Gastro Esophageal Reflux Disease GERD
advertisement

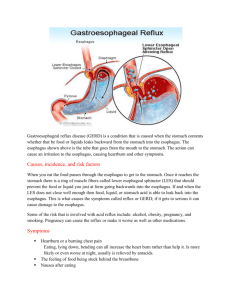
Gastro Esophageal Reflux Disease GERD Almost everyone has experienced heartburn. About 25 million American adults suffer daily from heartburn. It is that burning sensation felt behind the breastbone and sometimes in the neck and throat. Heartburn is caused by stomach acid refluxing or splashing up into the esophagus -- the muscular tube that connects the throat to the stomach. Occasional heartburn is nothing to be concerned about. However, anyone who has heartburn on a regular basis should consult a physician. Constant exposure to stomach acid can irritate the lining of the esophagus and cause other medical problems. Serious heartburn is known as gastroesophageal reflux disease or GERD. What is GERD? The esophagus carries food and liquid into the stomach. At the lower end of the esophagus where it enters the stomach, there is a strong muscular ring called the lower esophageal sphincter (LES). The LES should remain tightly closed, except to allow food and liquid to pass into the stomach. Reflux occurs when the LES is not working properly. It may relax for periods of time throughout the day and night, or it may be constantly too weak to function effectively. This allows the stomach's acid juices to flow into the esophagus. How severe the disease becomes depends on how weakened the LES is, and the amount and duration of acid refluxed into the esophagus. It is also common to find a hiatal hernia complicating GERD. With a hiatal hernia, the upper part of the stomach actually pushes up into the chest through a weakness in the diaphragm. The diaphragm is the thin, flat muscle that separates the lungs from the abdomen. When part of the upper stomach is stuck above the diaphragm, stomach acid is retained there for a longer period and is more likely to reflux into the esophagus. Symptoms and Causes of GERD Frequent heartburn is the most common symptom. However, patients may also experience some of the following: sour or bitter taste bitter stomach fluid coming into the mouth, especially during sleep hoarseness repeatedly feeling a need to clear the throat difficulty swallowing food or liquid wheezing or coughing at night worsening of symptoms after eating, or when bending over or lying down. Certain diet and lifestyle choices can contribute to the condition. For example, certain foods increase acid production, and fatty foods increase the time food remains in the stomach. Chocolate, peppermint, coffee, alcoholic beverages, and especially nicotine in cigarette smoke weaken or relax the LES. Obesity places added pressure on the upper abdomen, and during pregnancy the LES weakens for unknown reasons. Complications Complications occur when GERD is severe or long-standing. Constant irritation of the esophagus by stomach acid can lead to inflammation, ulcers, and bleeding. Anemia or low blood count may develop. Over time, scarring and narrowing of the esophagus can also develop, making it difficult to swallow foods and liquids. This narrowing is called a stricture. Some patients develop a condition called Barrett's esophagus, which is a serious change in the cells lining the esophagus. Barrett's esophagus may be a forerunner of esophageal cancer. Diagnosis of GERD The diagnosis can usually be suspected by the physician, simply by taking the medical history. Beyond that, the physician may order an x-ray examination of the esophagus and stomach. For this x-ray, the patient swallows a liquid containing barium. This makes it possible to see the reflux and a hiatal hernia on the x-ray. Endoscopy is the most important test for patients with GERD. It is done with the patient under sedation. The physician examines the lining of the esophagus and stomach with a thin, lighted, flexible tube called an endoscope. This exam is helpful in determining how severe the disease is, how much tissue damage there is, and if there are any complications. Certain conditions, such as narrowing or stricture in the esophagus, can usually be corrected during this procedure. During an endoscopy, the physician can also look for signs of Barrett's esophagus, and perform a biopsy to see if precancerous changes have occurred. There are other tests that are helpful. A pressure recording of the esophagus is called esophageal manometry. It measures the pressure in the LES and any abnormal muscle contractions in the main part of the esophagus. Finally, a 12 to 24 hour recording of the acidity in the esophagus is often helpful. What is the treatment? Treatment is aimed at reducing reflux and damage to the lining of the esophagus. Initial treatment is with lifestyle changes. Patients with GERD should follow these recommendations: Avoid eating anything within three hours before bedtime. Stop smoking. Nicotine in the blood weakens the LES. Avoid fatty foods, milk, chocolate, spearmint, peppermint, caffeine, citrus fruits and juices, tomato products, pepper seasoning, and alcohol -- especially red wine. Decrease portions of food at mealtime, and avoid tight clothing or bending over after eating. Review all medications with the physician. Certain drugs can weaken the LES, allowing acid irritation of the esophagus. Elevate the head of the bed or mattress 6 to 8 inches. This helps to keep acid in the stomach by gravity when sleeping. Extra pillows by themselves are not very helpful. Lose weight if overweight. This may relieve upward pressure on the stomach and LES. Lifestyle changes are often all that is needed to correct mild forms of GERD. When symptoms are bad or GERD is moderate to severe, the physician will prescribe medications. Some that reduce stomach acid include Tagamet, Zantac, Pepcid and Axid. Certain potent newer drugs, such as Prilosec and Prevacid, can almost eliminate stomach acid entirely. These two drugs are most frequently used when GERD is severe. Other medications, such as Reglan (generic: metoclopramide) tighten the LES. These may be especially useful at night when reflux often occurs. A number of patients with GERD may need surgery to strengthen the LES. This procedure is called fundoplication. Previously this surgery required a major operation, often through the chest. It is a difficult operation for the patient, with a long recovery. It is now usually done by laparoscopy. This is a new type of minimally invasive surgery, performed with a tiny incision at the naval and a few needle points in the upper abdomen. The patient usually returns home 1-2 days after surgery, with few problems. Surgery, however, should not be considered until all other measures have been tried. Surgery is often seriously considered for an otherwise healthy patient when the disease is severe, or the patient does not want to face the expense or regimen of long-term treatment with medications. Summary GERD is a common problem that requires medical attention when symptoms and tissue damage become troublesome. Fortunately, there is a great deal that can now be done about GERD. Lifestyle changes can help, and there are many medications and even surgery to treat and correct GERD. Working together with the physician, a good medical program can almost always be developed to successfully treat the patient with GERD. Gastroesophageal Reflux Disease Diet Purpose The esophagus is the tube that carries food from the throat to the stomach. However, it is not just a simple tube. The lower esophagus has a specialized muscle around it that usually stays tightly closed, opening only to allow food and liquid into the stomach. It acts to prevent the reflux of stomach acid into the esophagus. Symptoms occur when this specialized muscle weakens and allows stomach acid to splash up into the esophagus. These symptoms include heartburn, chest discomfort, and bitter fluid flowing up into the mouth. Chest discomfort can occur. If the stomach juice trickles into the breathing tubes, hoarseness, cough, and even shortness of breath can occur. This entire problem is called GERD (Gastroesophageal Reflux Disease). A number of factors, including certain foods, may cause the lower esophageal muscle to relax, causing GERD. Nutrition Facts A diet designed to prevent or reduce acid reflux is usually easy to follow. The basic food groups of cereals, vegetables, fruits, dairy products, and meats can be eaten with only a few limitations. So, this diet generally meets the Recommended Dietary Allowances (RDA) of the National Research Council. A vitamin C supplement may be needed if an individual does not tolerate citrus foods such as orange, tomato, etc. Special Considerations The lower esophageal muscle can be weakened by factors other than food. The following recommendations may be helpful in reducing symptoms: 1. Stop using tobacco in all forms. Nicotine weakens the lower esophageal muscle. 2. Avoid chewing gum and hard candy. They increase the amount of swallowed air which, in turn, leads to belching and reflux. 3. Do not lie down immediately after eating. Avoid late evening snacks. 4. Avoid tight clothing and bending over after eating. 5. Eat small, frequent portions of food and snack if needed. 6. Lose weight if overweight. Obesity leads to increased reflux. 7. Elevate the head of the bed six to eight inches to prevent reflux when sleeping. Extra pillows, by themselves, are not very helpful. 8. The following foods aggravate acid reflux, and should be avoided: o fatty or fried foods o peppermint and spearmint o whole milk o oils o chocolate o creamed foods or soups o most fast foods 9. The following foods irritate an inflamed lower esophagus and may need to be limited or avoided: o citrus fruits and juices (grapefruit, orange, pineapple, tomato) o coffee (regular and decaffeinated) o caffeinated soft drinks o tea o other caffeinated beverages 10. Spicy or acidic foods may not be tolerated by some individuals. Food Groups Group Recommend Avoid Milk or milk products skim, 1% or 2% low-fat milk; low-fat or fat-free yogurt whole milk (4%), chocolate milk Vegetables all other vegetables fried or creamy style vegetables*, tomatoes Fruits apples, berries, melons, bananas, peaches, pears citrus*: such as oranges, grapefruit, pineapple Breads & grains all those made with low-fat content any prepared with whole milk or high-fat Meat, meat substitutes low-fat meat, chicken, fish, turkey cold cuts, sausage, bacon, fatty meat, chicken fat/skin Fat, oils none or small amounts all animal or vegetable oils Sweets & desserts all itmes made with no or low fat (less chocolate, desserts made with oils and/or than or equal to 3 g fat/serving) fats Beverages decaffeinated, non-mint herbal tea; juices (except citrus); water alcohol, coffee (regular or decaffeinated), carbonated beverages, tea, mint tea Soups fat-free or low-fat based chicken, beef, milk, or cream-based soups *Individually determined This packet was prepared for you by Dr. Aaron J. Burrows (303) 320-1111