sloan neuro exam aaem 2005 - Foundation for Education and
advertisement

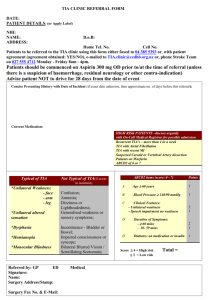
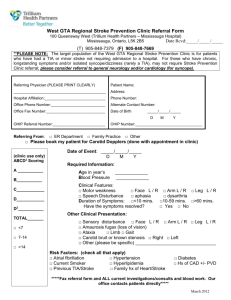
2008 Clinical Decisions in Emergency Medicine “Transient Ischemic Attack Patient Update: The Optimal Management of Emergency Department Patients With Suspected Cerebral Ischemia” Cerebral Ischemia and Transient Ischemic Attacks: Definitions and a Historical Perspective J Stephen Huff, MD, FACEP Associate Professor of Emergency Medicine & Neurology University of Virginia Charlottesville, VA Learning Objective and Key Clinical Questions Assess the clinical significance of how the definition of cerebral ischemia and transient ischemic attacks has evolved over time. How are TIA, RIND, cerebral ischemia, and cerebral stroke defined? What are the epidemiology and outcomes of patients with cerebral ischemia? How have these definitions changed over time and for what reasons, including the progress of advanced neuroimaging? Has the outcomes of these cerebral ischemia patients changed over time as the definitions have changed? Optimizing ED TIA Patient Management: TIA Definitions & Historical Perspectives 2008 FERNE / Clinical Decisions in Emergency Medicine J. Stephen Huff MD, FACEP Page 2 of 7 Key Clinical Questions and Learning Points How are TIA, RIND, cerebral ischemia, and cerebral stroke defined? Definitions are changing for TIA and stroke. TIA, or transient ischemic attack, has traditionally been defined as a stroke syndrome that is time-limited with complete resolution. Even though it has long been recognized that most TIAs resolve over minutes, and that the longer ischemic symptoms persist, the more likely a stroke is present, research criteria and consensus opinion arbitrarily defined a TIA as having resolution of signs and symptoms within 24 hours of onset. Implicit in the definition is that there must be some pre-test probability assessment of a transient symptom or sign having ischemic pathophysiology. Symptoms lasting seconds are unlikely to be ischemic in etiology. Simple dizziness or vertigo, without associated signs and symptoms, is unlikely to be ischemic in origin. Transient loss of consciousness (syncope) or seizures are not TIA syndromes. The symptoms of ischemia are usually negative in nature, that is neurologic deficits, rather than positive symptoms such as shaking. “Marching” of symptoms up an extremity, such as progression of a deficit or paresthesias, also suggests non-ischemic pathophysiology. RIND, or reversible ischemic neurologic deficit, was defined in the past by consensus as a stroke syndrome with resolution of signs and symptoms within 6 weeks. RIND has fallen from clinical usage. An ischemic stroke is an enduring neurologic syndrome with pathophysiology from embolic or thrombotic causes. What are the epidemiology and outcomes of patients with transient ischemic attack? It is estimated that there are 200,000-500,000 patients with transient ischemic attack in the United States each year. Outcomes data is still being accumulated especially as definitions are revised. It is estimated that somewhere between 2-13% of patients with transient ischemic attack will develop a stroke within one month, and up to one-third within 5 years. In some studies, high early risk of stroke following TIA has been found with up to onehalf of the strokes occurring within 48 hours. Optimizing ED TIA Patient Management: TIA Definitions & Historical Perspectives 2008 FERNE / Clinical Decisions in Emergency Medicine J. Stephen Huff MD, FACEP Page 3 of 7 How have these definitions changed over time and for what reasons, including the progress of advanced neuroimaging? Definition of transient ischemic attack is blurring with that of stroke. With advances in neuroimaging, TIA patients are increasingly identified whom have clinically transient events with resolution of deficits, but with abnormalities found on special neuroimaging. Diffusion-weighted MRI is an increasingly employed technology for patients with stroke and TIA. A new syndrome of TIA with DWI abnormality is being defined. The definition of TIA is being revised to reflect tissue-based pathology instead of a timereferenced definition. This implies that advanced neuroimaging is necessary to distinguish TIA patients with and without neuroimaging (MRI-DWI) abnormalities. Has the outcomes of these cerebral ischemia patients changed over time as the definitions have changed? Clearly the natural history of TIA patients is being further delineated with improved neuroimaging. The hope would be that subsets of patients might be identified where interventions might moderate stroke rate following TIA. Outcomes data is lagging. Antiplatelet agents, notably aspirin, seem to show risk reduction of stroke and other vascular events following TIA of approximately 20%. Other antiplatelet regimens including clopidegrel, ticlopidine, or combination treatments may be slightly better though arguably definitive data is lacking. A few sub-groups have been identified where interventions do limit subsequent stroke risk. Patients with TIA and significant carotid stenosis > 70% do have reduction in stroke risk following endarterectomy. For patients with carotid stenosis < 70%, antiplatelet medical treatment seems to be equal to surgical management. In patients with atrial fibrillation and TIAs, anticoagulation with warfarin has been shown to be superior to antiplatelet therapy in preventing strokes. Optimizing ED TIA Patient Management: TIA Definitions & Historical Perspectives 2008 FERNE / Clinical Decisions in Emergency Medicine J. Stephen Huff MD, FACEP Page 4 of 7 Are there publications that help the emergency physician with the approach to assessment of TIA patients? ___________________________________________________________ TIA, RIND, minor stroke: a continuum, or different subgroups? Koudstall PJ, van Gijn J, Frenken CWGM, Hijdra A, Lodder A, Vermeulen M, Bulens C, Franke CL (for the Dutch TIA Study Group) J Neurol, Nsurg, Psych 1992;55:95-97. One of the first articles to advance the argument that these time-defined clinical entities should be thought of as existing along a continuum rather than as separate groups. Cranial CTs were obtained more than 24 hours after the neurologic event. CT abnormalities showed relevant ischemic lesions in 13% of patients with clinical TIA (<24 hour definition), 35% of patients with RIND, and 49% of patients with minor stroke. CT infarction patterns were present more often with longer symptom duration but were also found in some patients with symptoms lasting less than a minute. ___________________________________________________________ The duration of symptoms in transient ischemic attack Kimura K, Minematsu K, Yasaka M, Wada K, Yamaguchi T Neurology 1999;52:976-980. Clinical records were reviewed of 81 patients with carotid distribution TIA. Patients were investigated with brain imaging (CT or MR) , EKG monitoring, and transthoracic echocardiography, and carotid ultrasound. TIA of longer duration (> 60 minutes) was associated with the presence of emboligenic cardiac disease or arterial disease. Recent infarcts on CT were seen more frequently in patients with longer duration TIA. Optimizing ED TIA Patient Management: TIA Definitions & Historical Perspectives 2008 FERNE / Clinical Decisions in Emergency Medicine J. Stephen Huff MD, FACEP Page 5 of 7 ___________________________________________________________ Timing of TIAs preceding stroke: time window for prevention is very short Rothwell PM, Warlow CP Neurology 2005;64:817-820 Retrospective review of patients with acute ischemic stroke from two studies who reported preceding TIA symptoms. 23% of patients gave a history of TIA before their stroke with 17% of those TIAs occurring the day of infarction, 9% on the previous day, and 43% at some point during the prior 7 days. ___________________________________________________________ Head computed tomography findings predict short-term stroke risk after transient ischemic attack Douglas VC, Johnston CM, Elkins J, Sidney S, Gress D, Johnston SC Stroke 2003;34:2894-2899 67% of patients presenting to EDs that received a diagnosis of TIA had CT scans performed within 48 hours. Evidence of new infarct was found in 4%. A nonischemic cause of TIA was found in 1.2% (tumors, chronic subdural hematoma). Risk of stroke during 90 day followup was higher in TIA patients that had a new infarct on CT. Patients with TIA and resolved symptoms with evidence of acute infarction on head CT may make up a population especially vulnerable to stroke. Optimizing ED TIA Patient Management: TIA Definitions & Historical Perspectives 2008 FERNE / Clinical Decisions in Emergency Medicine J. Stephen Huff MD, FACEP Page 6 of 7 ___________________________________________________________ DWI abnormalities and clinical characteristics in TIA patients Inatomi Y, Kimura K, Yonehara T, Fujioka S, Uchino M Neurology 2004;62:376-380 129 consecutive patients with TIA had MRI with DWI performed within 14 days. DWI demonstrated recent ischemic lesions in 44%. Prolonged TIA duration (> 30 minutes) and symptoms or signs of disturbances of higher brain function (aphasia, hemianopia, unilateral spatial neglect) were significant and independent factors associated with DWI abnormalities. ___________________________________________________________ Transient ischemic attack and stroke can be differentiated by analyzing early diffusion-weighted imaging signal intensity changes Winbeck K, Bruckmaie K, Etgen T, von Einsiedel HG, Rottinger M, Sander D Stroke 2004;34:1095-1099 DWI was performed within 24 hours after symptom onset in 60 patients with TIA and 37 patients with stroke. Patients with stroke had significantly higher DWI signal than that of patients with TIA. The authors suggest that DWI can differentiate stroke from TIA in patients as little as 6 hours from syndrome onset. Optimizing ED TIA Patient Management: TIA Definitions & Historical Perspectives 2008 FERNE / Clinical Decisions in Emergency Medicine J. Stephen Huff MD, FACEP Page 7 of 7 ___________________________________________________________ Transient ischemic attack – proposal for a new definition Albers GW, et al for the TIA Working Group N Engl J Med 2002;347:1715-1716 The redefinition of TIA: the uses and limitations of DWI in acute ischemic cerebrovascular syndromes Warach S, Kidwell CS Neurology 2004;62:359-360 Albers et al state the proposal for tissue-based new definition of TIA,”A TIA is a brief episode of neurologic dysfunction caused by focal brain or retinal ischemia, with clinical symptoms typically lasting less than one hour, and without evidence of acute infarction.” Stroke / infarction is defined by persistent clinical signs or characteristic imaging abnormalities. The arbitrary time criterion of 24 hours is dismissed in this new definition. The second reference above discusses some advantages and limitations of DWI use. ferne_clindec_2008_tia_huff_definitions_keyclinical_062508_final