commonly occur in motor vehicle or bicycle accidents. Splenic injuries are often associated with fractured ribs of the left chest. The diagnosis and clinical course of an isolated splenic injury is variable. The spleen receives approximately 5% of the cardiac output, and a large laceration through the body of the spleen can extend into the splenic pedicle, causing extensive and continued hemorrhage, abdominal distention with hemoperitoneum, and shock. More commonly, a laceration deep into the pulp occurs or an adhesion between the spleen and its ligaments or diaphragm causes capsular avulsion with cessation of hemorrhage after an initial blood loss of 500 to 750 ml. If the injury does not involve the major splenic vasculature and is limited to the pulp or capsule, the patient may remain hemodynamically stable. However, subcapsular hematomas can form, which have the potential to rupture at a time remote from the injury, accounting for the phenomenon of delayed rupture of the spleen. Alternatively, some subcapsular hematomas evolve into splenic cysts while others resolve with fibrosis and scarring . Unfortunately, in the acute setting of evaluating the stable patient with splenic injury, it is difficult to identify which splenic injuries will resolve without operative management. If a splenic injury is suspected, admission to the hospital for monitoring is mandatory. Although many useful measures are available to aid in the diagnosis of splenic injury, their application requires a high index of clinical suspicion. A careful history should be obtained to include delineation of pain and a mechanism of injury consistent with splenic trauma. Usually injury to the left upper abdomen associated with fractured ribs of the left anterior chest alerts the clinician to proceed with evaluation by specific diagnostic tests. If the patient is in shock with hemoperitoneum, the diagnosis of splenic injury is established at laparotomy. The signs and symptoms of splenic trauma are those of hemoperitoneum. Generalized and nonspecific abdominal pain in the left upper quadrant occurs in approximately one third of patients with splenic injury. Pain referred to the tip of the left shoulder (Kehr's sign) is inconstant, varying in incidence from 15% to 75%, and is unreliable for excluding splenic injury but is useful for enhancing the diagnostic probability if present. Kehr's sign is elicited by bimanual compression of the left upper quadrant after the patient has been in Trendelenburg's position for several minutes preceding the maneuver. On rare occasions, patients with splenic injury have a palpable tender mass in the left upper quadrant (Ballance's sign), caused by an extracapsular or subcapsular hematoma with omentum adherent to the injured spleen. Patients with splenic trauma usually have hemoglobin/hematocrit values that are 10% to 30% below normal and a moderate leukocytosis. Diagnostic peritoneal lavage is a useful and inexpensive maneuver, which may reveal gross blood or an elevated red blood cell count diagnostic of intraperitoneal hemorrhage. When intraperitoneal hemorrhage is diagnosed by peritoneal lavage, laparotomy is performed to diagnose and treat all bleeding viscera, including the spleen. A variety of imaging techniques are useful in the diagnosis of splenic injury. Standard abdominal or contrast radiography may reveal depression of the splenic flexure of the colon and medial displacement of the stomach in patients with an injured spleen but are less reliable in establishing the diagnosis of splenic trauma than isotope or scanning techniques. Splenic angiography can demonstrate a variety of splenic injuries but is used infrequently because of the equal or greater accuracy of diagnostic peritoneal lavage and less invasive imaging techniques. Ultrasonography of the spleen can provide evidence of free blood and hematoma surrounding the splenic capsule with reasonable accuracy. Isotope scans ( 99mTc sulfur colloid) are popular in many centers for the acute diagnosis of splenic injury with a diagnostic accuracy rate exceeding 90%. However, computed tomography (CT) is probably the most accurate method available for diagnosing splenic injury . Reports of imaging techniques reveal a high sensitivity and specificity (>90%) for the diagnosis of splenic injury; however, considerable variation exists in the skill and enthusiasm of different radiologic units performing the tests for suspected splenic injury. Although CT and isotope imaging techniques are accurate methods for establishing the diagnosis of an injured spleen, the accuracy in individual instances is in large part dependent on the skill of the radiologist. Changing Concepts in the Treatment of Ruptured Spleen. In recent years the spleen's important role in cellular and humoral immunity has been clarified and the danger of overwhelming bacterial infection in asplenic patients has been established. Consequently, operative techniques for splenic preservation have been developed, and a concept for nonoperative management of selected splenic injuries is evolving. Although periodic reports of repairing injured spleens by use of suture or cauterization have been available for many years, interest in partial splenectomy has been rekindled since 1960. In animal and human studies, it has been shown that segmental resection of the spleen is practical and safe. In addition to partial splenectomy, splenorrhaphy, ligation of segmental vessels, and capsular repair are useful techniques for splenic salvage. Splenic salvage operations have been greatly aided by the development and use of topical hemostatic agents such as microfibrillar collagen (Avitene) and a variety of absorbable envelopes to aid in hemostasis from splenic injuries. 28 Although technically more difficult than splenectomy, splenic repair can be performed with comparable transfusion requirements, reoperation rates, and morbidity. Conservatism in the management of splenic injury has extended beyond repairing and preserving an injured spleen when possible. Because bleeding from splenic trauma appears to be more self-limited in children than in adults, nonoperative therapy may prove to be safe in selected pediatric patients. Nonoperative therapy requires a stable patient who is found by diagnostic tests to have an isolated splenic injury. At The Hospital for Sick Children (Toronto), where nonoperative management of splenic injury has been pioneered, 75 children with splenic injury were treated between 1981 and 1986. Ten (13%) required splenectomy or splenorrhaphy, but the remaining 65 patients (87%) were successfully managed nonoperatively. Of those patients treated nonoperatively, only 23% required blood transfusions. In comparison to an earlier report, current guidelines for management have resulted in an increased number of patients managed nonoperatively, a reduction in the number of patients receiving blood transfusions, and a decrease in the length of both hospital stay and time spent in the intensive care unit. In one large series of injuries associated with splenic trauma an appropriate note of caution was suggested before nonoperative management of splenic trauma is adopted. 47 In 258 patients with splenic injury, concomitant injuries requiring operative therapy were present in 36.5% of those with blunt trauma and 94% of patients with penetrating injury. Children younger than the age of 16 had an incidence of intra-abdominal injuries in addition to the spleen of 32.6% for blunt trauma and 100% for penetrating trauma. One pitfall of nonoperative management of splenic trauma lies in the significant possibility of failing to diagnose and treat concomitant intra-abdominal injuries. An additional concern is that most reported series of nonoperative management of splenic injuries include patients with blood transfusion requirements substantial enough to expect an incidence of transfusion-related hepatitis greater than the statistical probability of postsplenectomy sepsis. In addition, hospital time is usually longer for nonoperative management (13–16 days) compared with operative management (7 days) with a longer period for convalescence. The recommended management in adults with hemoperitoneum and demonstrated splenic injury is laparotomy with the expectation that 30% to 50% of spleens may be salvaged with sufficient (>50%) splenic pulp retained to preserve immune function. In both children and adults with splenic injury secondary to penetrating wounds, laparotomy should be performed because of the risk of significant injury to other intra-abdominal organs. All patients in shock or with significant transfusion requirement should have exploratory laparotomy for control of hemorrhage from the spleen and management of any other injured structures. Nonoperative treatment of splenic trauma in children is prudent only for the stable patient who is being followed in an appropriate hospital area by surgeons experienced in nonoperative management. There should be no hesitation to proceed with laparotomy and splenic repair. Operation is well tolerated, and splenic salvage techniques are probably more feasible in children than adults because of the higher ratio of splenic capsule to pulp. Any mortality from nonoperative management of splenic injury in children is unacceptable. Delayed Rupture of the Spleen. As early as 1866, Evans suggested that the spleen might bleed catastrophically at a time remote from injury. 43 It was postulated that injury to the pulp of the spleen could not be contained indefinitely by the thin splenic capsule under continuous arterial pressure. The usual interval between injury and the onset of clinically apparent intra-abdominal hemorrhage (period de latence, Baudet, 1907) is within 2 weeks, although longer intervals have been reported. 43 Although the incidence of delayed rupture of the spleen has been reported to be 15% to 30%, the criteria for diagnosis are variable and unconvincing. 43 It is apparent from splenic injuries managed nonoperatively that many heal by fibrosis and without sequelae. The entity of delayed rupture of the spleen is more properly referred to as delayed diagnosis of splenic injury. As imaging techniques for follow-up of suspected or proved splenic trauma become commonplace, it is likely that delayed rupture of the spleen will cease to be an entity with clinical meaning or application. Splenosis and Splenic Implants. Splenosis is the autotransplantation of splenic tissue after splenic trauma. Although fewer than 200 cases have been reported, the true incidence of splenosis undoubtedly is more common because of the high incidence of traumatic injury to the spleen. Appearing as sessile or pedunculated dark red nodules, splenic implants vary from a few millimeters to several centimeters in diameter. Splenic implants depend on a blood supply from small arteries penetrating the capsule and usually remain small or outgrow their blood supply and undergo infarction. Splenosis may occur anywhere in the peritoneal cavity and has been reported on the pericardium and the pleura as well as in the subcutaneous tissue of abdominal incisions. 10 Splenosis seldom causes symptoms and is usually discovered as an incidental finding at reoperation years after splenic trauma. Isolated reports have described splenosis producing intestinal obstruction from adhesions, stomach masses simulating carcinoma, and pain, presumably from torsion. Recent interest in the postsplenectomy sepsis syndrome has heightened interest in splenosis as potentially valuable for preservation of immune function by providing splenic implants at the time of removal of an injured spleen. Splenosis can be produced in a variety of animals by transplantation of splenic pulp. Von Stubenrauch seeded crushed splenic pulp throughout the peritoneal cavity in dogs and believed that splenoids arose de novo from the peritoneum. Perla described the histologic sequence of splenic transplants in rats. After transplantation, splenic implants underwent degeneration with only the reticulum cells at the periphery remaining viable after 24 hours. Regeneration of splenic tissue appeared to originate from the reticulum cell precursor. 10 Recently, investigators interested in preserving the immune function of the spleen have injected splenic pulp into the liver to avoid mechanical problems from adhesions that sometimes develop in association with splenosis. Splenosis, the born-again spleen, may provide the blood management functions of the spleen. The absence of Howell-Jolly bodies, siderocytes, and other postsplenectomy blood changes as well as the recurrence of the hematologic disease for which splenectomy was performed should raise suspicion of splenosis or the presence of accessory splenic tissue. Splenosis has been reported in conjunction with the expected postsplenectomy blood changes, suggesting a critical mass of splenic tissue is needed for recovery of splenic function. Residual splenic tissue can be detected by isotope scanning using 99mTc sulfur colloid . Splenic reticuloendothelial function has been investigated in a series of patients previously undergoing total splenectomy, partial splenectomy and splenic repair, and splenic autotransplantation. 48 Partial splenectomy and splenorrhaphy resulted in normal splenic reticuloendothelial function that was indistinguishable from a control group of patients sustaining trauma but who had intact spleens. Extraperitoneal splenic autotransplantation resulted in the preservation of a small amount of reticuloendothelial function. The subnormal reticuloendothelial function achieved by splenic autotransplantation was clearly superior to that resulting from total splenectomy without deliberate splenic autotransplantation. Splenic autotransplantation, which in this study involved placing thin slices of spleen weighing a total of 25 to 30 gm. into an anterolateral extraperitoneal pocket, appeared to be safe and was not associated with increased postoperative complications. Although autotransplanted splenic tissue, accessory splenic tissue, and splenosis can restore some of the spleen's blood management functions and antibody synthesis, it is unclear how much splenic tissue is needed for protection against overwhelming postsplenectomy sepsis. Studies have failed to identify reestablishment of resistance to postsplenectomy sepsis after autotransplantation of splenic tissue. Death from postsplenectomy sepsis has occurred in children and adults having a total mass of residual splenic tissue weighing 3 to 92 gm. Although residual splenic tissue can restore some of the spleen's functions, a critical amount of splenic tissue is required for full protection against postsplenectomy sepsis. Immune Thrombocytopenic Purpura Immune thrombocytopenic purpura (ITP, previously called idiopathic thrombocytopenic purpura) is a syndrome characterized by a persistently low platelet count. The thrombocytopenia is caused by a circulating antiplatelet factor that causes platelet destruction by the reticuloendothelial system. In most patients, the antiplatelet factor is an immunoglobulin (IgG) antibody directed toward a platelet-associated antigen. Circulating immune complexes may have a causal role in some cases, but their precise role is unclear. Proof of autoimmunity is lacking. 31 The majority of patients with ITP are young women. In Schwartz's series, the average age was 36 years and the duration of clinical symptoms before splenectomy was 24 weeks, with an average preoperative platelet count of 33,000 per cu. mm. 41 ITP is increasing in frequency, and the disease is being diagnosed more often now in men. This increase results in part from the association of immune thrombocytopenia with the acquired immunodeficiency syndrome (AIDS) and an increasing occurrence of ITP in three groups of patients at risk for developing AIDS—homosexual men positive for human immunodeficiency virus (HIV), parenteral drug abusers, and hemophiliacs receiving multiple transfusions. The diagnosis of ITP is suggested by spontaneous and easy bruising, petechiae, and mucosal bleeding. Menorrhagia is common, and prolonged bleeding after shaving trauma may be an initial complaint in males. Intracranial hemorrhage is a rare and usually fatal complication. The propensity for hemorrhage is reflected by the level of thrombocytopenia. A bleeding diathesis is unlikely with thrombocytopenia in the range of 50,000 to 100,000 per cu. mm. Bleeding with minor trauma or surgical procedure can be expected with platelet counts in the range of 20,000 to 100,000 per cu. mm. Spontaneous bleeding with purpura and petechiae, epistaxis, menorrhagia, gingival bleeding, and so on, occurs commonly with platelet counts below 20,000 per cu. mm. and especially below 5,000 per cu. mm. Crosby has suggested classifying patients with thrombocytopenia into those with dry purpura (petechiae and ecchymoses) and those with wet purpura (active bleeding from mucosal surfaces). This distinction postulates that patients with wet purpura are at increased risk for central nervous system bleeding and thus require aggressive treatment. Patients with easy bruisability or hemorrhage require a careful history with special emphasis on recent exposure to quinine, quinidine, sulfonamides, and thiazides that may produce drug-dependent antibodies and immune thrombocytopenia. Isoantibodies against transfusion products can also cause thrombocytopenia. Collagen disease such as systemic lupus erythematosus may be indistinguishable in initial presentation from ITP. 26, 31 Pseudothrombocytopenia, a phenomenon in which the platelet count is spuriously low, results when antibodies in the patient's serum react with platelets in blood anticoagulated with ethylenediaminetetraacetic acid (EDTA), causing agglutination. Platelet clumping results in a falsely low platelet count that will be at variance with the estimated number of platelets present on a peripheral blood smear obtained by fingertip puncture. EDTAdependent platelet antibodies have been detected in several patients erroneously diagnosed as having ITP. Diagnosis of immune thrombocytopenia requires the exclusion of drug-dependent antibodies, isoantibodies, collagen vascular disease, lymphoproliferative disorders, thyroid disease, recent viral illness, and spurious thrombocytopenia. Patients with classic ITP rarely have a palpable spleen (<2%), whereas a palpable spleen that reflects mild to moderate enlargement and an associated high incidence of generalized lymphadenopathy have been found in ITP associated with AIDS. ITP is diagnosed definitively only after exclusion of other illnesses or conditions that cause or are associated with thrombocytopenia. Except for thrombocytopenia, patients with ITP usually have normal blood cell counts. Antinuclear antibodies are rarely present, but autoantibodies have been noted in some patients. A peripheral blood smear shows thrombocytopenia, occasionally with an increased number of large platelets. A bone marrow aspirate reveals normal granulocytic and erythrocytic elements with an increased megakaryocyte count. Platelet Kinetics and the Immune System in ITP. Platelet kinetics in patients with ITP are markedly altered with an increased platelet production (four to five times normal) and an increased megakaryocyte mass being present in association with a greatly shortened platelet survival. 31 In patients with ITP, body-surface counts show primarily splenic sequestration of platelets with significant liver sequestration occurring only in patients with severe disease. The amount of platelet-associated antibody reflects the severity of the clinical disease and is inversely correlated with the patient's platelet count and intravascular platelet life span. The antiplatelet factor probably is an IgG antibody directed against a plateletassociated antigen. In some patients, the IgG antibody functions in combination with IgM, IgA, or both. 31 Antiplatelet antibody assays are now routinely available, and the value for platelet-associated IgG normally is less than 1200 gamma-globulin molecules per platelet. The spleen is an important site of antibody production, and splenic cells from patients with chronic ITP produce five to six times more IgG in culture than control splenic cells. 31 The initial immune response to the platelet antigen probably occurs in the spleen, or in the bone marrow where intramedullary platelets and megakaryocytes share antigenic determinants and may trigger a response. In its function as a monitor of the intravascular space, the spleen probably is more important in the early response. Less involved initially, the marrow assumes an important role as the immune response becomes generalized. With development and recirculation of memory cells (both B and T lymphocytes), the marrow becomes a major site of antibody production. The liver produces little or no antiplatelet antibody, and the lymph nodes are not deeply involved in the response to intravascular antigens. Platelet destruction in ITP requires sufficient quantities of antigen (platelets), antibody, and phagocytic cells in an environment that provides time for antibody binding and subsequent platelet phagocytosis. 31 The spleen is ideally suited for this function, and once platelet sensitization has occurred, phagocytosis is triggered by the Fc portion of the IgG molecule or by complement activation with C3b fixation to the platelet surface. The macrophage Fc receptor mechanism clearly is important as increased platelet-bound IgG is present in essentially all patients with ITP. Macrophage Fc and C3b receptors may act synergistically, resulting in a greatly enhanced phagocytic efficiency. Because 30% of the total circulating platelet mass is within the spleen at all times as an exchangeable platelet pool, the spleen is the most active site of platelet destruction. The stagnant blood flow in the splenic microcirculation allows sensitized platelets to be readily removed by phagocytic cells lining the reticular network of the red pulp. Having no resident platelet pool and possessing a rapid microcirculation by contrast, the liver assumes a major role in platelet destruction when severe disease and high antibody titers result in heavily sensitized platelets. The bone marrow is the most likely source of antibody in patients who have undergone splenectomy. 31 Intramedullary platelet destruction and inhibition of thrombopoiesis may occur as a result of antiplatelet antibody binding to both platelets and megakaryocytes, although the efficiency of the marrow reticuloendothelial system is below that of the liver and the spleen. A study investigating the mechanisms of increase in the platelet count after treatment of ITP determined the survival time and localization of radiolabeled autologous platelets and measured platelet-associated immunoglobulin levels before and after prednisone therapy or splenectomy. 12 Prednisone therapy produced an increased platelet count from increased platelet production. The increased platelet count after splenectomy correlated with increased platelet survival. The degree of radiolabeled platelet localization in the liver was normal in patients in whom splenectomy was effective and was increased to above normal in patients in whom splenectomy was ineffective. The conclusion that prednisone improves platelet counts primarily by increasing platelet production requires modification of the pathophysiologic concept of ITP to incorporate the hypothesis that in some patients the predominant cause of thrombocytopenia is ineffective marrow production of platelets rather than accelerated platelet removal. In summary, thrombocytopenia in patients with ITP usually occurs from a combination of intramedullary platelet removal by reticuloendothelial cells, causing ineffective platelet production and decreased survival of circulating platelets due to peripheral sequestration and destruction in the spleen and liver. Successful therapy may produce an increase in the platelet count either by increasing the effective production of platelets or by decreasing peripheral platelet sequestration and destruction. Splenectomy appears to increase platelet survival by removing a major organ of peripheral destruction. If the liver is the major site of platelet destruction, splenectomy may not result in improvement in the platelet count. Treatment. The goal of therapy in chronic ITP is to obtain a complete and sustained remission of the disease and to remove the patient from the risks of hemorrhage. This can be achieved in 80% to 90% of patients. When ITP is initially diagnosed, the patient should be hospitalized. A patient having active bleeding should remain at bed rest and have specific therapy instituted. Platelet transfusions provide immediate benefit and should be administered as needed to control bleeding. Although transfused platelets rapidly become coated with antibody and destroyed and provide only transient benefit, they afford protection against life-threatening bleeding. High-dose intravenous gamma-globulin is also useful but requires several days for a beneficial platelet increase to occur. Corticosteroid therapy (prednisone, 1 mg. per kg. per day or the therapeutic equivalent) is instituted at the time of diagnosis. Most patients with ITP are improved with administration of corticosteroids, with an increase in the platelet count occurring within 3 to 7 days and reaching a maximum in several weeks. 31 Complete and sustained remission with corticosteroid therapy is rare, although rates as high as 25% have been reported. 31 In most cases, even if the platelet count becomes normal, the response is transient, and thrombocytopenia recurs as the corticosteroid dose is tapered. Splenectomy should be performed in patients with ITP that is refractory to corticosteroid therapy. In the majority of patients, splenectomy is performed electively. Emergent splenectomy is necessary in patients with ITP who have evidence of central nervous system bleeding. Complete remission after splenectomy is more likely in patients who have shown a response to corticosteroids. Additional clinical features indicating the likelihood of a favorable response to splenectomy include patients who are younger than 60 years old, who have disease of relatively short duration, and who exhibit a prompt thrombocytosis with platelet counts reaching 500,000 per cu. mm. or more after splenectomy. Most patients, however, are improved after splenectomy, even if their platelet counts were not significantly increased by corticosteroid therapy. Eighty-eight percent of Schwartz's patients responded to splenectomy and developed normal platelet counts. Of those responding to splenectomy, 20% had platelet counts exceeding 100,000 per cu. mm. by the third postoperative day, and 90% of them had normal platelet counts after 1 week. The remaining responders developed normal platelet counts within 1 to 6 months postoperatively. In three patients, thrombocytopenia recurred after a long interval and was attributed in one patient to an accessory spleen. The level of platelet-associated IgG falls to normal after a response to splenectomy due to the removal of a large site of antiplatelet antibody production. 31 A corticosteroid response is also accompanied by a decrease in platelet-associated IgG. An increase in the platelet count often occurs before platelet-associated IgG falls because of the corticosteroid influence on the reticuloendothelial system. A response to immunosuppressants such as cyclophosphamide and vincristine is also associated with a decrease in platelet-associated IgG. ITP During Childhood. In children, particularly those younger than age 6, ITP often appears after a viral upper respiratory tract infection. In contrast to the adult form of the disease, childhood ITP usually undergoes spontaneous remission without specific therapy. A short course of prednisone therapy is usually prescribed; however, a clear benefit has not been demonstrated. 26 Intracranial hemorrhage is a life-threatening complication of childhood ITP and occurs in 1% to 2% of cases. It is responsible for the majority of deaths from the disease in this age group. The risk of intracranial hemorrhage is greatest during the first month of the illness. Most reported cases appear to be spontaneous, but minor head trauma may result in intracranial hemorrhage in patients with platelet counts below 10,000 to 20,000 per cu. mm. 52 Development of intracranial hemorrhage in ITP is an indication for emergency splenectomy. Spontaneous and complete remission occurs in approximately 85% of children with ITP. Those in whom spontaneous remission does not occur within 1 year are considered to have chronic ITP and usually undergo elective splenectomy to avoid the risks of chronic thrombocytopenia. Splenectomy and Perioperative Therapy for ITP. Most patients are referred for splenectomy after corticosteroid therapy has failed to achieve a complete and sustained remission. A small group of patients have ITP diagnosed due to abnormal bleeding during surgical procedures or after injury. A third group of patients require emergent splenectomy for intracranial hemorrhage. High-dose intravenous gamma-globulin is very effective in achieving an increase in the platelet count preoperatively in patients who do not respond to corticosteroids or are not candidates for corticosteroid therapy. It is postulated that intravenous gamma-globulin therapy promotes a rise in the platelet count due to temporarily reducing platelet destruction by saturating macrophage Fc receptors, thus producing a transient blockade of the reticuloendothelial system. A significantly improved platelet count (100,000–250,000/cu. mm.) occurs within 4 to 6 days and provides a therapeutic window for performance of splenectomy. 23, 51 In addition to affecting an increase in the platelet counts of patients failing to respond to corticosteroids or who are not candidates for corticosteroid therapy, high-dose gamma-globulin therapy is appropriate for the patient with ITP needing urgent splenectomy in whom a trial of corticosteroids is not warranted and in the pregnant patient with ITP late in the third trimester of pregnancy. Immunizations with polyvalent pneumococcal vaccine , Haemophilus influenzae vaccine, and Neisseria meningitidis vaccine should be administered as soon as it becomes likely that splenectomy will be performed. Ideally these immunizations should be carried out 10 to 14 days preoperatively. It is probable that patients receiving corticosteroids have a suboptimal early response to these vaccines but ultimately will develop protective antibody titers. The availability of blood and platelets for transfusion should be ensured, although the need for blood transfusion is rare. Intraoperative thrombocytopenic bleeding usually ceases after the splenic artery is ligated. In Schwartz's series, platelets were not used preoperatively and were administered intraoperatively or postoperatively in only 9 of 120 patients having splenectomy for ITP. Although a nasogastric tube is advisable for postoperative gastric decompression in most patients undergoing splenectomy, some avoid use of a nasogastric tube in patients with ITP because of the potential risk of precipitating hemorrhage from the nose or nasopharynx. Splenectomy can be performed through a variety of abdominal incisions. The midline incision is preferred in ITP because it allows entry into the peritoneal cavity without transection of abdominal muscles and thus reduces the potential for postoperative muscle hematoma. The spleen, usually of normal size, is assessed for adhesions and the nature of its ligamentous attachments. Splenic ligaments vary considerably in composition, being thin membranes affording easy dissection in some patients and being thick and tendinous in others. The technique for splenectomy is a matter of personal preference. The authors prefer the sequence of initially incising the posterior splenic ligaments followed by mobilizing the spleen and tail of the pancreas toward the midline for subsequent dissection of the splenic vessels in the hilus. Caution is taken to avoid excessive traction or trauma to the tail of the pancreas. Division of the gastrosplenic ligament is performed with suture ligation of the gastric ends of the short gastric arteries. After removal of the spleen, laparotomy pads are placed in the left upper quadrant while a search is made for accessory splenic tissue. Approximately 20% of patients have an accessory spleen, and common sites are the splenic hilus, adjacent to the splenic vessels and tail of the pancreas, greater omentum, and gastrosplenic and gastrocolic ligaments. Rarely has an accessory spleen been found in the intestinal mesentery, presacral, and gonadal regions. The left upper quadrant is not drained routinely. Indications for closed suction drainage are injury to the pancreas during hilar dissection and incomplete hemostasis. During the immediate postoperative period, corticosteroid therapy is continued intravenously, and the platelet count is monitored. It usually is possible to begin tapering the corticosteroid dose immediately, and in patients demonstrating a satisfactory thrombocytosis, corticosteroids are gradually reduced over 4 to 6 weeks and discontinued. The mortality rate for splenectomy in ITP is under 2% and occurs primarily in patients with intracranial hemorrhage. In approximately 80% of adult patients who have splenectomy for ITP, the platelet count returns to normal or above-normal levels within the first 6 weeks after operation. 31 In approximately 15% there is substantial improvement in the platelet count from preoperative levels, but it does not reach a normal level. Only about 5% of patients remain severely thrombocytopenic after splenectomy and require some form of chronic therapy. In these patients with refractory ITP, therapy having the least side effects is chosen to maintain the platelet count at a safe level (30,000 to 50,000/cu. mm.). Ingestion of antiplatelet drugs, trauma, azotemia, fever, and infection increases the bleeding tendency in thrombocytopenic patients. 31 Immunosuppressants such as cyclophosphamide, Vinca alkaloids (vincristine and vinblastine), azathioprine, and danazol, a modified androgen, have been used to treat patients with refractory ITP, with variable results . Thrombotic Thrombocytopenic Purpura Thrombotic thrombocytopenic purpura (TTP, Moschcowitz's syndrome) is a syndrome characterized by thrombocytopenia, microangiopathic hemolytic anemia, fluctuating neurologic abnormalities, progressive renal failure, and fever. TTP is produced by widespread deposition of platelet microthrombi, and the pentad of clinical manifestations results from occlusion of arterioles and capillaries by subendothelial and intraluminal deposits of hyaline material composed of aggregated platelets and fibrin. The etiology of TTP is unknown, and approximately 90% of the cases of TTP are idiopathic. The pathologic response in TTP may be initiated by various stimuli, including viral and bacterial infection, pregnancy, drugs (oral contraceptives, mitomycin, and cyclosporine), and nonspecified toxins. The syndrome has been associated with systemic lupus erythematosus and other connective tissue disorders, malignancies, and more recently with AIDS. TTP has a peak incidence in the third decade of life and occurs more frequently in females than in males. The differential diagnosis includes hemolytic-uremic syndrome, disseminated intravascular coagulation, drug reaction, eclampsia, aplastic anemia, idiopathic AIHA, ITP, leukemia, paroxysmal nocturnal hemoglobinuria, periarteritis nodosa, infection, systemic lupus erythematosus, and exposure to toxins. The exact role of the spleen in TTP is unclear, but approximately 20% of patients will have splenomegaly. Prognosis for untreated patients with TTP is very poor, with less than 10% surviving beyond 1 year. 23 The current therapeutic regimen of infusions of freshfrozen plasma results in dramatic improvement for the majority of patients with TTP. A combined therapeutic approach using plasma therapy, antiplatelet agents (aspirin and dipyridamole) and high-dose corticosteroid therapy is instituted immediately after the diagnosis is established. Plasma infusion or plasma exchange using plasmapheresis and replacement with fresh-frozen plasma achieves response rates between 70% and 90%. 23 It is speculated that plasma infusion or plasma exchange replaces a deficient plasma component or removes some toxic substance. 23, 51 Immunosuppressive drugs (vincristine and azathioprine) are also beneficial adjunctive agents in the present combined therapeutic approach for TTP. If combined-modality therapy fails, splenectomy should be performed. Splenectomy occasionally results in spectacular improvement, particularly when combined with high-dose corticosteroid therapy and antiplatelet drugs. 23 Although a clear physiologic explanation is lacking for this occasional response to splenectomy, prior experience has documented that 70% of the long-term survivors with TTP were patients who had undergone splenectomy. Hypersplenism Hypersplenism is a concept, probably first used by Chauffard in 1907, which refers to a variety of ill effects resulting from increased splenic function that may be improved by splenectomy. 23, 51 Criteria for diagnosis include: (1) anemia, leukopenia, thrombocytopenia, or combinations thereof; (2) compensatory bone marrow hyperplasia; (3) splenomegaly; and (4) improvement after splenectomy. 8, 23, 51 Hypersplenism is classified as primary when an underlying disease cannot be identified to account for the exaggerated splenic function. Secondary hypersplenism refers to those cases in which a specific or more-or-less welldefined disorder has been diagnosed. Because it now is possible to obtain more specific diagnoses for many patients who previously would have been thought to have primary hypersplenism, primary hypersplenism is now diagnosed much less frequently than secondary hypersplenism. Primary hypersplenism was initially described in 1939 by Doan and Wiseman as an illness consisting of neutropenia and splenomegaly for which splenectomy was curative. 40 The definition of the syndrome subsequently was broadened to include patients with variable degrees of anemia, thrombocytopenia, or pancytopenia. Subclassification of primary hypersplenism is used to describe splenic hyperfunction producing depression of one or more of the formed elements of the blood (red cells, white cells, and platelets). Primary splenic panhematopenia (pancytopenia) refers to depression of all formed elements, whereas in primary splenic neutropenia, depression of the white blood cells is the prominent feature. Most patients with primary hypersplenism are women. Clinical manifestations are dependent on the specific formed elements that are depressed and include pallor and other signs of anemia, fever, recurrent infections, oral ulcerations, ecchymoses, and petechiae. Splenomegaly is common. The peripheral blood smear shows leukopenia or varying degrees of pancytopenia without evidence of leukemia or myeloproliferative disorders. Pancellular hyperplasia is present in the bone marrow. Primary hypersplenism is a diagnosis of exclusion and should be accepted only after an exhaustive search for a specific etiology of hypersplenism has been unrewarding. Corticosteroids are seldom of benefit in primary hypersplenism. Splenectomy is indicated when the diagnosis is established and usually results in marked hematologic improvement for virtually all patients. Occasional patients have subsequently developed reticulum cell sarcoma or histiocytic lymphoma. Lymphoma having primary presentation in the spleen may present as asymptomatic splenomegaly with or without hypersplenism. Radionuclide studies, CT, and magnetic resonance imaging usually reveal nonspecific, featureless organ enlargement. If parenchymal expansion secondary to tumor infiltration and congestion becomes massive, splenic pooling and increased regional blood flow may result in hypersplenism. Lymphoma with primary presentation in the spleen may result in the diagnosis of idiopathic splenomegaly until splenectomy permits accurate histopathologic diagnosis. Secondary hypersplenism classically refers to a syndrome of pancytopenia (anemia, thrombocytopenia, and leukopenia) associated with portal hypertension from intrahepatic or extrahepatic portal or splenic vein obstruction. Hypersplenism associated with portal hypertension secondary to cirrhosis seldom requires splenectomy. Cytopenias commonly are improved after a shunt between the portal and systemic circulations, presumably caused by relief of congestive splenomegaly. Splenic vein thrombosis with bleeding from gastric varices should be treated by splenectomy, which usually cures the gastric variceal bleeding and any existing hypersplenism. Secondary hypersplenism includes a number of diseases sharing the common feature of splenomegaly. Rather than listing these, it is more appropriate to consider the mechanisms producing splenic enlargement 8 Work hypertrophy from immune response and/or red blood cell destruction, venous congestion, myeloproliferation, infiltration, and neoplastic proliferation within the spleen produce variable degrees of splenomegaly. Diverse pathophysiologic mechanisms are involved in the resulting hypersplenism . 8 In both primary and secondary hypersplenism, the degree of splenomegaly does not correlate closely with the severity of clinical symptoms or the degree of depression of formed elements of the blood. Hyposplenism Hyposplenism is a potentially lethal syndrome characterized by diminished splenic function. Hyposplenism was first described by Dameshek in 1955 in a patient with sprue who had an asplenic peripheral blood picture with Howell-Jolly bodies and target cells. 8 As in the asplenic patient, other peripheral blood findings that suggest hyposplenism are the presence of acanthocytes and siderocytes, a longterm lymphocytosis and monocytosis, and a mild thrombocytosis. 8 Diagnosis of hyposplenism is confirmed by an isotope scan ( 99mTc sulfur colloid) revealing an atrophic spleen. Hyposplenism can occur in the presence of a normal sized or an enlarged spleen . The danger of hyposplenism is the risk of developing potentially lethal sepsis (see The Problem of Overwhelming Postsplenectomy Sepsis). Sickle cell anemia is the most common disease associated with hyposplenism. Children with sickle cell anemia are vulnerable to overwhelming pneumococcal infection similar to that seen in asplenic children. The child with sickle cell anemia is most vulnerable when the spleen is enlarged. By the time the spleen becomes atrophic from recurrent infarctions (autosplenectomy), the patient will have developed some immunity from exposure to different pneumococcal strains. The most common surgical disease associated with hyposplenism is chronic ulcerative colitis, in which 40% or more of patients develop hyposplenism as the pancolitis progresses. Other conditions associated with hyposplenism in which the surgeon is commonly involved include thyrotoxicosis, corticosteroid administration, and patients who have received Thorotrast (thorium dioxide) as a radiocontrast agent. If a patient is suspected or proved to have hyposplenism, the same precautions against sepsis recommended for asplenic patients should be instituted. Hodgkin's Disease Described by Thomas Hodgkin in 1832, Hodgkin's disease is a malignant lymphoma characterized by the presence of typical, multinucleate giant cells. The unique cell, described by Sternberg and later Reed around the turn of the century, is essential for diagnosis. Hodgkin's disease is relatively rare, with a bimodal ageincidence curve that peaks in the late 20s and declines to the mid 40s. After age 45, the incidence of Hodgkin's disease increases with age. The disease is slightly more common in men than women. Most patients with Hodgkin's disease have asymptomatic lymphadenopathy at the time of diagnosis. The site of initial nodal involvement is the cervical area in most patients (65%–80%), followed by the axillary (10%–15%) and inguinal (6%–12%) regions. Retroperitoneal lymph nodes may be involved but require lymphangiography or CT for diagnosis. Mediastinal involvement occurs in 6% to 11% of patients at the time of diagnosis. Constitutional symptoms (B symptoms) such as fever, night sweats, weight loss, and pruritus are usually indicative of widespread involvement and are unfavorable prognostic signs. They may appear simultaneously with lymph node enlargement or may precede development of lymphadenopathy. A typical fever pattern is a high temperature alternating for a few days with an afebrile period (Pel-Ebstein fever). Less specific constitutional symptoms include localized acute discomfort in areas of adenopathy after ingestion of alcoholic beverages, malaise, lethargy, easy fatigability, generalized weakness, and anorexia. Many patients have a mild normochromic normocytic anemia. One third have a leukocytosis due to a neutrophil increase, and eosinophilia is present frequently. Lymphopenia is common in the later stages of the disease. The platelet count is normal initially but is frequently depressed in advanced disease. There is a progressive loss of T-lymphocyte function with reduced cell-mediated immunity. A classification of Hodgkin's disease was developed by the international symposium held in Rye, New York, in 1965, at which time the earlier classifications were simplified. In the Rye classification there are four histopathologic subtypes of Hodgkin's disease: lymphocyte predominance, nodular sclerosis, mixed cellularity, and lymphocyte depletion. Lymphocyte predominance and nodular sclerosis subtypes have a more favorable prognosis than mixed cellularity and lymphocyte depletion subtypes. However, the prognostic implications of subtyping are becoming less useful because of the excellent results of current aggressive treatment. Hodgkin's disease metastasizes initially in a predictable, nonrandom pattern through lymphatic channels to contiguous lymph node groups and organs with a prominent lymphatic tissue component. The predictable mode of spread of Hodgkin's disease provides the basis for irradiation of adjacent lymph node areas in patients with apparently localized disease. 3 Treatment and ultimately survival of the patients with Hodgkin's disease depend on the anatomic distribution of the disease and the presence or absence of specific symptoms, the stage of the disease, and the histopathologic subtype. Histopathologic diagnosis is made by lymph node biopsy in which the largest and most centrally placed node should be selected for excision. In a matted group or cluster of nodes, a central node from the group should be excised or a generous incisional biopsy specimen obtained. Nodes from the lower cervical or axillary areas provide the most satisfactory tissue for histopathologic evaluation, because nodes from the parotid, submandibular, and inguinal regions often show changes due to previous inflammatory processes in their regions of drainage. When only mediastinal adenopathy is present, biopsy is performed through mediastinoscopy or thoracotomy, as indicated. Laparotomy is seldom required to obtain the initial diagnosis in Hodgkin's disease. Since the concept of staging was introduced approximately 30 years ago, the staging process has undergone continued modification with the intent of accurately defining the anatomic sites of involvement and thus improving patient selection for the most appropriate type and amount of therapy. Stage I disease indicates nodal involvement in only one lymph node region. Stage II disease is limited to two or more lymph node regions on the same side of the diaphragm. Stage III refers to disease involving lymph node regions on both sides of the diaphragm (the spleen is considered a lymph node). Stage IV disease encompasses diffuse or disseminated involvement of one or more distant extranodal organs with or without associated lymph node involvement. Stage IV is further classified as A (absence) or B (presence) with regard to fever, night sweats, weight loss, and pruritus. The subscript E is used to classify selected patients having localized extranodal disease in Stages I to III (e.g., lung, muscle, bone, skin) contiguous to involved nodes. In general, the E designation is reserved for patients having extralymphatic disease so limited in extent and/or location that it is amenable to definitive treatment by radiotherapy. The S subscript indicates splenic involvement. Anatomic substages of Stage IIIA disease have been designated to differentiate between upper abdominal disease (III 1) and lower abdominal disease (III 2). A biologic difference or prognostic significance has not been clearly shown with respect to 5year survival or disease-free survival between upper and lower abdominal involvement. 42 Both a clinical stage designation and a pathologic stage designation are implied by the Ann Arbor staging classification. Clinical stage is dependent on history and physical examination, the initial diagnostic biopsy, laboratory tests, and the results of radiographic and imaging studies. Pathologic stage is more accurate than the clinical stage because histopathologic data from the bone marrow, liver, spleen, intra-abdominal lymph nodes, and other involved tissues (e.g. bone, skin, lung) provide precise knowledge of the extent of the disease. Lymphangiography and abdominal CT are reliable and complementary tests to evaluate retroperitoneal and abdominal nodal involvement. Lymphangiography has an overall accuracy of 80% to 90% with high sensitivity and specificity and can detect disease in nodes that are not significantly enlarged. Shortcomings include the need for bipedal incisions and a failure to adequately visualize the celiac, splenic hilar, and portal nodes. These and other enlarged lymph nodes can be detected by CT, which has lower overall accuracy, sensitivity, and specificity than lymphangiography. 42 CT is not helpful in detecting splenic involvement unless extensive splenic disease exists. 24, 25 When the lymphangiogram is positive, involvement of retroperitoneal nodes by Hodgkin's disease is confirmed by staging laparotomy in 80% to 90% of cases. 24, 42 Additionally, approximately 40% of patients with abnormal lymphangiograms have another site of Hodgkin's disease within the abdomen, most commonly the spleen. 24 A normal lymphangiogram usually indicates that the retroperitoneal lymph nodes are uninvolved (10%–15% incidence of false-negative results) but does not exclude other abdominal sites of occult disease. Approximately 20% of patients with negative lymphangiograms have intra-abdominal disease, usually in the spleen. Subdiaphragmatic Hodgkin's disease is frequently confined to the spleen and splenic hilar lymph nodes. The probability of subdiaphragmatic Hodgkin's disease is related closely to histopathologic subtype, with mixed cellularity and lymphocyte depletion subtypes having greater likelihood of subdiaphragmatic extension than lymphocyte predominance and nodular sclerosis subtypes. The probability of splenic involvement increases with increasing spleen size and is almost always present in spleens weighing more than 400 gm. The absence of splenomegaly does not exclude splenic involvement. Hodgkin's disease involving the spleen is commonly apparent on gross examination as grayish white nodules ranging from several millimeters to several centimeters. Liver involvement with Hodgkin's disease rarely occurs in the absence of splenic disease. Hepatic disease, in contrast to splenic disease, may not be apparent from inspection and palpation. In a report of the Stanford experience, the spleen was found to be involved with Hodgkin's disease in 39% of patients undergoing staging laparotomy. 42 In 50% of these, the spleen was the only site of intra-abdominal disease detected by staging laparotomy. Splenic involvement consisted of fewer than five nodules in 27%, with all of the nodules being too small to have been detected by CT or found on random biopsy. All positive liver and accessory spleen specimens were associated with positive splenic involvement, suggesting that the spleen is the trigger for visceral dissemination. Staging laparotomy, which in the past was frequently employed for pathologic staging of Hodgkin's disease, is now being used less frequently. Its use as a diagnostic test has been based on the following: 1. Hodgkin's disease generally begins in a single area and spreads initially in a predictable and nonrandom manner through lymphatic channels to contiguous lymph node areas and organs having a prominent lymphatic tissue component. 2. Selection of therapy is dependent on pathologic stage. 3. Assignment of stage using clinical criteria alone is often inaccurate. Twentyfive to 30% of clinically staged patients will have their stage of disease increased (upstaged), and 10% to 15% will be downstaged after laparotomy for a total alteration in stage of approximately 40%. (Patients with AIDS who develop Hodgkin's disease have great likelihood of being upstaged by laparotomy.) 4. Prognosis is related primarily to the pathologic stage of the disease. The role of staging laparotomy continues to be re-evaluated as a routine staging procedure for Hodgkin's disease. Diagnostic advantages and contributions of staging laparotomy have helped to significantly change the understanding and therapeutic management of patients with Hodgkin's disease, and the current success and widespread use of combination chemotherapy has challenged the need to know the precise anatomic extent of the disease required for treatment by radiation therapy. 31 Staging laparotomy is not applicable to all patients with Hodgkin's disease and should be performed only in patients in whom the results may change management decisions and plans for therapy. Patients with advanced disease, clinical Stage IIIB or Stage IV, do not benefit from staging laparotomy because treatment employs combination chemotherapy. (If splenomegaly is present or develops in these advanced stages of Hodgkin's disease, splenectomy may be of value to control cytopenias and reduce tumor burden.) Staging laparotomy has been restricted by the recognition of the limitations of radiation therapy for patients with extensive mediastinal presentation or with multiple extranodal sites. The success of combination chemotherapy in treating minimal or occult disease and for controlling recurrent disease after radiation therapy is a major consideration in further restricting the use of staging laparotomy. 31 Splenectomy in Hodgkin's staging has been shown to be a predisposing risk factor for acute leukemia in patients older than 40 years of age who have received combination chemotherapy (MOPP—mechlorethamine, vincristine, procarbazine, and prednisone). This surprising association suggests that staging laparotomy with splenectomy should not be done in patients of this age group who may eventually require MOPP-like chemotherapy. Controversy continues regarding the role of staging laparotomy, and improved noninvasive diagnostic tests and the introduction of more effective and less toxic chemotherapy continue to reduce the indications for this procedure. Currently, staging laparotomy is appropriate for selected patients with Hodgkin's disease of low clinical stage (Stage IA, IIA, and IIIA) in whom the results will have major influence on therapeutic management. Staging laparotomy is based on a systematic abdominal exploration with an organized approach to tissue sampling and consists of splenectomy, liver biopsy, and selective excision of abdominal and retroperitoneal lymph nodes based on CT, lymphangiographic, and operative findings. The operation is performed through a midline incision. The liver is examined initially, and if no gross evidence of disease is identified, a 2-cm. wedge of tissue is excised from the left hepatic lobe, and deep biopsy samples are obtained from the right and left lobes with a Trucut needle. Splenectomy is then performed with biopsy of splenic hilar lymph nodes and placement of identifying metal clips on the splenic pedicle. Partial splenectomy does not provide an adequate degree of accuracy in staging to justify its use as an alternative to splenectomy. The lesser omentum is incised, and a lymph node is removed from the celiac axis region. The hilum of the liver, cystic duct, and distal common duct areas are inspected, and representative lymph nodes are removed. Representative nodes are excised from the small intestinal mesentery and mesocolon. Exposure of the para-aortic, paracaval, and iliac lymph nodes is necessary to adequately examine these areas. If any abnormal or suspicious retroperitoneal nodes were demonstrated on the lymphangiogram, the nodes are excised and the sites are marked with metal clips. Confirmation that the specific node or nodes have been excised can be obtained by comparing an intraoperative abdominal radiograph with the lymphangiogram. Ten to 15% of patients with normal lymphangiograms will have involvement of the retroperitoneal lymph nodes by Hodgkin's disease (false-negative), and representative nodes should be excised even if the lymphangiogram is normal. A bone marrow biopsy should be obtained from the iliac crest to conclude the staging aspects of the operation. Preoperative bone marrow biopsy has a false-negative rate of 2% to 3% and would constitute a significant treatment error if not corrected by staging laparotomy findings. Oophoropexy (ovarian translocation) is advisable in the premenopausal woman in whom radiation therapy using an inverted Y port is likely. Both ovaries should be moved from the potential field of radiation and identified with metal clips. Lead shielding is an important adjunct to the protective effects offered by oophoropexy, and menstrual function is retained in approximately 55% of women receiving pelvic irradiation for Hodgkin's disease after oophoropexy and lead shielding. Ancillary procedures such as appendectomy or cholecystectomy add an unnecessary risk to the staging laparotomy and are not recommended. Staging laparotomy has minimal morbidity, and the mortality rate is less than 0.5%. The risk of developing postsplenectomy sepsis in patients with Hodgkin's disease is 10% or higher. Current treatment of Hodgkin's disease integrates radiation therapy and combination chemotherapy to achieve the maximum potential for cure. The success of combination chemotherapy in controlling and even curing Hodgkin's disease in patients demonstrating recurrence after radiation therapy has been a major therapeutic advance. In the Stanford experience from 1974 to 1980 for patients at all stages of Hodgkin's disease, survival was 86%, and freedom from progression (FFP) was 77% in surgically staged patients. 42 For patients with Stage IA and IIA disease being treated by irradiation only, survival and FFP were 91% and 82%, respectively, with no advantage being shown by adding chemotherapy (usually MOPP). Adding chemotherapy to radiation improved survival from 65% to 92% and FFP from 70% to 82% in patients with Stage IIIA disease. Patients with Stage IIIB disease had a generally poorer prognosis even with combination therapy, but alternating chemotherapy and radiation therapy has yielded significantly improved survival. Extensive extranodal disease (Stages IIE, IIIE, IV) has a poor survival (approximately 60% at 5 years), whether irradiation or combined therapy is used. Most patients with Hodgkin's disease present with Stage II or III disease. Ten to 15% present with Stage I or IV. Untreated Hodgkin's disease has a 5-year survival rate of 5%. Current survival rates for Hodgkin's disease, however, approximate 85% for all stages. The gold standard for the management of Stage I and IIA Hodgkin's disease is external-beam radiation. The potential contribution of adjuvant radiation therapy to the management of advanced-stage Hodgkin's disease remains controversial. The cornerstone of therapy for advanced Hodgkin's disease is combination chemotherapy. It is the staging between IIA and IIIA that might make some difference. There are subsets of patients in whom the likelihood of any staging change that would alter therapy is remote. The risk of having abdominal involvement is less than 10% in women with clinical Stage I disease, in men with clinical Stage I disease with lymphocyte predominance, and in women with clinical Stage II disease who are younger than 27 years of age with three different sites of involvement. Alternatively, the patient with Stage I disease who has a large mediastinal mass now usually requires chemotherapy in addition to external-beam radiation, because of recurrence outside the radiation ports and the fact of cardiac, especially pericardial, complications from radiation. Patients with Stage IIIB disease require no staging, nor do ones with multiple E, IIA 2. Another contraindication or reason for the decline in staging has been the appearance in significant numbers of patients of acute myeloid leukemia in patients who have had MOPP therapy and have received staging laparotomy with splenectomy. The approximate results of different stages of Hodgkin's disease, then, are as follows: Stages I and IIA treated by external-beam radiation alone have an 80% FFP (free from progression) and a 90% regression-free survival; Stage IIIA has a 94% relapse-free survival at 10 years with MOPP; and Stage IVA with alternating MOPP and ABD has an 80% remission. The potential of bone marrow transplantation adding to the treatment is an additional therapeutic maneuver. The reason, then, that staging laparotomies are less frequently done currently is not entirely due to the ability to better stage the disease by noninvasive means (e.g., CT, laparoscopic surgery). It in part results from the effectiveness of the various therapeutic modalities available. Salvage after recurrence is quite possible with most patients with Hodgkin's disease, making it less important that the small differential that would be changed from a staging process at the present time would make much difference in overall survival. Non-Hodgkin's Lymphomas Non-Hodgkin's lymphomas constitute a diverse group of primary malignancies of lymphoreticular tissue. The clinical course and natural history of NHL are more variable than those of Hodgkin's disease, the pattern of spread is irregular, and more patients have leukemic features. Current histologic classifications incorporate the nomenclature based on light and electron microscopic morphology, histochemical studies, and selected cell-surface antigens. For prognostic and therapeutic purposes, NHL is classified according to nodular (favorable) and diffuse (unfavorable) types. In contrast to Hodgkin's disease, only about two thirds of patients with NHL initially have asymptomatic lymphadenopathy. In 20% to 35% of patients, the onset of NHL occurs in an extranodal site. 3 In addition to peripheral and mediastinal lymphadenopathy, NHL is commonly found initially as an abdominal mass (retroperitoneal or mesenteric) or as hepatic and/or splenic enlargement. Constitutional symptoms such as fever, weight loss, and night sweats are frequently present. Occasionally the first manifestation of NHL is an oncologic emergency such as superior vena caval syndrome, spinal cord compression, or ureteral obstruction. In NHL the mode of spread generally is unpredictable, and most patients have disseminated disease at the time of presentation. In patients with initial nodal involvement, early spread may be limited to contiguous lymphatic sites or adjacent extranodal sites. More often, NHL spreads rapidly to distant nodal and extranodal sites through the bloodstream. Progression of NHL arising in extranodal areas may be through (1) local invasion of adjacent structures, (2) extension to regional lymph nodes, and/or (3) dissemination to noncontiguous lymph nodes and/or distant extranodal sites. The extranodal spread of NHL is comparable to the pattern of metastasis observed in carcinoma. 3 The median age at the time of diagnosis is 50 years, without sex preference. Patients younger than age 35 and older than 65 are more likely to have diffuse histology. The majority of NHLs are monoclonal B-cell tumors that are sometimes associated with an IgM or IgG protein. In some patients, particularly children with a mediastinal mass, the disease is thymic. As with Hodgkin's disease, chemotherapy and/or radiation therapy are the primary forms of treatment. Therapeutic considerations are based on the histopathologic type of lymphoma and the stage (extent) of disease. Because the majority of patients with NHL have disseminated disease at the time of presentation, staging laparotomy is seldom required and is indicated only for the patient with limited disease in whom laparotomy findings may influence selection of therapy. NHL having primary presentation in the spleen may present as asymptomatic splenomegaly, with or without hypersplenism. Radionuclide scanning, CT, and magnetic resonance imaging usually reveal nonspecific, featureless organ enlargement. If parenchymal expansion secondary to tumor infiltration and congestion becomes massive, splenic pooling and increased regional blood flow may result in hypersplenism. NHL with primary presentation in the spleen may result in the diagnosis of idiopathic splenomegaly until splenectomy permits accurate histopathologic diagnosis. Splenectomy in NHL is also performed for hematologic depression secondary to hypersplenism or to relieve symptomatic splenomegaly or discomfort from recurrent splenic infarctions. Hypersplenism may produce symptomatic anemia requiring red blood cell transfusions, dangerous levels of thrombocytopenia, and leukopenia with recurrent infections. The severity of the cytopenia may require withholding of chemotherapy and radiation therapy. Immunohemolysis or AIHA occasionally contributes to the anemia in NHL and is diagnosed by a positive Coombs test. The bone marrow typically has significant infiltration by neoplastic cells and additionally shows erythroid hypoplasia and decreased megakaryocytes. Because most patients with NHL have received chemotherapy or radiation therapy before becoming candidates for splenectomy, the splenic contribution to the pancytopenia can only be determined by the response to splenectomy. 13 Almost all patients with NHL undergoing splenectomy for hypersplenism require red cell and platelet transfusions preoperatively. Significant therapeutic benefit can be achieved by splenectomy in 80% to 90% of patients with advanced lymphomas (including Hodgkin's disease). Although patients with both NHLs and Hodgkin's disease may develop remission with reinstituted chemotherapy after correction of cytopenias, the eventual outcome of the underlying disease is unchanged. Most patients with well-differentiated lymphocytic lymphoma survive for 5 years, and many live 10 years after the diagnosis is made. The prognosis is more favorable for the nodular than for the diffuse forms of NHL. Chronic Lymphocytic Leukemia Chronic lymphocytic leukemia (CLL) is a lymphoproliferative abnormality that occurs primarily in the elderly (sixth decade of life or older), with a male predominance (2:1). Proliferation and accumulation of abnormal lymphocytes in lymphatic tissues result in the major signs of lymphadenopathy, splenomegaly, and lymphocytosis in the peripheral blood. The most constant abnormality on physical examination is lymph node enlargement, which frequently is found either by the patient or on routine physical examination. Splenomegaly is present in most patients and is progressive during the course of the disease. Hepatomegaly is a frequent finding, and lymphocytic infiltration of the skin and gastrointestinal and respiratory tracts occurs as the disease progresses. The diagnosis is based on the increase in the total leukocyte count due to a large number of abnormal, small, immature lymphocytes. Bone marrow examination demonstrates a variable and progressive degree of infiltration by abnormal lymphocytes. 23, 51 Therapy for CLL incorporates the judicious use of chemotherapeutic agents, corticosteroids, irradiation, and splenectomy. Although CLL is not cured by available therapeutic modalities, effective palliation is achieved in most patients, and many lead relatively normal lives. The disease progresses over 5 to 10 years with gradual increases in lymphadenopathy, splenomegaly, and hepatomegaly and development of weakness, weight loss, anemia, and thrombocytopenia. CLL is frequently complicated by development of immune hemolysis (AIHA), in which the hemolytic anemia is nearly always Coombs positive. If hemolysis becomes severe and cannot be controlled by medical therapy, splenectomy is useful to ameliorate the hemolytic process. As in NHL, splenectomy in chronic lymphocytic leukemia is performed primarily for hematologic depression secondary to hypersplenism and for palliation of symptomatic splenomegaly (Fig. 36–11 Fig. 36–11). Significant hematologic improvement occurs after splenectomy in 80% to 90% of patients, but the natural course of CLL is unchanged. Unless another illness supervenes, death usually occurs from hemorrhage or infection. Chronic Myeloid Leukemia Chronic myeloid (granulocytic, myelocytic) leukemia (CML, CGL) is a myeloproliferative abnormality characterized by marked elevation of the leukocyte count from myeloid cells in all stages of maturation and by neoplastic overgrowth of granulocytes in the bone marrow. The incidence of CML increases with age and is more frequent in males than in females (ratio 3:2). Splenomegaly is the most common physical finding, and sternal tenderness, lymphadenopathy, and hepatomegaly are frequently present. A unique chromosomal abnormality designated the Philadelphia chromosome (Ph) occurs in 90% of patients with CML. Patients who are Ph-negative have an atypical course and a poorer prognosis than patients with CML who have the Ph chromosome. Chemotherapy (busulfan, hydroxyurea), irradiation, radioactive phosphorus, and extracorporeal irradiation of the blood can control symptoms and most physical and laboratory abnormalities of CML during the chronic or treatable phase, which lasts from 1 to 4 years. 23, 51 Development of myeloblastic crisis appears to be an intrinsic feature of CML and indicates an accelerated or acute stage of the disease, which results in death from infection or hemorrhage within 3 to 6 months. Splenectomy may be of benefit in selected patients during the chronic stage of CML to palliate severe thrombocytopenia and/or anemia and to relieve pain from splenic infarctions or massive splenomegaly. Splenectomy offers no benefit in delaying the onset of blastic transformation, improving the quality of life after the development of blastic crisis, or in prolonging survival. 32 Hairy Cell Leukemia Hairy cell leukemia (leukemic reticuloendotheliosis) is an uncommon form of leukemia characterized by pancytopenia, splenomegaly without significant lymphadenopathy, and characteristic mononuclear cells in the blood and bone marrow. The disease is more common in males (ratio 4:1). The typical patient is a middle-aged man with moderate splenomegaly, absence of significant peripheral adenopathy, and variable hepatomegaly. Initial complaints among symptomatic patients are abdominal fullness or discomfort due to splenomegaly, nonspecific symptoms of fatigue, weakness, and weight loss, easy bruising from thrombocytopenia, or recurrent infections associated with leukopenia. In approximately 25% of patients, splenomegaly and cytopenias are detected during a routine examination or during evaluation for an unrelated illness. HCL is characterized by the presence of malignant cells that have irregular, filamentous cytoplasmic projections on light microscopy that give the cells a hairy appearance. The surface projections are demonstrable by electron microscopy as broad-based, undulating ruffles and patches of short, blunt microvilli. A pancytopenia of moderate severity is present in approximately two thirds of patients at the time of diagnosis. Hairy cells are frequently present in the peripheral blood and often account for a large proportion of the total white cell count. Demonstration in the hairy cells of tartrate-resistant acid phosphatase (TRAP) isoenzyme activity as a red reaction product is helpful supporting evidence for diagnosis. Although not required for diagnosis, the TRAP positive reaction product occurs in 90% to 95% of patients with HCL. Bone marrow biopsy permits definitive diagnosis of HCL from characteristic morphology. Ten to 15% of patients with HCL have an indolent course with a nearly normal life expectancy and require no specific therapy. These are usually elderly men who have minimal splenomegaly, relatively few hairy cells in the blood, and asymptomatic neutropenia. The remaining 85% to 90% require treatment because of one or more cytopenias resulting in symptomatic anemia requiring transfusions, thrombocytopenic bleeding, and repeated infections attributable to neutropenia. Pancytopenia develops from concurrent splenic pooling secondary to infiltrative splenomegaly and bone marrow replacement with hairy cells. Symptomatic splenomegaly and recurring splenic infarctions are other indications for therapy. For the majority of patients who require some form of therapy shortly after diagnosis, splenectomy continues to be an early consideration. Splenectomy is most appropriate for those patients with severe cytopenias, a large spleen, and patchy bone marrow infiltration. It results in rapid palliation, and almost all patients have hematologic improvement. Blood cell counts return to normal in 40% to 50% of patients, with the response lasting for many years and almost half the patients requiring no further therapy. Patients with HCL having diffuse infiltration of the bone marrow, minimal splenomegaly, and severe cytopenias gain only minor or short-term benefit from splenectomy and require additional therapy. In the past 5 years interferon alfa and pentostatin have been found to be highly effective systemic therapy for HCL. Randomized trials of interferon alfa versus pentostatin are in progress, both for newly diagnosed HCL patients and those patients previously having had splenectomy. Presently, interferon alfa remains the systemic therapy of choice, with pentostatin being indicated for patients with HCL that is refractory to interferon alfa. Splenectomy likely will continue to have a place in the sequential treatment of those patients with HCL requiring therapy. SPLENECTOMY FOR ANEMIA Hemolytic anemia results from an increase in the rate of red blood cell destruction. The adult bone marrow can produce red cells at six to eight times the normal rate, and hemolysis must be reasonably severe before laboratory or clinical evidence of anemia occurs. Diagnostic evaluation should include a detailed family history because many hemolytic anemias that improve after splenectomy have a hereditary basis. Congenital hemolytic anemias have a defect intrinsic to the red blood cell that may involve the cell membrane (hereditary spherocytosis), cellular metabolism (pyruvate kinase deficiency, glucose-6-phosphate dehydrogenase deficiency), hemoglobin structure (sickle cell anemia), or hemoglobin chain synthesis rates (thalassemia). Acquired hemolytic anemias have an extracorpuscular factor that affects normal red cells. Chromium-51–labeled red cell survival studies are sometimes useful to confirm hemolysis and a shortened red cell life span and to determine sites of red cell destruction. Clinical features include variable pallor related to the degree of anemia, mild, fluctuating jaundice, and splenomegaly. Pigment gallstones are common after childhood and may produce biliary tract symptoms. Valuable laboratory studies include serum direct and total bilirubin and haptoglobin levels. Jaundice associated with hyperbilirubinemia resulting from hemolysis is caused by an excess of unconjugated (free) bilirubin and is measured by an increase in the indirect reacting fraction of bilirubin. The unconjugated bilirubin that is bound to albumin does not enter the urine, and indirect hyperbilirubinemia thus is not associated with biliuria. Reticulocytosis and bone marrow erythroid hyperplasia reflect increased red cell production. Red cell morphology is often abnormal, as is osmotic fragility. Red cells tagged with chromium-51 demonstrate a shortened red cell survival. Hereditary Spherocytosis Hereditary spherocytosis is a relatively common, genetically determined red blood cell membrane disorder that results in hemolytic anemia. The erythrocyte membrane defect results from a deficiency in spectrin, a major component of the membrane skeleton that is thought to be responsible for the shape, strength, and reversible deformability of the red blood cell. The membrane abnormality leads to a gradual loss of red cell surface area, so that instead of remaining a flexible biconcave disc, the red cell becomes small and spherical. Lacking adequate deformability to traverse the splenic microcirculation, spherocytes are trapped in the splenic red pulp and are eventually destroyed by reticuloendothelial cells. Hereditary spherocytosis occurs primarily by autosomal dominant inheritance with variable expression. Twenty to 25% of the cases appear sporadically. The severity of the anemia and other clinical manifestations are variable. The disease may be so severe that repeated blood transfusions are required to maintain a functional hemoglobin level, or it may be so mild as to go unnoticed in childhood, becoming manifest in adult life with development of symptomatic cholelithiasis. Aplastic crisis, which usually is precipitated by a viral illness such as human parvovirus, may produce a rapidly worsening anemia that may be life threatening. Fluctuating jaundice due to hemolysis is common, and pigment gallstones are frequent, with the incidence being directly related to the severity of the hemolysis and patient age. Cholelithiasis develops in 20% to 55% of patients with hereditary spherocytosis but is uncommon before age 10. Moderate splenomegaly is a characteristic physical finding. Diagnosis is established by the presence of spherocytes in the peripheral blood, reticulocytosis (usually 5%–20%), an increased osmotic fragility, and a negative Coombs test. Splenectomy is indicated in virtually all patients. In children, splenectomy is usually performed after age 6 but can be done at a younger age if warranted by the severity of the anemia and the need for frequent transfusions. After splenectomy, hemolysis is alleviated, and clinical cure of the anemia is achieved in most patients. The intrinsic red cell membrane defect is unaltered by splenectomy, but red cell survival becomes normal. With resolution of hemolysis, jaundice disappears, and the increased risk of calculous biliary tract disease is removed. Gallbladder ultrasonography is advisable before splenectomy in anticipation of combining cholecystectomy with splenectomy if gallstones are demonstrated. Hereditary Elliptocytosis Hereditary elliptocytosis is a relatively common heterogeneous red blood cell membrane disorder characterized by an abundance of elliptical red cells. The abnormality usually produces a mild anemia, and most patients remain asymptomatic throughout their lives. Like hereditary spherocytosis, hereditary elliptocytosis is caused by an abnormal erythrocyte membrane skeleton. Several defects in the red cell membrane skeleton have been identified in hereditary elliptocytosis and include impaired association of spectrin chains and a quantitative deficiency of protein 4.1. Symptomatic individuals have a mild hemolytic anemia with clinical and laboratory features similar to those of hereditary spherocytosis except for the elliptical appearance of the erythrocytes. Splenectomy is indicated in symptomatic patients, and results are uniformly good, although the abnormal erythrocyte morphology persists. Hereditary Pyropoikilocytosis Hereditary pyropoikilocytosis (HPP) is a rare congenital hemolytic anemia that is catalogued along with hereditary elliptocytosis because of certain molecular and morphologic similarities. Distinguished from hereditary elliptocytosis (and hereditary spherocytosis) by marked alterations in red cell morphology and by the pattern of inheritance, this severe hemolytic disorder occurs most commonly in blacks. Erythrocytes in HPP are severely deformed, and virtually all red cells are poikilocytic, fragmented, spherocytic, or elliptocytic. Osmotic fragility is increased, and red cells in HPP exhibit increased susceptibility to thermal injury. The decision for splenectomy in HPP is deferred until the natural course of the disease has been established. In some newborns, HPP gradually evolves into a morphologic picture characteristic of hereditary elliptocytosis. True HPP persists as a severe hemolytic anemia that usually requires early splenectomy, which greatly reduces hemolysis. Hereditary Nonspherocytic Hemolytic Anemia A number of erythrocyte enzyme deficiencies associated with hemolytic syndromes constitute this group of hemolytic anemias. Pyruvate kinase (PK) deficiency is the prototype of the enzymopathies involving the Embden-Meyerhof pathway of anaerobic glycolysis in the red cell. PK deficiency is inherited as an autosomal recessive trait and affects both sexes equally. An unusually high incidence exists among the Pennsylvania Amish. A discrepancy between red cell energy needs and adenosine triphosphate–generating capacity produces irreversible membrane injury with cellular distortion, rigidity, dehydration, and premature destruction of the red cells by the spleen. 23, 51 The severity of the anemia is variable. Splenectomy results in improvement, but hemolysis is not abolished, and mild anemia persists. After splenectomy, transfusion requirements are reduced, young children experience a period of rapid catch-up growth, and the danger from aplastic crises is reduced. It is important to differentiate between pyruvate kinase deficiency and other erythrocyte enzymopathies that cause hemolytic anemia such as G-6-PD deficiency and its variants. Specific enzyme assays are employed for this purpose. In G-6-PD deficiency, hemolysis is precipitated by infection and other acute illness, certain drugs, and fava beans. Splenic enlargement is rare, in contrast to frequent splenomegaly with pyruvate kinase deficiency, and splenectomy is not indicated for patients with G-6-PD deficiency. A role for splenectomy in other erythrocyte enzyme deficiency states has not been established. Sickle Cell Anemia Sickle cell anemia is a hereditary hemolytic anemia occurring in blacks who are homozygous for the sickle hemoglobin (HbS) gene. Sickle hemoglobin (HbS) differs from normal adult hemoglobin (HbA) only in the substitution of valine for glutamic acid in the sixth position of the beta chain. HbS, which results from this single amino acid substitution, imparts the sickle shape to deoxygenated red blood cells and is responsible for the wide spectrum of clinical features that characterize sickle cell anemia. The highest incidence of HbS occurs among black Africans and descendants of emigrants from equatorial Africa. Sickle cell anemia (homozygous state for HbS) occurs in approximately 0.5% of the black population, and sickle cell trait (heterozygous state for HbS) is present in approximately 8% of African Americans. In the homozygous state, HbA is totally lacking and the red cells contain predominantly HbS. The red cells of individuals with sickle cell trait contain both HbA and HbS, with the relative amount of HbS ranging between 35% and 45%. A combination of two variant hemoglobin genes or a combination of a variant hemoglobin and an interacting thalassemia gene results in doubly heterozygous states designated by both aberrant gene products (e.g., HbS/C, HbS/beta thalassemia). Under conditions of reduced oxygen availability, red cells containing HbS acquire the sickle-shaped deformity due to the intracellular polymerization of the HbS molecules. Sickling of erythrocytes containing HbS occurs more readily with a reduced pH, higher intracellular concentration of HbS, low intracellular concentrations of HbF (fetal hemoglobin), and conditions favoring hemoglobin deoxygenation. Increased blood viscosity due to the sickled cells and an increased adhesion of sickled cells to vascular endothelium result in circulatory stasis and stagnation that leads to further reduction in oxygen tension, further sickling, and a vicious cycle of erythrostasis. The consequent thrombosis, ischemia, necrosis, and organ fibrosis result in the clinical features of sickle cell anemia. Patients with sickle cell anemia characteristically are without symptoms until the second half of the first year of life due to an initial sufficiency of HbF that limits clinically significant sickling. Clinical features of sickle cell anemia, which are both acute and episodic (crises) and chronic and progressive, are more a consequence of the rheologic properties of the sickle cells than of the anemia itself. Patients with sickle cell crisis often have severe abdominal pain and signs of peritoneal irritation similar to those of acute surgical illnesses such as acute cholecystitis and appendicitis. Clinical features of abdominal crises in patients with sickle cell anemia tend to be similar for a given individual, and deviation from previous patterns may be an important differentiating feature of an acute surgical illness in patients with sickle cell anemia. 27 Chronic features of sickle cell anemia include retarded growth and development after the first decade; bone and joint disease; cardiovascular, pulmonary, hepatobiliary, genitourinary, and neurologic manifestations; hematuria; priapism; and ulcerations over the malleoli and distal portions of the legs. The incidence of pigment gallstones in patients with sickle cell anemia increases with age. Calculi appear first in childhood (2–4 years of age) and are present in approximately 70% of adult patients. Diagnosis is established by the presence of characteristic sickle cells on blood smear, hemoglobin electrophoresis demonstrating predominantly HbS, variable amounts of HbF (5%–15%) and no HbA, and the presence of the sickle cell trait in both parents. Treatment is palliative and is directed toward minimizing complications of the disease. Many patients die during childhood from infections, renal failure, and heart failure. Rarely will a patient with sickle cell anemia have a relatively normal life span. The role of the spleen in sickle cell anemia is unclear. Sequestration crisis characterized by sudden trapping of blood in the spleen is a complication that occurs almost exclusively in infants and young children whose spleens are chronically enlarged. Further enlargement of the spleen occurs rapidly at the expense of the blood volume, and hypovolemic shock and death may occur within hours. Splenomegaly first becomes apparent after 6 months of age and characteristically persists throughout childhood. Despite splenomegaly, splenic hypofunction may be documented as early as 5 months of age, and the risk of overwhelming infection exists in a child with sickle cell anemia by age 1 year. By adolescence or early adult life, recurrent infarctions have resulted in splenic atrophy and functional asplenia (hyposplenism). (See Hyposplenism and The Problem of Overwhelming Postsplenectomy Sepsis.) Splenectomy may be beneficial to the occasional child with sickle cell anemia in whom excessive red cell sequestration occurs in an enlarged spleen. The beneficial effect of splenectomy clearly is related to spleen size and is most effective in children with large spleens. Sickle cell trait is rarely associated with significant clinical or hematologic manifestations, although splenic infarction has occurred in patients flying at high altitudes in unpressurized aircraft. Thalassemia (Thalassemia Syndromes) These hereditary hemolytic anemias result from a defect in hemoglobin synthesis in which one of the hemoglobin polypeptide chains is synthesized at a markedly reduced rate. Specific pairs of genes are responsible for synthesis of the alpha, beta, gamma, and delta chains of the hemoglobin molecule, and a deficiency in synthesis of one of these subunits may lead to one of the thalassemia syndromes. Thalassemia is classified by the deficient peptide chain. Beta-thalassemia, in which there is a quantitative reduction in the rate of beta chain synthesis, is the most common type of thalassemia. When the abnormal gene is inherited from both parents (homozygous), severe anemia, termed thalassemia major, results. Heterozygous patients have a mild anemia termed thalassemia minor. The term thalassemia intermedia is used to describe some homozygous patients who have a milder than usual course and some heterozygous patients who have a more severe course than usual. In thalassemia major, the reduction in the rate of beta chain synthesis produces a marked decrease in the amount of normal adult hemoglobin (HbA) with a compensatory increase in fetal hemoglobin (HbF). Homozygous alpha-thalassemia is incompatible with life, and these infants are stillborn or die shortly after birth. Patients with heterozygous alpha-thalassemia have a mild form of anemia similar to that in heterozygous beta-thalassemia. The pathogenesis of hemolysis in thalassemia lies in the unbalanced synthesis of the polypeptide chains. Because of the absence of the complementary polypeptide chain with which to bind, the overproduced normal chains form aggregates that precipitate within the red cell cytoplasm and lead to premature cell destruction. In homozygous beta-thalassemia (thalassemia major), the deficiency of beta chain synthesis causes a relative overproduction of alpha chains, which undergo aggregation to form insoluble inclusions in bone marrow erythroid precursors. Ineffective erythropoiesis occurs because of the death of many of these cells. Additionally, the inclusion-bearing red cells are detained in the spleen, where they sustain mechanical and metabolic injury that facilitates their ultimate destruction. Thalassemia major results in a severe anemia and clinical manifestations, usually within the first year of life. Pallor, retarded growth, and enlargement of the head with thalassemic facies are present, along with splenomegaly and hepatomegaly. The intense erythroid hyperplasia in the bone marrow causes expansion of the medullary cavities and attenuation of the cortex, producing bony abnormalities and a predisposition to fractures. Iron overload due to defective iron utilization coupled with increased iron absorption and frequent blood transfusions is a common complication. The peripheral blood smear in thalassemia major shows a microcytic hypochromic anemia with a severe degree of poikilocytosis, anisocytosis, and polychromatophilia. Nucleated red cells are invariably present and may outnumber the leukocytes. Reticulocytosis and leukocytosis are characteristic, but the platelet count is generally normal. Hemoglobin electrophoresis in thalassemia major reveals absence or almost complete absence of HbA with the presence of large amounts of HbF. Treatment consists of transfusion therapy and iron chelation, and splenectomy is effective in selected patients. Although the basic hematologic disease is not influenced, splenectomy decreases blood transfusion requirements and relieves discomfort from splenomegaly. Most patients with thalassemia major die during the second decade of life from complications of iron excess with myocardial hemosiderosis. Patients with alpha-thalassemia minor and beta-thalassemia minor rarely need treatment, and an important therapeutic consideration for patients with thalassemia minor is avoidance of therapeutic iron to minimize the risk of iron overload. Autoimmune Hemolytic Anemia Autoimmune hemolytic anemia is an acquired hemolytic anemia resulting from antibodies that are produced by the body against its own red cells. Patients with AIHA have the usual manifestations of hemolysis with anemia, reticulocytosis, a shortened erythrocyte survival time, fluctuating jaundice, and splenomegaly. The blood smear in AIHA shows spherocytes and microspherocytes in numbers exceeded only in hereditary spherocytosis. The distinguishing feature of AIHA is a positive direct Coombs test, which identifies antibody on the red cell surface. The type of antibody attached to the red cell determines the mechanism of hemolysis as well as the site for primary destruction of the sensitized cells. Anti–red cell antibodies are classified as warm reactive or cold reactive, depending on whether they bind to red cells most avidly at 37º C or have progressively greater affinity for erythrocytes as the temperature approaches 0º C. Warm-reactive antibodies usually are IgG (less commonly IgM, IgA, or a combination) and facilitate sequestration and destruction of sensitized erythrocytes in the spleen. When IgG-coated red cells become attached to splenic macrophages, which have receptors for the Fc portion of the IgG molecule, portions of the red cell membrane are removed, rendering the erythrocyte more spherical and more susceptible to sequestration and premature destruction. Red cells coated by both IgG and complement are destroyed by the reticuloendothelial system generally and not primarily by the spleen. Cold-reactive antibodies usually are IgM (rarely IgG or IgA) and bind to red cells mainly in the peripheral circulation where the blood temperature is cooled. Cold-reactive antibodies may cause either immediate intravascular hemolysis by complement-mediated mechanisms or sequestration and destruction of sensitized red cells by the liver. These patients usually have chronic hemolysis that is acutely worsened by cold exposure and often demonstrate acrocyanosis (Raynaud's phenomenon) due to intracapillary red cell agglutination. The designation autoimmune in AIHA must not obscure the fact that in many cases the hemolytic process is associated with or related to a drug or a reversible disease that can be eliminated. Drugs associated with AIHA include penicillin, cephalothin, streptomycin, methyldopa (Aldomet), quinidine, quinine, phenacetin, p-aminosalicylic acid, and several sulfonamides. AIHA may occur in association with another disease, such as mycoplasmal pneumonia, viral infections, chronic lymphocytic leukemia, lymphoma, Hodgkin's disease, systemic lupus erythematosus, infectious mononucleosis, and AIDS. When a drug exposure or an underlying disease is identified, AIHA is termed secondary. When no other etiologic association is demonstrable, AIHA is classified as primary or idiopathic. AIHA occurs at any age and in both sexes but is more common in women older than age 50. Pallor and splenomegaly are the main physical findings in idiopathic AIHA, whereas in secondary AIHA additional clinical features of the underlying disease are present. The severity and duration of the hemolytic anemia may vary, and in some patients the course is rapid and fulminating. Severe hemolysis may produce hemoglobinuria and acute tubular necrosis. When AIHA follows mycoplasmal pneumonia, the disease may be acute and self-limited over several weeks and require no therapy. More often the disease is chronic, with varying degrees of severity over months or years. Treatment is directed toward the hemolytic anemia and any underlying disease. Blood transfusions, corticosteroid therapy, and splenectomy are important aspects of treatment for the anemia. Splenectomy is usually performed in patients with AIHA in whom either corticosteroids are ineffective or an excessive corticosteroid dose is required, or when complications preclude corticosteroid use. Chromium51–labeled red cell studies are useful to measure the degree of splenic sequestration and to serve as a guide for selecting patients who are most likely to respond to splenectomy. Splenectomy results in a favorable response, with complete hematologic remission in approximately 80% of patients demonstrating significant splenic sequestration. Lack of significant red cell sequestration by the spleen does not preclude a good response to splenectomy. Splenectomy is more likely to induce a complete and sustained remission in primary (idiopathic) AIHA in which only IgG (warm-reactive) antibodies coat the red cells. In addition to removing the primary site for destruction of the sensitized red cells, splenectomy can be expected to significantly reduce production of anti-red cell antibody, because the spleen is a major site for IgG antibody production. The prognosis for patients with secondary AIHA depends mainly on the underlying disease and is generally favorable when the hemolytic anemia follows a viral illness or is related to a drug exposure. Prognosis is poor when AIHA is associated with an underlying malignancy or one of the collagen diseases. The presence of complement indicates greater likelihood of association with an underlying disease than the presence of IgG alone coating the red cells. AIHA due to cold-reactive antibodies is usually not benefited by splenectomy, and treatment for these patients consists of avoiding cold temperatures, treating any underlying disease, suppression of antibody production, and employing plasmapheresis in acutely ill patients. Hereditary Hydrocytosis and Xerocytosis Hereditary hydrocytosis and xerocytosis are rare forms of hemolytic anemia that result from a primary alteration in red cell membrane monovalent cation permeability. If the major effect involves membrane permeability to sodium, sodium gain exceeds potassium loss with an increase in total intracellular cation content and water movement into the red cell. The water-distended red cells (hydrocytes) have increased fragility, a low mean corpuscular hemoglobin concentration and an elevated mean corpuscular volume, and a characteristic fishmouth (stomatocyte) appearance on peripheral blood smear. When the permeability disorder allows potassium loss to exceed sodium gain, total intracellular cation content decreases, with resulting loss of water and cell dehydration. The dehydrated red cells (xerocytes) have a low mean corpuscular volume, an elevated mean corpuscular hemoglobin concentration, and a dense appearance on blood smear. Xerocytosis is differentiated from hereditary spherocytosis, elliptocytosis, or other conditions where the mean corpuscular hemoglobin concentration is elevated by red cell morphology and resistance of the cells to osmotic lysis. Splenectomy is effective in hydrocytosis by reducing hemolysis and eliminating the need for transfusion and the potential risk for life-threatening aplastic crises. In contrast to hereditary spherocytosis, mild hemolysis persists after splenectomy, and the risk of pigment gallstone formation continues. Splenectomy is seldom required for xerocytosis because the hemolysis is usually not severe. MISCELLANEOUS ANEMIAS SOMETIMES BENEFITTED BY SPLENECTOMY Splenectomy is occasionally performed for rare disorders such as acquired idiopathic sideroblastic anemia, congenital dyserythropoietic anemia, and porphyria erythropoietica. In these syndromes, splenectomy may offer significant benefits by improving the hemolytic anemia and reducing transfusion requirements. Myeloid Metaplasia (Agnogenic Myeloid Metaplasia, Myelofibrosis, Myelosclerosis) Myeloid metaplasia is an unusual illness with numerous names but no known cause. There is gradual and progressive impairment of normal hematopoiesis due to continued fibroblastic proliferation, which ultimately produces sclerosis of the bone marrow and myelofibrosis. 5, 23, 51 The panproliferative process produces increased connective tissue proliferation, also in the liver, spleen, and lymph nodes, and concomitant proliferation of hematopoietic elements in the spleen, liver, and long bones. Myeloid metaplasia is closely related to polycythemia vera, myelocytic (myelogenous) leukemia, and essential (idiopathic) thrombocytosis and with these conditions constitutes a disease spectrum termed myeloproliferative disorders. Characteristic features of myeloid metaplasia are (1) progressive fibrosis of the bone marrow, (2) extramedullary hematopoiesis, (3) presence in the peripheral blood of immature erythroid and granulocyte precursors (leukoerythroid response), and (4) massive splenomegaly. In some patients the enlarged spleen provides an expanded vascular space with an associated increase in plasma volume. By serving as a shunt, the enlarged spleen may result in a decreased peripheral vascular resistance and an increased cardiac workload. Portal hypertension with varices and ascites may develop in some patients from hepatic fibrosis, increased forward blood flow through the splenoportal system, or a combination of these factors. Most patients are middle-aged or older and have symptoms related to anemia and splenomegaly. Malaise, dyspnea, and weight loss are common, and symptoms due to splenomegaly include abdominal fullness and discomfort, early satiety, and intermittent pain from splenic infarction. Less common symptoms include episodes of spontaneous bleeding, recurrent infections, bone pain, pruritus, and complications of hyperuricemia. Splenomegaly due primarily to extramedullary hematopoiesis is invariably present, and myeloid metaplasia (myelofibrosis) has been responsible for some of the largest spleens the authors have encountered (Fig. 36–12 Fig. 36–12). Hepatomegaly is present in 50% to 75% of the patients. The peripheral blood smear characteristically shows immature red cells, anisocytosis, poikilocytosis, and numerous teardrop and elongated shapes. Most patients have a mild normochromic anemia that worsens as myelofibrosis progresses. The white blood cell count is usually depressed but may reach levels of 50,000 per cu. mm. or higher. Immature granulocyte forms are present, and these, along with the red cell abnormalities, constitute a leukoerythroblastic anemia. A normal platelet count is present in 25% of patients, and thrombocytopenia occurs in approximately one third. Thrombocytosis of over 1 million per cu. mm. occurs in 25% of the patients. The leukocyte alkaline phosphatase score is usually normal or high. Hyperuricemia is present frequently and should be anticipated to avoid episodes of gouty arthritis and renal calculi. Bone marrow biopsy reveals varying degrees of fibrosis with scattered foci of hematopoietic elements. Treatment of patients with myeloid metaplasia is directed toward the anemia, thrombocytosis, and splenomegaly and includes blood transfusions, corticosteroid and androgen therapy, chemotherapy (busulfan, hydroxyurea), and splenic irradiation. Hydroxyurea is of great value in rapidly reducing and controlling the marked thrombocytosis associated with this disease. In addition, hydroxyurea may be beneficial in slowing development of splenomegaly. Splenectomy is effective in controlling anemia and thrombocytopenia and relieving symptoms due to painful or massive splenomegaly. 51 Splenectomy should be performed early rather than late in the course of the illness, because the risk of complications after splenectomy increases with progression of the disease. Indications for splenectomy are (1) an increasing transfusion requirement, (2) thrombocytopenic bleeding episodes, (3) symptomatic splenomegaly, (4) high output cardiac failure, and (5) portal hypertension with bleeding varices. 23, 42, 51 Although the course of myeloid metaplasia is not altered by splenectomy, certain prognostic factors are associated with favorable long-term survival. These include a hemoglobin level greater than 10 gm. per 100 ml., a platelet count greater than 100,000 per cu. mm., a normal leukocyte alkaline phosphatase score, and a spleen weighing less than 3,000 gm. Loss of the spleen as a major site of extramedullary hematopoiesis rarely has an adverse influence on the hematologic status of patients with myeloid metaplasia. Morbidity and mortality rates after splenectomy, however, are significantly higher for patients with myeloid metaplasia than for patients with other hematologic disorders. In advanced disease, the patients are in poor general condition, and the risk of postoperative hemorrhage and infection is great. Additionally, after splenectomy many of these patients have a marked thrombocytosis that is associated with an increased risk of thromboembolic complications that include thrombosis of the portal vein and major mesenteric veins. Specific antiplatelet therapy may be needed in the preoperative preparation and postoperative care of patients undergoing splenectomy for myeloid metaplasia. The spectrum of antiplatelet therapy includes administration of aspirin, dipyridamole, heparin, dextran, hydroxyurea, and busulfan. Hydroxyurea is especially valuable in reducing and controlling the marked thrombocytosis that can occur after splenectomy. A rapid reduction in the platelet count can be achieved by plateletpheresis (thrombocytopheresis) in patients who have thrombohemorrhagic manifestations and severe thrombocythemia. In some patients with myeloid metaplasia, there is transition to another form of myeloproliferative disorder, and in approximately 10% of patients, acute myeloid leukemic transformation occurs. The median survival after diagnosis of myeloid metaplasia is 5 years, but many patients live longer. Death usually results from hemorrhage, infection, or cardiac or renal failure. Felty's Syndrome Felty's syndrome consists of the triad of severe rheumatoid arthritis, granulocytopenia, and splenomegaly. It usually occurs in patients with a long history of rheumatoid arthritis. Patients with Felty's syndrome fail to show a substantial granulocytosis in response to infection, and severe, persistent, and recurrent infections are characteristic. Antibody directed against granulocytes is demonstrable in most patients. Mild anemia and thrombocytopenia are present in some cases. Moderate splenomegaly is common and is caused by the expansion of the red pulp. Splenectomy is effective in most patients with Felty's syndrome and should be performed in those having significant recurrent infections and chronic leg ulcers. The granulocyte response is immediate, and most patients will have resolution or significant improvement of granulocytopenia within 48 to 72 hours after splenectomy. Long-term correction of the granulocytopenia is achieved in the majority of patients with a marked reduction in the incidence of infections and healing of leg ulcerations. Controversy exists regarding the advisability of splenectomy for patients with Felty's syndrome who have severe granulocytopenia (less than 500 granulocytes/cu. mm.) but have not yet developed severe or recurrent infections. Gaucher's Disease Gaucher's disease is a disorder of lipid metabolism that may result in massive splenomegaly and hypersplenism. Genetically transmitted as an autosomal recessive trait, the disease is most commonly found in Ashkenazi Jews. Caused by a deficiency of beta-glucocerebrosidase, an enzyme responsible for breaking down certain lipid complexes, Gaucher's disease ultimately leads to retention of glucocerebroside in macrophages, especially those of the spleen, liver, bone marrow, and lungs. Diagnosis is made by finding the typical Gaucher cells in biopsied tissues. These large-diameter (20–80 mm.) cells, which contain dense fibrillar deposits of glucocerebroside in the cytoplasm, may be found in any tissue having a fixed macrophage population (e.g., bone marrow, spleen, and liver). The appearance of clinical manifestations is earliest and progression of disease is most rapid in patients having the least glucocerebrosidase activity. Of the three clinical forms of the disease, the adult form is most common. Splenomegaly, which may be massive, is usually the presenting feature and may be discovered accidentally or as a result of symptoms of early satiety, abdominal fullness, or painful infarctions. Bone pain is common due to bone destruction, which may result in collapse of vertebral bodies, pathologic fractures, and crippling. Central nervous system abnormalities are absent in the adult form of Gaucher's disease. Thrombocytopenia causes recurrent bleeding from the nose and gums, purpura, and petechiae. The infantile form, in which the central nervous system is the major site of involvement, is a much less common form of Gaucher's disease. Retarded development, early appearance of neurologic signs, seizures, hepatosplenomegaly, and cachexia are followed by death, usually before 3 years of age. The juvenile form appears during childhood and usually becomes apparent due to splenomegaly. In contrast to the adult form of Gaucher's disease, there is progressive neuronal damage and development of central nervous system abnormalities. Moderate to severe thrombocytopenia is present in most patients and is the most troublesome hematologic manifestation. Moderate normocytic anemia and leukopenia are common. Splenectomy is almost uniformly effective in correcting the cytopenias and relieves symptoms due to splenomegaly and recurring splenic infarction, although there is no evidence that splenectomy influences other aspects of the disease. Subtotal splenectomy has been performed for patients with the adult form of Gaucher's disease who have developed massive splenomegaly and hypersplenism. 20 Hypersplenism was controlled, and dramatic improvement occurred in appetite and general feeling of well being, after resection of approximately 85% of the spleen. Functioning residual splenic tissue was demonstrable postoperatively. In addition to controlling cytopenias and eliminating symptoms related to splenomegaly, subtotal splenectomy in Gaucher's disease may provide a splenic remnant large enough to afford protection against overwhelming sepsis. Cysts and Tumors of the Spleen The differential diagnosis of splenomegaly and isolated splenic masses includes cysts and primary tumors of the spleen other than systemic neoplasms of lymphoid tissue and the reticuloendothelial system. Splenic cysts and primary tumors are rare but must be considered in the differential diagnosis of a left upper quadrant mass. Cystic lesions of the spleen comprise parasitic and nonparasitic cysts. Parasitic cysts are due almost exclusively to echinococcal disease and account for 60% to 70% of splenic cysts in countries where hydatid disease is endemic (South America, Australia, and Greece). Because echinococcal disease is rare in the United States, nonparasitic cysts are encountered much more frequently in this country. Nonparasitic cysts are classified as primary or true cysts, which have an epithelial lining, and pseudocysts. Pseudocysts are much more common and probably result from liquefaction of old hematomas or areas of infarction and inflammation. True cysts of the spleen are very rare and include epidermoid and dermoid cysts, cystic hemangiomas, and cystic lymphangiomas. Symptoms of splenic cysts are vague and are caused primarily by mass effect, compression of adjacent viscera, and diaphragmatic irritation. Although selected nonparasitic cysts may be effectively managed by aspiration, splenectomy should be performed for all large cysts and those with uncertain diagnosis. In some patients a splenic cyst may be suitably located for excision by partial splenectomy. Intraoperative drainage may facilitate dissection and splenectomy for very large cysts. External drainage and marsupialization have an unacceptable incidence of infection, bleeding, and cyst reaccumulation and are inappropriate techniques for management of splenic cysts. Malignant and benign primary tumors of the spleen are rare. Most primary malignant tumors are angiosarcomas, although primary splenic lymphoma may occur. Before primary parenchymal lymphoma is diagnosed in the spleen, the bone marrow, nodal regions, liver, and other areas must be evaluated and found to be free of disease. Benign splenic tumors include hamartomas, lymphangiomas, hemangiomas, and lipomas. Except for involvement with Hodgkin's disease and NHLs, metastatic disease to the spleen is diagnosed infrequently. The spleen's effective filtering mechanism and high blood flow suggest that the spleen would develop metastatic lesions more often. Although spleens from patients dying of metastatic tumors frequently reveal malignant cells, metastatic deposits are rare. Studies in rodents have confirmed that metastatic tumors rarely develop in the spleen after injection of tumor cells into the splenic artery. It is probable that the splenic immune mechanisms that so efficiently destroy abnormal red cells also eliminate the majority of metastatic tumor cells that are trapped in the red pulp. Splenic Vein Thrombosis Since the pathophysiology of splenic vein thrombosis was first elucidated 50 years ago, this uncommon cause of upper gastrointestinal variceal hemorrhage has been found to be eminently curable by splenectomy. 6 Pancreatitis is the cause of splenic vein thrombosis in more than half of the reported cases. Other causes include pancreatic carcinoma, pancreatic pseudocyst, penetrating gastric ulcer, retroperitoneal fibrosis, and myeloproliferative disorders. 6 The underlying disease produces thrombosis of the splenic vein with subsequent development of venous collateral channels. Because the collateral pathways are usually the short gastric veins to the submucosal venous plexus of the gastric cardia and fundus, gastric varices develop. Splenic vein thrombosis should be suspected in a patient with upper gastrointestinal hemorrhage, isolated gastric varices on endoscopy, and a history of pancreatitis or pancreatic cancer. Splenomegaly is variable, and if present it is not associated with other stigmata of cirrhosis. Anemia is usually present, but tests of liver function are normal. Definitive diagnosis is made by celiac angiography, which demonstrates absence of the splenic vein. Splenomegaly may be noted along with venous collaterals in the splenic hilus. Splenectomy is curative and eliminates the increased blood flow through collaterals to the gastric venous plexuses. Although there are no studies that have followed the course of asymptomatic patients with splenic vein thrombosis, it seems prudent to consider splenectomy if this diagnosis is made. RARE SPLENIC DISORDERS Wandering (Ectopic) Spleen. Congenital deficiency or acquired laxity of the suspensory ligaments of the spleen may cause extreme splenic mobility. This rare condition, which is termed wandering or ectopic spleen, permits a normal-sized spleen to be palpable in the lower abdomen or in the pelvis. The majority of cases of wandering spleen have occurred in young and middle-aged women in whom multiparity and laxity of the abdominal wall and splenic ligaments due to the hormonal effects of pregnancy have been cited as predisposing causes. A wandering spleen may be an incidental finding on physical or radiographic examination. An elongated splenic pedicle predisposes a wandering spleen to torsion, leading either to development of acute symptoms due to splenic volvulus and infarction or to chronic and intermittent abdominal discomfort due to spontaneous torsion and detorsion. Useful diagnostic tests in the patient who is asymptomatic or has chronic and recurring symptoms include abdominal CT or ultrasonography, a splenic radionuclide scan, and visceral arteriography. Splenic volvulus with infarction requires emergency splenectomy. Selected asymptomatic patients and those with chronic and recurring symptoms may sometimes be managed successfully by splenopexy, which preserves splenic function and avoids the potential danger of postsplenectomy sepsis. Splenic Artery Aneurysm. Aneurysms of the splenic artery are rare and occur more frequently in females, in whom the most common etiology is medial dysplasia of the arterial wall. Atherosclerosis accounts for the majority of splenic artery aneurysms in males. Additional causes include focal arterial injury due to pancreatitis, trauma or arteritis due to septic emboli, portal hypertension with splenomegaly, and an ill-defined pathogenesis associated with multiparity. Most splenic artery aneurysms are asymptomatic, and characteristic eggshell calcification of an arteriosclerotic aneurysm may be an incidental finding on an abdominal radiograph. When symptoms are present, they are variable and consist primarily of vague left upper quadrant discomfort. Aneurysmal rupture may occur, and the rupture initially may be contained within the lesser sac. Initial aneurysmal rupture into the peritoneal cavity or delayed rupture from the lesser sac are associated with findings of hemoperitoneum and exsanguinating hemorrhage. Rarely, a splenic artery aneurysm ruptures into the gastrointestinal tract, pancreatic duct, or splenic vein. The mortality with a ruptured splenic artery aneurysm remains high. Excision of the aneurysm is advisable for symptomatic aneurysms and for asymptomatic aneurysms in patients who are acceptable operative risks. This is especially important for women of childbearing age who have an increased propensity for aneurysmal rupture during pregnancy. Elective operation has a low risk of mortality and minimal morbidity. In the treatment of splenic artery aneurysm, the spleen should be preserved if possible. Splenic Abscess. Splenic abscess occurs rarely and usually results from (1) bacteremia associated with a primary septic focus such as bacterial endocarditis or lung abscess or (2) secondary infection in an area of the spleen damaged by infarction (sickle cell anemia or leukemia), trauma, or parasitic infestation. Clinical features of splenic abscess are those of left subphrenic suppuration and include fever, chills, left upper quadrant tenderness, and often splenomegaly. Imaging techniques (ultrasonography and radionuclide and CT scans) are useful in differentiating splenic abscess from left subphrenic abscess and in determining whether there is a single abscess or multiple abscesses within the spleen. CT is probably the most direct way of evaluating the spleen and establishing an early diagnosis. Splenectomy has been the preferred treatment for most patients in the past and remains a standard means of safe and rapid management. Splenotomy and abscess drainage may be advisable for selected patients with a single abscess and extensive adhesions between the spleen and adjacent structures. Image-guided percutaneous drainage may be appropriate in the management of some patients with splenic abscess. Percutaneous drainage is most likely to be successful, if the abscess is unilocular and if the abscess contents are amenable to complete evacuation by an in-dwelling suction catheter.