Patients frequently present to an otolaryngologist with nasal
advertisement
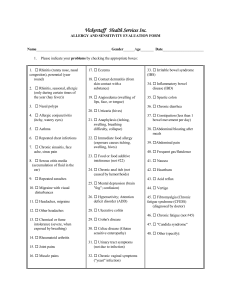
Appendix of Trio Thesis: The Role of Allergy and Smoking in Chronic Rhinosinusitis and Polyposis Steven M. Houser, MD, FACS*, Kevin J. Keen, PhD, PStat** *MetroHealth Medical Center, Cleveland OH, USA, and **University of Northern British Columbia, Prince George, BC, Canada Corresponding author: Steven M. Houser, MD, FACS MetroHealth Medical Center, 2500 MetroHealth Dr., Cleveland OH 44109 O: 216-778-8890, f: 216-778-7868, e: shouser@metrohealth.org 1 Appendix I: Supplementary Literature Review Pathophysiology of Allergic Rhinitis The mechanism of allergic disease is through a Gell and Coombs type I, or IgE mediated, reaction. The subject must first be exposed to a potential allergen, the antigen is taken up by the body, and the host generates IgE antibodies towards the antigen via a Th2 cell line; this phase is referred to as sensitization. Upon re-exposure to the particular antigen, the specific IgE antibodies situated on the surface of mast cells can elicit an immediate response toward the offending allergen; preformed mediators (histamine, leukotrienes, etc.) can be released into the milieu of the allergic response. Late inflammation can then take place as the preformed mediators induce a recruitment of inflammatory cells (eosinophils, etc.) to the active site and more mediators are formed and released (leukotrienes, etc.). Priming can also take place, whereby increasingly smaller amounts of antigen exposure can lead to allergic manifestations.(1) Defining Rhinosinusitis Rhinosinusitis is not as clearly defined as allergic rhinitis. The Task Force on Rhinosinusitis of the American Academy of Otolaryngology-Head and Neck Surgery has attempted to clarify this issue in 1997 and 2003.(6,7) They replaced the term sinusitis with rhinosinusitis to better reflect the inflammation of the sinuses that occurs in conjunction with inflammation of the nose. The 1997 report created five categories of rhinosinusitis based upon the duration of a patient’s symptoms: Acute rhinosinusitis (symptoms present for less than 4 weeks) 2 Subacute rhinosinusitis (symptoms present for more than 4 weeks, but less than 12 weeks) Chronic rhinosinusitis (symptoms present for greater than 12 weeks) Recurrent acute rhinosinusitis (more than 4 acute episodes over 1 year) Acute exacerbation of chronic rhinosinusitis (acute infection, with new acute symptoms, superimposed over a chronic infection, with a constant baseline level of symptoms) In 2003 the task force further refined the definition of rhinosinusitis. A diagnosis of CRS may be suggested by patients’ symptoms and the duration of the illness (greater than 12 weeks of symptoms), but it should be confirmed by physical evidence of mucosal swelling or discharge. The 2003 clinical criteria for diagnosing chronic rhinosinusitis include: Duration of disease is qualified by continuous symptoms or findings for more than 12 consecutive weeks. The physician should be able to identify at least one physical sign of inflammation (e.g. discolored nasal drainage, edema or erythema of the middle meatus or ethmoid bulla, generalized or localized erythema, edema, or granulation tissue, computed tomography scan or plain sinus radiograph suggesting inflammation). 3 Steinke and Borish (2004) presented an alternative scheme for categorizing chronic sinusitis.(A1) They divided chronic (i.e., greater than 6 weeks) sinusitis into 4 groups based upon the underlying disease process: Chronic infectious sinusitis includes infection with some immunologic, or other issue prohibiting clearance of the infection (e.g. immune deficiencies, ciliary dyskinesia). Chronic inflammatory sinusitis is seen in patients whose sinus ostia are repetitively insulted by some disease process (e.g. viral infections, allergic rhinitis, and/or anatomic restrictions). The inflammatory cells seen in this situation are those which are commonly seen in infection (e.g., mononuclear cells). Nasal polyps may develop as a result of the inflammation. Chronic hyperplastic eosinophilic sinusitis (CHES) is characterized by eosinophilic inflammation and often nasal polyposis. Allergic fungal sinusitis may represent a severe form of CHES with fungal colonization and an IgE inflammatory reaction. In 2004 a joint committee of the American Academy of Allergy, Asthma and Immunology, the American Academy of Otolaryngic Allergy, the American Academy of Otolaryngology-Head and Neck Surgery, the American College of Allergy, Asthma and Immunology, and the American Rhinologic Society met to discuss and find common ground for defining sinusitis.(5) Consensus definitions were produced for 4 classes of rhinosinusitis: 4 Acute (presumed bacterial) rhinosinusitis is an inflammatory condition of the nasal and sinus lining lasting up to 4 weeks. Chronic rhinosinusitis without polyposis is an inflammatory condition of the nasal and sinus lining lasting 12 or more weeks. Examination reveals signs of inflammation, but not polyposis. Chronic rhinosinusitis with polyposis denotes bilateral nasal polyposis seen on examination. Classic allergic fungal rhinosinusitis is defined as meeting the criteria of CRS with or without polyposis, as well as allergic mucin and evidence of allergic hypersensitivity to fungal antigens. Thoughts as to the origins of CRS, and how AR fits into the picture Sinusitis cycle The development of rhinosinusitis is often thought of as a wheel, or cycle of events, that conspire to cause the disease initiation and promotion (Figure A 1, modified from Reilly).(A2) Some insult (e.g., viral, bacterial, fungal, allergic, genetic) to the nasal and sinus mucosa results in inflammation. Prolonged inflammation of the nasal mucosa in the region of the ostiomeatal complex can cause obstruction of the paranasal sinus outflow tracts. When the sinus ostia are obstructed there is decreased oxygen tension in the sinus. The stagnant secretions in the sinus become more viscous and acidic, further damaging the respiratory epithelium. This is an ideal environment for bacteria to proliferate and perpetuate tissue insult, causing a cycle of chronic inflammation. The process may then 5 expand to involve adjacent sinuses. The initiating insult, or a propagating one, may be allergic inflammation. 6 Figure A1. Rhinosinusitis Cycle. Particulates/smoke Mucus stasis Allergic Viral Viscous, acidic mucus Inflammation at ostia Fungal Bacterial Bacterial proliferation (possibly fungal proliferation) Rhinosinusitis cycle denoting the initiation and promotion of the disease. 7 Inflammatory cascade The pathophysiology of allergic rhinitis may explain how this relationship develops between PAR and chronic rhinosinusitis. In patients with allergic rhinitis, specific allergens induce a Gell and Coombs type I immunologic reaction in the nasal cavities. Allergens are bound by IgE affixed to the mast cell membrane, which leads to degranulation and release of inflammatory mediators. These mediators cause increased vascular permeability and hypersecretion from serous and mucus glands. Cytokines, formed from lymphocytes and mast cells, attract eosinophils, macrophages, lymphocytes and mast cells, which cause the late-phase allergic response. Allergen hypersensitivity has also been shown to directly cause inflammation in the paranasal sinuses. Slavin studied patients with ragweed sensitivity. During the ragweed season, these patients had increased hyperemia in the sinuses as well as increased metabolic activity in the bone around the sinuses using single photon emission computerized tomography.(A3) T-helper cells type 2 (Th2) lymphocytes play a commanding role in allergic inflammation and they are also important in the development of nasal polyps and most CRS. This commonality speaks to the relationship between AR and CRS.(A4) 8 Immunity Proper host immunity is necessary for sinus health. Low levels of immunoglobulin or selective IgG subclass deficiency are known causes or contributors to the development of CRS.(A5,A6) Atopic patients may also be slightly more susceptible to immune deficiencies.(A7,A8,A9) MCC Impaired mucociliary clearance (MCC) in allergic rhinitis also seems to be very important in the development of chronic sinusitis. MCC is a vital defense mechanism against infection; it serves to trap foreign particles, including bacteria, and eliminate them from the body. In patients with allergic rhinitis, saccharin clearance times are significantly prolonged.(A10,A11,A12) The mechanism is not clearly defined. The slow flow may be attributed to a change in the rheologic properties of mucus.(A13) Damage to nasal cilia in patients with allergic and chronic rhinitis may produce a prolongation in MCC.(A14) The delay in clearance adds to mucus stagnation and consequent bacterial overgrowth. Disease states which directly impair MCC will predispose a patient to CRS. Two examples of such diseases are cystic fibrosis, with overly thickened secretions, and primary ciliary dyskinesia, with deranged ciliary function. 9 Particulate matter The role of the nasal mucus is to trap and expel foreign material, but the system can be overtaxed and come to a standstill in the face of an overwhelming insult. Tobacco use deserves special consideration. Acute, recurrent acute, and chronic rhinosinusitis are more prevalent among subjects who smoke, or expose themselves directly to tobacco.(A15,A16) Tobacco use has been associated with poorer outcomes after sinus surgery among adults with direct exposure and children with indirect or passive exposure.(A17,A18,A19) Indirect tobacco exposure is a notable respiratory irritant. Those that complain of rhinitis associated with indirect tobacco exposure have been shown to have a reduction in MCC.(A20) Tobacco may exert its derogatory effects through reducing MCC by changing cilia or nasal secretions.(A15) Saccharin clearance times are significantly increased in smokers.(A11) A significant decrease in ciliary beat frequency is noted to be tied to cotinine levels which rise with tobacco exposure. (A21) Other models to help explain chronic rhinosinusitis that do not involve allergy Bone involvement Kennedy has suggested possible pathophysiologic changes in the bone morphology in CRS may explain the persistence of the infection. Ethmoidal bone from patients with CRS expressed marked activity not seen in controls. These patients expressed increased fibrosis, remodeling, and woven bone formation; the changes approximate osteomyelitis. Also, inflammation within the bone may be present even when overlying mucosa is normal.(A22) Although, the evidence is not conclusive of an osteomylelitic process, it may contribute to the increased susceptibility for the chronicity of the sinusitis in these 10 patients. Intravenous antibiotics may have improved efficacy in these patients because of increased concentration and duration of antibiotics present in the blood stream. Biofilms In otitis media, a disease analogous to CRS, research has shown the presence of pathogens attached to inner ear mucosa of animal models as a bacterial biofilm, rather than as free-floating organisms.(A23) Correlation of biofilm studies in otitis media led to further investigation in CRS. A hallmark of biofilms is the chronic nature of the disease. Biofilms have a unique mechanism of resistance to conventional bacterial therapy. They survive within a polysaccharide matrix in a metabolically slowed state. In vivo, antibiotics may suppress symptoms of infection by killing free-floating bacteria shed from the bacterial biofilm, but fail to eradicate those bacterial cells still embedded in the biofilm. When the course of antibacterial therapy ends, the biofilm can act as a nidus for a renewed infection as bacteria again spread out of the biofilm. Intravenous antibiotics may be necessary to penetrate the sessile biofilm. Biofilms may also explain the relative inability to culture out bacteria from CRS patients; the low density of organisms recovered in cultures contributes to the notion that microbial agents are not significant in CRS. Biofilms have been detected in the mucosal specimens of patients undergoing surgery for CRS. Biofilms may develop as rapidly as five days after the initiation of bacterial 11 sinusitis.(A24) Biofilms have been detected in the mucosal specimens of patients undergoing surgery for CRS.(A24,A25) Fungal hypothesis Ponikau believes fungi within the nose and sinuses may engender an abnormal immune response resulting in CRS. Eosinophils are recruited to fight of fungi in the nose and sinuses of some patients, while healthy controls do not respond to fungi within their nose. The eosinophils migrate through the nasal mucosa and into the mucus. Eosinophils degranulate to kill off the fungi that selected individuals perceive as a threat. The nasal mucosa itself is accidentally damaged by the release of toxic products. Mucosal destruction allows the bacteria which normally reside harmlessly within the nose to secondarily invade the patient's mucosa and cause an acute exacerbation of chronic sinusitis. Applying these concepts into a treatment scheme with amphotericin B nasal lavage produced modest benefit.(A26) Other researchers have found little benefit with the use of topical amphotericin B.(A27) Superantigen hypothesis One of the possible early events in the development of inflammation in chronic hyperplastic sinusitis with nasal polyposis is the production of exotoxins from Staphylococcus aureus. The exotoxins may act as superantigens and cause activation and clonal expansion of lymphocytes, resulting in massive cytokine production.(A28) The vigorous inflammatory reaction may be responsible for polyp development. 12 Independent treatment of AR and CRS It is important to understand that both AR and CRS are treated as distinct diseases entities. The otolaryngologist combines their treatment protocols to treat both conditions simultaneously, as they so often co-exist. AR treatment Allergic rhinitis is classically treated through a three tiered approach: 1. avoidance/environmental control 2. pharmacotherapy 3. immunotherapy Seasonal allergens can often be deduced by the timing of symptoms; this allows the treating physician to discuss what actions, and when, the patient needs to employ to minimize their pollen exposure. Minimizing outdoor activities during the height of a pollen season may be wise. Following the pollen counts published in print, television, and the internet is often useful to guide activities. Advising removing clothes, showering, and lavaging the nose with saline after prolonged outdoor exposure during an active season is often helpful. Keeping windows closed and using air conditioning can minimize pollen entry into buildings. Avoidance measures for perennial allergens are also possible. The dust mite burden can be reduced by minimizing dust mite reservoirs (e.g., carpeting, wrapping the mattress) and maintaining an environment less conducive to mite growth (e.g., cool, dry air). Cat and dog dander, and cockroach antigen, will fade with removal of the agent. Short of 13 removal, keeping the bedroom free from pets is useful. Allergy testing is often helpful for counseling a patient as to what they need to avoid. If they appear to have perennial allergies it may be very helpful to differentiate a sensitivity to dog from a sensitivity to dust. Pharmacotherapy is a “shotgun” treatment method for allergy – no matter what the patient is allergic to, these medications should provide some benefit. Hence, allergy testing is not an essential feature for prescribing medications for allergic rhinitis. Steroids reduce inflammation by decreasing inflammatory cell infiltration, especially that of mast cells and eosinophils. They also diminish the hyperreactivity and vascular permeability of the nasal mucosa and may reduce the release of mediators from mast cells.(A29) Steroids may be given orally, parenterally, topically, intramuscularly, and intra-turbinal. For the nose, topical intranasal steroids are often preferred because they enhance the therapeutic value while minimizing systemic effects. Intranasal steroid sprays are effective in alleviating nasal congestion, rhinorrhea, and itching. The various sprays on the market seem to vary more in issues such as smell, presence of alcohol, and delivery method rather than efficacy. H1 antihistamines have been one of the basic treatment options for allergic rhinitis. Their primary activity is dose-related competitive binding of the H1 receptors on target cells. They are divided into the classic or first-generation and the second-generation antihistamines. They primarily treat the itching, sneezing, and rhinorrhea symptoms of allergic rhinitis. First generation antihistamines are available OTC; they are often 14 slighted for their sedative side effect. The second generation antihistamine loratadine is also available OTC and it is non-sedating. Other second generation antihistamines are less or non-sedating, but may be more expensive that their older counterparts. Leukotriene inhibitors have demonstrated efficacy in treating allergy symptoms after originally finding a niche treating asthma. These medications also may have efficacy against rhinosinusitis, supporting the assertion that allergic rhinitis and rhinosinusitis have similar processes. Decongestants are available for both topical and oral treatment. The former can cause rhinitis medicamentosa, or rebound rhinitis, if used for a prolonged period. Oral decongestants can also cause problems by elevating blood pressure, disturbing sleep, urinary difficulty, etc. Other medications exist in the allergy armamentarium. Mast cell stabilizers prevent the dissolution of the mast cell wall and prevent degranulation. The mechanism is one of inhibition of calcium-dependent degranulation with accumulation of cyclic AMP. With this action, these agents reduce nasal itching, sneezing, rhinorrhea, and nasal obstruction in allergic rhinitis. Mast cell stabilizers are used topically with minimal side effects; however, the duration of the effect is quite short and thus they must be given several times a day. (A30) 15 Anticholinergics will decrease nasal rhinorrhea. Anticholinergics decrease the amount of nasal secretions, but they have no effect on nasal obstruction. Anticholinergics, such as ipratropium bromide and oxitropium bromide, inhibit muscarinic cholinergic receptors. They have no known current role in the treatment of vascular congestion/decongestion of the nose.(A31) Anti-IgE therapy has proven efficacy in treating both seasonal and perennial allergic rhinitis.(A32) Immunotherapy is considered by many allergists to be the most powerful tool to treat allergy. Immunotherapy or “desensitization” is not a necessity for all allergic patients. It is usually considered if there is insufficient control with the use of pharmacotherapy and avoidance for patients with moderate to severe symptoms. The exact mechanism(s) of immunotherapy is unknown, but includes the development of IgG blocking antibody, and the alteration of T-cell interactions.(A33) Patients are given extracts containing the allergens that they are sensitive to; over time they lose their sensitivity to these exact items. Immunotherapy can be given orally or sublingually, although it is most often delivered by subcutaneous injection in the United States. The benefits of immunotherapy can last long after discontinuing therapy. CRS treatment Treatment for CRS revolves around identifying and treating any underlying causes and attempting to break the inflammatory cycle as depicted earlier. Infectious contribution 16 must be considered. Conservative measures to treat CRS include nasal saline lavage, decongestants, and mucolytic agents. Multiple prescription agents to combat CRS are available as well. Broad-spectrum antibiotics are useful in CRS and if they do not cure the disease state, they tend to provide at least a temporary reprieve from symptoms. Antibiotics should be used for 3 or more weeks. Culture-directed therapy may be more effective than empiric treatment. Antibiotics can be delivered orally, intravenously, or topically; the later is controversial as to whether the agent actually reaches the target tissue. Steroids are potent agents to diminish inflammation, regardless of the type of inflammation. Steroids can reduce polyp tissue as well as shrinking inflamed tissue back to a normal appearance. Topical, injection, and oral steroids all serve roles in managing chronic rhinosinusitis. The relative banality of topical steroids leads a physician to prescribe these medications to most patients with chronic rhinosinusitis. Oral steroids, and even local steroid injection, are used by physicians to shrink polyp tissue. Leukotriene inhibitors also work to modify the inflammatory response, and may play a role in treating chronic rhinosinusitis. Macrolide antibiotics appear to also have antiinflammatory effects and, while not convincingly inhibiting the typical pathogens involved in CRS, they may be a useful adjunctive therapy when used for longer than 4 weeks.(A34) Macrolides may also inhibit biofilm formation.(A24) Aspirin 17 desensitization can help to limit the recurrence of polyposis in Samters triad patients.(A35) Conjoint Treatment of Allergic Rhinitis and Chronic Rhinosinusitis Considering allergic rhinitis in all rhinosinusitis patients, and treating allergies accordingly, is an important way to combat rhinosinusitis. Atopic disease is considered a strong cofactor in rhinosinusitis, so its contribution to the disease process cannot be overstated; treatment of atopic disease may help to resolve rhinosinusitis symptoms. Several studies have suggested allergic patients with rhinosinusitis may benefit from immunotherapy.(20,21) Improvement in MCC from immunotherapy may be a factor in this therapy’s effectiveness.(A36) 18 Appendix II: Supplementary Results Table AI. Allergy prevalences among CRS cases tested by RAST or IDT. Allergy Percentage Prevalence (SE) 59.9 (3.2) Any 40.5 (3.2) Seasonal 27.2 (2.9) Trees Cottonwood 12.9 (2.2) White Birch 12.9 (2.2) White Ash 11.6 (2.1) American Elm 11.2 (2.1) Sycamore 10.8 (2.0) White Mulberry 8.6 (1.8) 30.6 (3.0) Grasses Brome or Bermuda 27.2 (2.9) Redtop 11.2 (2.1) 31.9 (3.1) Weeds Lamb’s Quarters 17.2 (2.5) English Plantain 16.4 (2.4) Sheep’s Sorrell 11.2 (2.1) 56.9 (3.3) Perennial 38.4 (3.2) Dust mites Dermatophagoides farinae 35.8 (3.1) Dermatophagoides pteronnysius 33.6 (3.1) 39.2 (3.2) Epidermals Cat 29.7 (3.0) Dog 22.0 (2.7) Cockroach 22.0 (2.7) 29.3 (3.0) Molds Candida 19.8 (2.6) Alternaria 15.5 (2.4) Aspergillus fumigatus 11.6 (2.1) Helminthosporium 10.3 (2.0) Hormodendrum 9.5 (1.9) Phoma 9.5 (1.9) Pullularia 8.2 (1.8) Penicillium 7.3 (1.7) Curvularia 6.0 (1.6) Trichoderma 3.9 (1.3) Trichophyton 2.6 (1.0) Rhizopus 2.2 (1.0) Epidermophyton 1.7 (0.9) Fusarium 1.7 (0.9) 19 Appendices References A1 Steinke JW, Borish L. The role of allergy in chronic rhinosinusitis. Immunol Allergy Clin N Am 2004; 24: 45-57. A2 Reilly JS. The sinusitis cycle. Otolaryngol Head Neck Surg 1990; 103 (5): 856-862. A3 Slavin RG, Zilliox AD, Samuels LD. Is There Such An Entity As Allergic Sinusitis? Journal of Allergy and Clinical Immunology 1988; 81: 284. A4 Dykewicz MS. Rhinitis and sinusitis. J Allergy Clin Immunol 2003; 111: S520-9. A5 May A, Zielan S, von Ilberg C, Weber A. Immunoglobulin deficiency and determination of pneumococcal antibody titers in patients with therapy-refractory recurrent rhinosinusitis. Eur Arch Otorhinolaryngol 1999; 256: 445-59. A6 Scadding GK, Lund VJ, Darby YC, et al. IgG subclass levels in chronic rhinosinusitis. Rhinology 1994; 32: 15-9. A7 Cortesina G, Carlevato MT, Bussi M, Baldi C, Majore L, Ruffino C. Mucosal immunity in allergic rhinitis. Acta Otolaryngol. 1993 May;113(3):397-9. A8 Sustiel A, Rocklin R. T cell responses in allergic rhinitis, asthma and atopic dermatitis. Clin Exp Allergy. 1989 Jan;19(1):11-8. 20 A9 Stevens WJ, de Backer W, Vermeire PA. Serum IgA, IgG, IgM and IgD in allergic (type I) and non-allergic respiratory diseases. Clin Allergy. 1983 Jan;13(1):11-9. A10 Corbo GM et al. Measurement of nasal mucociliary clearance. Arch Dis Childhood 1989; 64: 546-550. A11 Mahakit P, Pumhirun P. A Preliminary Study of Nasal Mucociliary Clearance in Smokers, Sinusitis and Allergic Rhinitis Patients. Asian Pacific Journal of Allergy and Immunology 1995; 13: 119-121. A12 Stanley PJ et al. Abnormal Nasal Mucociliary Clearance in Patients with Rhinitis and its Relationship to Concomitant Chest Disease. British Journal of Disease of the Chest 1985; 79: 77-82. A13 Passali D, Bellusi L, Lauriello M. The rheological characteristics of nasal mucus in patients with rhinitis. Eur Arch Otorhinolaryngol 1995; 252: 348-352. A14 Maurizi M et al. Ciliary ultrastructure and nasal mucociliary clearance in chronic allergic rhinitis. Rhinology 1984; 22: 233-240. A15 Lieu JE, Feinstein AR. Confirmations and surprises in the association of tobacco use with sinusitis. Arch Otolaryngol Head Neck Surg 2000; 126: 940-6. 21 A16 Chen Y, Dales R, Lin M. The epidemiology of chronic rhinosinusitis in Canadians. Laryngoscope 2003; 113: 1199-205. A17 Briggs RD, Wright ST, Cordes S, Calhoun K. Smoking in chronic rhinosinusitis: a predictor of poor long-term outcome after endoscopic sinus surgery. Laryngoscope 2004; 114: 126-8. A18 Ramadan HH, Hinerman RA. Smoke exposure and outcome of endoscopic sinus surgery in children. Otolaryngol Head Neck Surg 2002; 127: 546-8. A19 Kim HY, Dhong HJ, Chung SK, et al. Prognostic factors of pediatric endoscopic sinus surgery. Internat J Ped Oto 2005; 69: 1535-9. A20 Bascom R, Kesavanathan J, Fitzgerald TK, et al. Sidestream tobacco smoke exposure acutely alters human nasal mucociliary clearance. Environ Health Perspect. 1995 Nov;103(11):1026-30. A21 Agius AM, Wake M, Pahor AL, Samllman A. The effects of in vitro cotitine on nasal ciliary beat frequency. Clin Otolaryngol Allied Sci. 1995 Oct;20(5):465-9. A22 Kennedy DW. Pathogenesis of chronic rhinosinusitis. Ann Otol Rhinol Laryngol Suppl. 2004;193:6-9. 22 A23 Post JC, Stoodley P, Hall-Stoodley L, Ehrlich GD. The role of biofilms in otolaryngologic infections. Curr Opin Otolaryngol Head Neck Surg. 2004 Jun;12(3):18590. A24 Palmer J. Bacterial biofilms in chronic rhinosinusitis. Ann Otol Rhinol Laryngol 2006; 115(9)Suppl 196: 35-9. A25 Ramadan HH, Sanclement JA, Thomas JG. Chronic rhinosinusitis and biofilms. Otolaryngol Head Neck Surg 2005; 132: 414-7. A26 Ponikau JU, Sherris DA, Weaver A, Kita H. Treatment of chronic rhinosinusitis with intranasal amphotericin B: a randomized, placebo-controlled, double-blind pilot trial. J Allergy Clin Immunol 2005;115(1):125-31. A27 Ebbens FA, Scadding GK, Badia L, et al. Amphotericin B nasal lavages: not a solution for patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2006 Nov;118(5):114956. A28 Bernstein JM, Kansal R. Superantigen hypothesis for the early development of chronic hyperplastic sinusitis with massive nasal polyposis. Curr Opin Otolaryngol Head Neck Surg. 2005 Feb;13(1):39-44. 23 A29 Lund VJ, Aaronson D, Bousquet J, Dahl R, Davies RJ, Durham SR, et al. International Consensus Report on the Diagnosis and Management of Rhinitis. Allergy 1994; 49: Supplement. A30 King HC. Mast Cell Stabilizers. Otolaryngol Head Neck Surg 1992; 107:841-4. A31 Bronsky EA, Druce H, Findlay SR, et al. A clinical trial of ipratropium bromide nasal spray in patients with perennial nonallergic rhinitis. J Allergy Clin Immunol 1995; 95: 1117. A32 Holgate ST, Djukanovic R, Casale T, Bousquet J. Anti-immunoglobulin E treatment with omalizumab in allergic diseases: an update on anti-inflammatory activity and clinical efficacy. Clin Exp Allergy. 2005 Apr;35(4):408-16. A33 Fornadley J. Allergy immunotherapy. Otolaryngol Clin North Am 1998; 31(1): 11127. A34 Vining EM. Evolution of medical management of chronic rhinosinusitis. Ann Otol Rhinol Laryngol 2006; 115(9)Suppl 196: 54-60. A35 Pfaar O, Klimek L. Eicosanoids, aspirin-intolerance and the upper airways - current standards and recent improvements of the desensitization therapy. J Physiol Pharmacol. 2006 Dec;57 Suppl 12:5-13. 24 A36 Cmejrek RC, Gutman MT, Torres AJ, Keen KJ, Houser SM. The Effect of Injection Immunotherapy on Mucociliary Clearance in Allergic Patients. Otolaryngol Head Neck Surg 2005; 133(1):9-15. 25
![Form: Medical history: for new patients [Form]](http://s3.studylib.net/store/data/007605872_2-8e9e11d5356e956dfeae2f990eec56a6-300x300.png)