DRAFT
advertisement

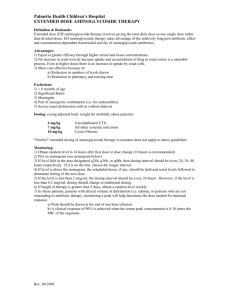
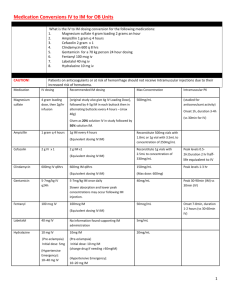
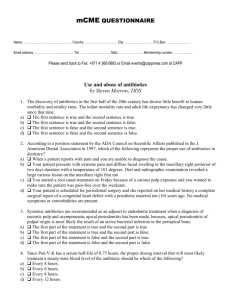
#16 PROJECT NAME: Controlling antibiotics dosing errors in patients with impaired renal function using an EMR alert Institution: UTMB Galveston Primary Author: Hudali, Tamer MD Secondary Author: Low, Leah MD., Almomani, Ahmed MD., Masel, Meredith PHD. MSSW. Project Category: General Quality Improvement Overview: Frequently medication dosing is not adjusted according to the glomerular filtration rate (GFR) resulting in many avoidable adverse outcomes such as worsening renal function, medication toxicity, and death. This problem originates from either decreased awareness of the patient’s estimated GFR and/or a lack of knowledge regarding the prescribed medication. This quality improvement project was intended to decrease the rate of dosing errors in patients with impaired renal function and to increase both patient and physician awareness of kidney function. The idea was to start with a group of medications (antibiotics) that commonly requires renal dosing adjustment and then broaden the intervention to include different kinds of medications and interventions (IV contrast introduction and chemotherapy for instance). A team of physicians, nurses, pharmacists and IT staff were grouped to review the process of antibiotic administration. The project began in August 2012 with a data collection from EPIC (the electronic medical record system used at UTMB) to assess the rates of dosing errors based on the patient’s GFR at the time of ordering. Data from a three month period was assessed, followed by a repeat assessment after the intervention. The data were collected from medical floors that were covered by internal medicine and family medicine services at John Sealy hospital, UTMB. Purpose/Aim: Our aim is to reduce antibiotics dosing errors in renally impaired patients by 20% in a 3 month period (by March 2013) through implementing a best practice alert in our EMR. Tools and Measurement: The following quality tools have been used: Fish bone Diagram: Process flow chart: Intervention and Improvement: After discussing the possible areas of intervention and reviewing the fishbone diagram and process flow chart, we chose the EMR as the tool for intervention. Six antibiotics were chosen based on the frequency of use in our institution. These antibiotics are: Vancomycin, Piperacillin-Tazobactam, Levofloxacin, Cefepime, Ertapanem and Meropenem. With the help of our IT department, 2321 antibiotic orders were collected and reviewed to assess for the rates of wrong dosing based on the GFR at the time of dosing. The GFR was calculated manually for each patient using the MDRD formula. Patients with acute kidney injury were excluded from this data analysis. The clinical indications for antibiotics were considered when assessing the appropriate dose and the dose that needs adjustment. Ideally, we would like our EMR to recognize a patient with impaired renal function, recognize the antibiotic being ordered needs adjustment, and recommend the appropriate dosing using dosing guidelines per www.uptodate.com. However, we encountered technical difficulties and were unable to implement this system. Instead, the alert we formulated is a best practice alert that provides the ordering staff with the current GFR based on the current creatinine. The EMR will prompt the provider with a link to the uptodate website to help determine the appropriate dose: The alert was launched on January 1st 2013. A presentation was given to the internal medicine residents during morning report explaining the implications and the purpose of the alert. One thousand one hundred and sixteen antibiotics orders were reviewed (with the same criteria described above) in a 2 month period after the release of the EMR alert. Intervention Results: We compared dosing error rates between the two sets of data collected before and after the intervention. Patients on dialysis were studied separately. As shown above, the total error percentage decreased significantly after the alert system was launched. The percentage of errors before the intervention was 15.4%, and the percentage of errors after the intervention was 3.7%. To assess the significance of these results, a one sided Z-score was performed. Z score: 9.5002 with a P value of < 0.000001. Table 1: Pre-intervention Data Correct dose Wrong dose Total Antibiotics orders 1856 338 2194 percentage 84.6% 15.4% 100% Antibiotics orders 959 37 996 percentage 96.3% 3.7% 100% Table 2: Post-intervention Data Correct dose Wrong dose Total The same analysis was conducted on data obtained from dialysis patients, however no significant difference was found between the 2 groups. The following graphs illustrate the reduction in errors rates shown in all antibiotic groups: A cost-effectiveness analysis is currently being conducted and results are pending. We anticipate a significant cost reduction associated with the reduction in incorrect dosing. Revenue Enhancement /Cost Avoidance / Generalizability: After reviewing the results and following the PDSA cycle, multiple areas of improvement in our intervention were identified. In the future, we would like to include patients with AKI by adding a best practice alert that identifies a change in creatinine of more than 50% or more than 0.3 mg/dl (as per current guidlines). This alert will signal an ordering provider that the patient’s renal function has changed and antibiotics need adjustment. We also feel it is imperative to include patients on dialysis and plan to add an addendum to our current alert notifying the provider when a patient has end stage renal disease. Our intervention has decreased the cost of health care by two aspects. First, we have avoided unnecessary doses of antibiotics to patients with renal impairment without affecting treatment rate or outcome. Second, we have decreased the rate of possible adverse outcomes and potential harm that may occur when overdosing antibiotics and failing to complying with the current guidelines regarding renal dosing of antibiotics. Because we achieved highly significant results with a fairly simple intervention, in the future we would like to generalize the alert to include all medications that require renal adjustment. Additionally, we would like the alert to include procedures requiring contrast that may harm patients with renal impairment such as imaging and cardiac catheterizations.