Course Specification
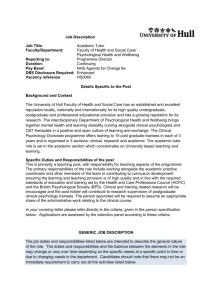
advertisement

1st Feb.2010 1. Title of programme Doctorate in Clinical Psychology by Research 2. Awarding Institution University of Hull 3. Approval/Accreditation Details Health Professional Council (HPC) British Psychological Society (BPS) 4. Name of final award Doctorate in Clinical Psychology (Successful completion of the programme confers eligibility for HPC registration as Clinical Psychologist and to apply for registration for Chartered Membership of the BPS as well as full membership of the Division of Clinical Psychology and with the British Psychological Society as full member of its Division of Clinical Psychology). 5. QAA subject benchmark - QAA subject benchmark – clinical psychology 2004 6. Aims of the Programme. 6.1 The principal aim of the programme is to produce competent clinical psychologists who are qualified for employment in the NHS and whose professional practice will conform to the high ethical and professional practice standards specified in the HPC’s and BPS’s publications: Standards of Education and Training Guidance (HPC 2009); Standards of Proficiency for Practitioner Psychologists (HPC 2009), Standards of Conduct, Performance and Ethics (HPC 2008 ), The Professional Practice Board’s Generic Professional Practice Guidelines (BPS 2007) and the Division of Clinical Psychology publications as supportive advice and appendices to the Professional Practice Board Guidelines . 6.2 The distinctive characteristics and competencies of clinical psychologists have been defined in a series of documents (HPC Standards of Education and Training Guidance; HPC Standards of Proficiency for Practitioner Psychologist; MAS and MPAG Reports; CTCP Accreditation Criteria; QAA Benchmark Statement for Clinical Psychology; BPS National Occupational Standards for Clinical Psychology, Quality Assurance Framework for Higher 1 Education Qualifications). The programme seeks to produce clinical psychologists who are fit for purpose, that is individuals who: who have the competences and capability which meet the needs of the local and national health service; who are steeped in its culture and values; who are aware of the policies and processes by which these are implemented; who are motivated to remain up-to-date with NHS policy development. 6.3 The programme's unifying orientation is the application of scientific knowledge to the understanding and treatment of psychological problems and disabilities. Trainees need to develop knowledge and the ability to evaluate critically the current literature relating to a particular type of problem, including the empirical and experimental evidence for and against the use of a given intervention. By the end of the programme, trainees will have: a good mastery of cognitive behavioural therapy and systemic therapy plus the knowledge and understanding of a range of psychological clinical models applicable to individual, family and group work; knowledge and understanding of issues relating to diversity and differences; multi-theoretical formulation skills (which include formulation about systems and organisations as well as individuals) which draw from a broad range of theoretical models, across client groups of different backgrounds and abilities, across a variety of settings and ranging from individual work to group work and family work; the ability to apply their knowledge and skills to a variety of clinical problems in terms of assessment and formulation; the ability to apply their knowledge and skills to develop effective interventions and to evaluate these within an appropriate methodological framework; knowledge of research methods in clinical psychology and an ability to apply these to NHS R&D priorities; the skill to manage a continual professional learning agenda to acquire clinical knowledge, the maintenance of current awareness of the everevolving knowledge base of the profession and an ability to implement evidence-based practice; the skill to be a reflective practitioner who has critical self-awareness; the ability to consider the psychological, emotional and behavioural impact on the self of clinical and personal experiences, both during and following clinical encounters. 7. Programme outcomes. 7.1 The outcomes of this programme – the competencies required by a clinical psychologist – are achieved through the integration of the four main 2 ‘strands’ of the programme, which are academic; clinical practice under supervision; research; and personal and professional development. 7.2 The HPC’s Standards of Proficiency and the BPS Committee of Training in Clinical Psychologists’ list of nine high-level summaries of the required objectives and competences (general and transferable skills, psychological assessment, psychological formulation, psychological intervention, evaluation, research, personal and professional, communication and teaching and services and organisations) form the outcomes of the programme. Based on these standards of proficiency by the HPC and the nine competencies listed by the BPS Committee of Training in Clinical Psychology (CTCP), seven main teaching bundles are formed. These bundles focus on helping trainees to develop the following competencies. I. Therapeutic relationships and self awareness Trainees will have developed: an understanding of key issues in therapeutic relationships e.g. boundaries; an appreciation of the inherent power imbalance between practitioners and clients and how abuse of this can be minimised; the ability to use formulations with clients to facilitate their understanding of their experience; the ability to recognise when (further) intervention is inappropriate, or unlikely to be helpful, and to communicate this sensitively to clients and carers; strategies to handle the emotional and physical impact of their own practice and to recognise the need for and to seek appropriate support when necessary, with good awareness of boundary issues; their skills in managing their own personal learning needs and strategies for meeting these; an understanding of the supervision process for both supervisee and supervisor roles. II. Clinical Skills Trainees will have developed competence in: developing and maintaining effective working alliances with clients, including individuals, carers and services; choosing, using and interpreting a broad range of assessment methods; conducting appropriate risk assessment and using this to guide practice; making formulations of presenting problems or situations, drawing on a range of psychological models and using them appropriately; 3 using formulations to plan appropriate interventions that take the client’s perspective into account; implementing appropriate psychological interventions (following from a formulation) directly or indirectly with individuals, groups or services; revising formulations in the light of ongoing intervention and when necessary re-formulating the problem; communicating effectively clinical and non-clinical information from a psychological perspective in a style appropriate to a variety of different audiences (e.g. to professional colleagues, and to users and their carers); adapting style of communication to people with a wide range of levels of cognitive ability, sensory acuity and modes of communication; preparing and delivering teaching and training which takes into account the needs and goals of the participants (for example by appropriate adaptations to methods and contents). III. Practice Based Knowledge & Applications Trainees will have developed competence in: deciding, using a broad evidence and knowledge base, how to assess, formulate and intervene psychologically from a range of possible models and modes of intervention with clients, carers and service systems; developing formulations of presenting problems or situations which integrate information from assessments within a coherent framework that draws upon psychological theory and evidence and which incorporates interpersonal, societal, cultural and biological factors; IV. Ethical Practice, Values & Professional Issues Trainees will have established: understanding of the ethical foundations of clinical psychology practice; awareness of issues within the profession and of personal development procedures; awareness of the role of values in clinical practice; understanding of ethical issues and applying these in complex clinical contexts, ensuring that informed consent underpins all contact with clients and research participants; understanding of the impact of difference and diversity on people’s lives, and its implications for working practice; And trainees will have developed competence in: 4 working effectively, at an appropriate level of autonomy, with awareness of the limits of own competence and make appropriate referrals to other professionals; accepting accountability to relevant professional and service managers; V. Disciplined Enquiry Trainees will have: developed an understanding of research design, methodology, analysis and dissemination; gained insight into the role and use of the audit cycle in the NHS; developed knowledge about conducting service evaluation/audit and small N research; developed knowledge about selecting and implementing appropriate methods to evaluate the effectiveness, acceptability and broader impact of interventions (both individual and organisational), and using this information to inform and shape practice; Trainees will have developed competence in: identifying and critically appraising research evidence relevant to practice; conducting service evaluation/audit or small N research; conducting collaborative research; planning and conducting independent research i.e. identifying research questions, demonstrating an understanding of ethical issues, choosing appropriate research methods and analysis, reporting outcomes and identifying appropriate pathways for dissemination; VI. NHS Context & Professional Relationships Trainees will have developed competence in: working with users and carers to facilitate their involvement in service planning and delivery; consultancy models and the contribution of consultancy to practice; working collaboratively and constructively with fellow psychologists and other colleagues and users of services, respecting diverse viewpoints; working effectively in multi-disciplinary teams; using formulations to assist multi-professional communication, and the understanding of clients and their care; 5 VII. processes of change in service delivery systems and appropriate interventions to facilitate this; Integration through Reflection Trainees will have developed the competencies to: a. generalise and synthesise prior knowledge and experience in order to apply them in different settings and novel situations; b. make use of self-awareness in their clinical and research work; c. work as a reflective practitioner; d. think critically, reflectively and evaluatively; e. use supervision to reflect on practice and make appropriate use of feedback received; 8. Teaching, Learning and Assessment methods used to enable outcomes to be achieved and demonstrated 8.1 Teaching and learning in all four ‘strands’ of the Course is based upon a progressive learning model. The competencies acquired in the first year of clinical training provide the basis for those learned in the second year, and in turn, those in year two for year three competencies. 8.2 Trainee clinical psychologists are salaried employees of the NHS and are regarded as junior colleagues. Teaching is designed and delivered for adult learners, who need to acquire the skills for continuous learning throughout their professional career. A variety of teaching / learning formats is used, including: Lectures; workshops; small group discussions; trainee clinical case presentations; independent study; individual and group supervision of both clinical and research activity. 8.3 Teaching and learning take place both in the University and in clinical practice settings. Although the formal programme of teaching is presented in the University, there is provision, in NHS and other service settings, of learning opportunities to acquire competence in clinical practice and research and to foster personal and professional development. 8.4 Much of the teaching of the formal programme is delivered by practising clinician psychologists, who are encouraged to include case material in their 6 presentations to further the integration of theory and practice. Teaching and learning on practice placement is delivered and consolidated through clinical supervision. Teaching is synchronised with placements at all stages of training. 8.5 The extensive course handbook enables clinical supervisors, ‘field’ research supervisors and clinician teachers to have an overview of the totality of the four ‘strands’ of the programme and the position of their contribution within it. 8.6 Assessment methods have been designed to meet the HPC and BPS requirements for assessments of trainee competence at intervals throughout the programme. The detail of these is set out in the programme handbook section on trainee evaluation and in a separate timeline table. 8.7 The assessments are thus related to programme outcomes and take a variety of forms including: written case studies; a research report for small scale (service-related/audit) research project; research reports for main research project; clinical literature review; supervisor evaluations of practice; clinical practice evaluations by course staff unseen and open-book examinations. 8.8Performance on assessments is clearly linked to progression on the programme. Trainee performance on three major components of the Course (taught academic syllabus, clinical placement work and research) is assessed independently. Trainees must achieve a “pass” standard on each piece of work in each component to complete the Course. 8.9The Course does not give credits for prior (experiential) learning. Students will need to pass all the requirements of the Course in order to gain the doctoral degree. 8.10There are no exit qualifications at a lower level. For example candidates who fail the course will not be able to gain a masters degree or a diploma because they passed certain components of the Course. 8.11The CTCP’s list of nine competencies form the outcomes of the programme. See diagram 1 for the link between assessment and competences. In addition to these summative assessments, there are a number of formative assessments throughout the programme. 7 Diagram 1: Matrix showing the link between assessment and competence Nine competencies 1. General, transferable 2. Assessment 3.Formulation Psychometric skills Critical appraise the problem presented and decide on the appropriate psychometric tests Critical evaluation of theory & evidence from literature, to synthesise and formulate clinically related questions 4.Intervention 5.Evaluation 6.Research 7.Personal, professional 8.Communication & Teaching YEAR 4 ASSESSMENTS 1. Psychometric compendium (Formative but trainees have to pass) 2. Clinical Literature Review Literature search skills, applying knowledge & critical evaluation 3. 1:1 Case study Reflectivity & applying knowledge Working alliance & other modes of assessment 4. Clinical Practice Evaluation 5.Compendium Exam Reflectivity Working alliance & interview and assessment skills Application of knowledge to novel situations Demonstration knowledge of risk assessment and of various modes of assessment Appraising the evidence in the light of theory to develop new questions that contribute to new psychological knowledge Formulation development; plan intervention & communicate Formulation and reformulation Implementing intervention Ability to demonstrate what information required to develop a formulation Demonstrate of broad accurate theoretical and clinical knowledge base which can be used to determine appropriate intervention Selecting methods of evaluation Effectively targeting written communication Power issues, informed consent, boundaries Written communication and professional correspondence Verbal presentation skills Professional ethics, power, difference & diversity Demonstrate an understanding of requirement to adapt communication Intervention planning 8 Research ethics 9.Services & organisation YEAR 5 ASSESSMENTS 6. MDT case study Reflectivity & applying knowledge Formulation development; plan intervention & communicate Implementing intervention through others Selecting methods of evaluation Professional roles, informed consent, boundaries Working alliance with MDT members 7. MDT rating 8. Small scale research project Working alliances & other modes of assessment Applying research into practice, thinking critically, evaluatively and reflectively Applying knowledge Showing knowledge of modes of assessment 10. Clinical Practice Evaluation Reflectivity Demonstrating knowledge of risk assessment and of various modes of assessment s Understanding context, consultative & MDT skills, MDT contribution Effectively communicating research information relevant to audience Showing understanding of and contributing to organisational context Professional roles Selecting methods of evaluation & effectiven ess audit 9a. Fifth year exam – Paper 1 9b. Fifth year examine – Paper 2 Written communication and professional correspondence Ability to demonstrate what information is required to develop a formulation and to hypothesise possible formulations from limited information Formulation with systemic focus. Intervention planning Demonstration of accurate theoretical and clinical knowledge base which can be used to determine appropriate interventions. Recognising when intervention is not indicated Development of MDT care package 9 Selecting methods of evaluation Selecting outcome measures Planning conducting and implementing small scale service orientated or audit research Professional ethics, power, difference & diversity, boundaries Professional roles Understanding of the therapeutic relationship Professional ethics, power, difference & diversity, boundaries Understanding context & organisational change Verbal presentation skills YEAR 6 ASSESSMENTS Critical appraisal of the problem presented and choice of and interpretation of appropriate psychometric tests 11. Psychometric case study 12. Systematic literature review Thinking critically and evaluatively 1 3. Reseach portfolio Journal articles ( one based on main research project and one systematic literature review) 14. Research Viva Thinking critically and evaluatively Formulation of problem on basis of full assessment and communication of formulation to appropriate parties. Intervention flowing from formulation Critique of case studyability to critically appraise own work Written communication And professional report writing Thinking critically and systematically do literature search; evaluate evidence and argue cogently ; writing for a peerreviewed journal Thinking critically and systematically; data collection and analyses;; writing for a peerreviewed journal Thinking critically and evaluatively Effectively communicating information to relevant audience Reflection on research process Effectively communicating research information relevant to audience Effectively communicating research information relevant to audience 10 9. Programme structure 9.1 The programme is continuous over three calendar years, beginning in September. As salaried NHS employees, trainees receive an annual leave allowance but this cannot be taken during university teaching days. Attendance at the university and on placement is compulsory. Over half the available time is spent in supervised clinical practice, with the remainder split equally between the formal academic programme on the one hand and research and private study on the other. 9.2 Teaching, clinical experience and research training are all within a developmental framework of individual work, team and system work and finally specialisation. There is an emphasis throughout on developing transferable skills. Trainees are expected to demonstrate competences according to the developmental model. Close working with NHS colleagues ensures close integration and most programme staff work as NHS clinicians. NHS clinicians, mostly clinical psychologists, provide the bulk of the teaching on the programme. Teaching is synchronised with placements at all stages of training. 9.3 Generally, postgraduate trainees spend 3 days a week on clinical placement (Monday, Tuesday, Wednesday) and 2 days a week at the University (Thursday, Friday). In the final year of clinical training, trainees spend Tuesday, Wednesday and Thursday on clinical placement and Friday and Monday for academic work, including research. During Semester time, alternative Friday mornings are devoted to research seminars, examination of clinical issues and case conferences, in which trainees in rotation present confidential case-material from their work on placement. Clinical workshops and lectures take place on academic days. 9.4 The first year of clinical training begins with a nine-week teaching block during which trainees are provided with an induction to employment in the NHS and extensive practical skill-based workshops to prepare them for their first clinical placement. The emphasis during this teaching block is on 1-1 working with individuals across the lifespan and ability range, in preparation for the placements in the remainder of year four. 9.5 The fifth year begins with a four-week teaching block, which prepares trainees for indirect work and working within a multi-disciplinary setting during their placements that year. 9.6 Following a four week teaching block, the final year consists normally of two elective specialist placements lasting for five and a half months each, determined partly by trainee preference, in consultation with the placement co-ordinator. Trainees often elect to undertake placements in centres of excellence which may be of some considerable distance from Hull University. Occasionally this may include an overseas placement. 9.7 The system of placement planning and allocation is described below. Supervised clinical practice is organised within individual training pathways, 11 which are fixed for the first two years of training. In the first year of clinical training placements are structured to facilitate the development of competencies in 1:1 working and fifth year placements provide the opportunity to experience multi-disciplinary and indirect methods of working. Sixth year elective placements are designed to consolidate core competencies and provide further clinical experiences, often in more specialised settings. 9.8 The research programme is organised by a staff research group led by the Research Coordinator. It operates in the context of a Departmental Research Strategy, which is strongly focussed on ongoing research by academic staff who act as supervisors for the large-scale trainee research project. It aims to equip and motivate trainees with a broad range of knowledge and skills, thus enabling them to become effective and productive scientist-practitioners of evidence-based research methods in typical areas of clinical psychology. It also provides the skills required to enhance areas of research-methods and competence in future clinical psychological careers, as part of continuing professional development. 9.9 In addition to the Large-Scale Research Project, the Small-Scale Research Project -SSRP (used to be known as Placement Based Project) is also part of the research programme. The Small-Scale Research Project is set in the NHS with placement supervisors suggesting topics (and providing supervision) that are of interest to the placement and supervisors in service provision. The remit of the SSRP is to either answer the question “What standard does the current service achieve (Service Evaluation) or “Does this service reach a predetermined standard” (Clinical Audit). The aim of the SSRP is to give hands-on experience of research rather than to generate generalizable new knowledge. Teaching and qualitative or statistical analysis support to conduct the SSRP, is available to the Trainee from the Department. 10 Support for learning 10.1 The University Department of Clinical Psychology is located within the Post Graduate Medical Institute in a self-contained suite which includes 4 well-appointed, dedicated clinical teaching laboratories and 1 additional seminar room. The Department has exclusive use of audio-visual teaching equipment and possesses an extensive clinical test library. There is easy access to the main University library, the Graduate Research Institute (GRI), the Department of Psychology (Fenner Building and Applied Science 3), the University bookshop and the Students Union. To obtain copies of material not held in the University library there is a Document Supply Service. Trainees also have access to eBridge, a web-based virtual learning environment which can be accessed from anywhere with an internet connection using a web browser. This enables access to electronic versions of course materials and guidance documents. 12 Whilst on clinical placement, trainees have access to NHS libraries and to the NHS online National Library for Health. The placements meet the minimum standards that each trainee has access to a desk and a telephone. Laptop computers are available from the University if no computer is available on placement. 10.2 At the beginning of the programme, the trainee is allocated a personal tutor who is a member of the clinical academic staff of the University. It is expected that the personal tutor and student will meet at least once a semester in order to discuss academic and personal progress and/or difficulties. It is the tutor who usually carries out an annual individual performance development review with the trainee. The personal tutor can also acts as the student's advocate if the student is the subject of University disciplinary procedures, appeals, official inquiries and other difficulties. 10.3 In addition to personal tutors, the following mechanisms are in place: a mentor system via which trainees can seek support confidentially from practising psychologists via a co-ordinator in the NHS. The coordinator or the mentor will not inform the Course Team about any contacts. This system ensures that trainees can seek additional supports without any risk of prejudice to the trainees’ standing on the Course; a buddy system for the appropriate peer bonding and support; a research tutor who has expertise in the trainee’s proposed major research project. A clinical tutor who oversees the trainees placement experience, acts as a link person between the course and supervisor and provides additional tutorial input to trainees if required. 10.4 It is expected that the clinical supervisor of each placement will offer, but not impose, supervision which will encompass personal issues and personal development. 10.5 The programme has access to two independent sources of support for trainees who develop personal or mental health problems. These are the University Counselling Service and the employing Trust’s occupational health service. 11 Methods for evaluating and improving the quality of teaching and learning. 13 11.1 Programme Committees All of the programme’s committees have a role in the monitoring and improving the quality and content of the programme. Most of the committees include significant NHS psychologist and trainee representation. In particular, the Academic Syllabus Committee, the Clinical Placements Committee and the Trainee Research Committee review routinely all aspects of each of the three component strands of the Course. 11.2 Teaching Quality Assurance It is University policy that all courses should be subject to TQA procedures and such procedures are an integral part of the doctorate programme. All academic aspects of the programme are reviewed, where feasible immediately on completion. The Academic Syllabus Co-ordinator has responsibility for the design of electronic TQA feedback questionnaires which trainees complete. All responses remain anonymous: completed forms are received in confidence by the Programme Manager who collates numerical ratings and written comments in typed form. All feedback is processed by the Academic Team and the Programme Manager reported feedback to individual staff and external lecturers to whom the comment and ratings apply. Where there is persistent and consensual criticism, steps are taken to remedy the difficulty. TQA procedure also applies to placement learning. 11.3 The External Examiner's Report At the end of each academic year, a Board of Examiner's meeting takes place at which assessed work from all three postgraduate years of the programme is reviewed by the External Examiner and the Course staff. Subsequently the External Examiner provides a written report on the quality of work submitted and general standards of the programme. This report is included in the Annual Report to the Purchasing Consortium of the York and Humber SHA, the Board of Management of the Course, the Graduate School and the Dean of Hull York Medical School. 11.4 Course Annual Report Each Autumn a written annual review report is made to the York and Humber SHA which commissions the programme and the Quality Office at Hull University for quality assurance purposes. 11.5 Health Professional Council (HPC) The HPC is an independent statutory regulatory body whose main aim is to protect the public. It currently regulates 14 health professions. Clinical Psychology is regulated by the HPC. It is a legal requirement that anyone who wishes to practice using the protected title “Clinical Psychologist” is on the HPC Register. When the HPC took over the regulation of clinical psychology in 2009, the Hull Clinical Psychology Doctorate Course was granted open-ended approval based on the status of our programme’s accreditation with the BPS. Successful completion of this Course provides 14 eligibility to apply for registration with the HPC. For more information about the HPC, please see the HPC website at: http://www.hpc-uk.org/ 11.6 The HPC does not regulate clinical psychology students. However students are expected to adhere to the HPC’s policy on professional standards described in their booklet Standards of Conduct, Performance and Ethics (HPC 2008). Guidance on Conduct and Ethics for Students (HPC 2010) has also been published. 11.7The HPC intends to visit all the practitioner psychologist programmes over a three academic year period, commencing in 2009-2010 with all visits completed by July 2012, with ongoing approval of all programmes reconfirmed by the 2012-2013 academic year at the latest. In January 2011, the HPC is scheduled to visit the University of Hull Doctorate Degree Course in Clinical Psychology. 11.8 British Psychological Society (BPS) Accreditation All clinical psychology training programmes are subject to accreditation by the BPS every five years. Accreditation teams are particularly interested in trainee and other stakeholder views of the programme. The Course enjoys full accreditation status with the BPS and the next visit is scheduled in January 2011 as a joint visit with the HPC. 11.9 Review by the Quality Assurance Agency (QAA) for Higher Education All university departments in the UK are subject to 5-yearly review by the QAA to evaluate and monitor the quality of teaching and learning. Clinical Psychology was part of a subject review of psychology in March 1999. The subject was rated "excellent", scoring 23 out of a possible 24 points. 12 Admission criteria 12.1 Unlike other doctoral programmes in clinical psychology, admission to the postgraduate phase of the integrated programme is restricted to graduates of the Psychology Departments of the Universities of Hull and York. 12.2 The recruitment and selection policy is determined by the Selection Committee of the programme, and is monitored by the Board of Management. Both of these bodies include substantial NHS service manager representation. Selection criteria for admission are reviewed annually by the Selection Committee and the Selection Panel members taking part. 12.3 Candidates from Hull University wishing to be considered for the postgraduate training programme in Clinical Psychology are entered for selection after Part I Finals results have been published (June of the Second Year). Candidates from York University are entered for selection in June of the Third Year. 15 12.4 A person specification is employed in the selection process and sets out the personal and other attributes required of successful candidates. This includes some experience during undergraduate years, or before, of working within health and personal care services. 12.5 Selected candidates must obtain an upper second or first class degree in single honours psychology and must have studied a number of compulsory clinical modules during the final year of their first degree. 13. Date specification written February 2010 16