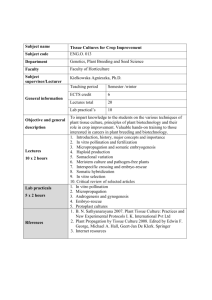
In vitro systems
advertisement
Human-Based In Vitro Systems for Predicting In Vivo Hepatic Clearance of Drugs Name: Ruthmila F. Paskel Student number: 3858413 Course: MSc Thesis, MSc Toxicology and Environmental Health Examiner: Nynke I. Kramer Second Reviewer: Bas J. Blaauboer Date: December 6, 2012 Table of contents Abstract .......................................................................................................... 3 Introduction .................................................................................................... 4 In vitro systems.............................................................................................. 6 Human liver microsomes .............................................................................. 6 Hepatocytes ................................................................................................. 8 Fresh and cryopreserved primary human hepatocytes ............................. 8 Human hepatic cell lines ........................................................................... 9 Precision-cut human liver slices ................................................................. 10 Conclusion ................................................................................................... 12 References ................................................................................................... 14 2 Abstract Unfavorable drug metabolism is the main reason for attrition of new chemical entities and withdrawal of drugs from the market, costing pharmaceutical companies a great deal of money and time. Therefore, obtaining information about the drug metabolism of a new chemical entity via the hepatic clearance in the early stages of the drug development process is crucial in guaranteeing its success. Human-based in vitro systems, especially liver microsomes, hepatocytes and liver slices are increasingly applied in the drug development process for this purpose. The aim is to determine which of these commonly used systems is the most appropriate for predicting hepatic clearance in humans. Although there is no “perfect” in vitro system, primary hepatocytes and the HepaRG cell line are the most representative systems of the liver at present. However, it has to be kept in mind that besides their potential to accurately predict in vivo clearance other influencing factors that may interfere with their ability to do so also have to be taken into consideration when deciding which is the most appropriate system. 3 Introduction The development of a new chemical entity (NCE) is a very expensive and time-consuming process. It can cost pharmaceutical companies between 800 million to 900 million USD and take well over 10 years before the NCE is put on the market, if it ever reaches the market at all 4, 9. It is, therefore, of utmost importance to obtain enough information about the pharmacokinetic properties of the NCE early in the development process. Since unfavorable drug metabolism is one of the main reasons for attrition of a NCE during the drug development process and the withdrawal of a drug from the market, sufficient information about drug metabolism early in the drug development process is crucial in guaranteeing the success of this process 34. Although there are several organs contributing to metabolism, the liver is the major organ in biotransformation of drugs in mammals 52. Biotransformation or hepatic metabolism is an enzymatic process in which a drug is chemically modified to facilitate its elimination via the urine or feces. It can be divided into two phases, namely phase I and phase II. During the former phase drugs become slightly watersoluble by exposing or incorporating functional groups mainly via the oxidation pathway. The key enzymes involved in this pathway include enzymes belonging to the cytochrome P450 superfamily, also known as CYPs. CYPs can be found throughout the body, but is predominantly present in the liver. Moreover, the CYPs superfamily can be divided into several subfamilies of which the CYP1A, CYP2C, CYP2D, and CYP3A are responsible for the metabolism of nearly all drugs 4. At present, CYP3A alone is responsible for an impressive 50% metabolism of all drugs on the market 38. After phase I, phase II largely increases the water-solubility of drugs by conjugating polar groups to the drug. An important aspect of a NCE is its metabolic stability. The metabolic stability gives information about the susceptibility of a NCE to metabolism in the body, often by the liver 9. In other words, the higher the metabolic stability, the slower the chemical compound is metabolized whereas the lower the metabolic stability, the more rapidly it is metabolized. In practice it is difficult to directly measure the stability of a NCE, therefore, this aspect is often measured as the kinetic parameter, clearance 9. Clearance describes the depletion of an unchanged compound from a given volume of plasma or blood per unit of time 29. For example, if clearance is 100mL/minutes, 100mL of plasma or blood is cleared of the compound each minute. Thus, given the relation between metabolic stability and clearance, this is a suitable parameter for obtaining information about the drug metabolism of a NCE. Most importantly, clearance is very useful when considering the therapeutic dose range and regimen of a NCE in the later stages of the drug development process 13. Various organs in the body can contribute to clearance and the sum of all these clearances is referred to as the total body clearance. Furthermore, clearance by the liver is referred to as the hepatic clearance (CLh). Due to the fact that the liver is a major player in biotransformation of drugs, as previously stated, the CLh is often used. Traditionally, laboratory animals have been used in metabolic studies as models for humans. The fact that these models are intact systems containing the complex interactions among different compartments like in humans makes them attractive to use in predicting the clearance of NCEs in humans. However, similarities in physiology among species do not always imply similarities in drug metabolism. 4 For example, the human liver contains high levels of CYP3A in contrast to the liver of laboratory animals, like rats 33. Moreover, large variations in the expression levels and metabolic activity of CYP2D and CYP3A have been reported within the human population 36, 38, 48. If even humans differ in their levels and activity of important metabolic enzymes, animal models cannot accurately reflect the full span of clearance values in humans. Thus, human-derived materials would be much more suitable as candidates for predicting drug clearance in humans. Not surprisingly, in vitro systems with human tissue have been increasingly used in drug development in the past decade. With the increasing application, different classes of in vitro systems have been developed. The aim of this thesis is to determine what the most appropriate human-based in vitro system is for predicting hepatic clearance of drugs in humans. The thesis discusses how in vitro systems can be used to predict CLh in humans. It considers the three most commonly used human-based in vitro systems for this purpose and weighs their advantages and disadvantages. 5 In vitro systems In vitro systems can be defined as subcellular fractions, cells or tissues cultured for experimental purposes under artificial conditions mimicking the physiological milieu in organisms. Some reasons why these systems are increasingly used in early prediction of drug clearance are that they are relatively easy to maintain and their use may be automated in a high throughput setting. Most importantly, in vitro systems can be obtained from different human-derived organs or tissues what makes them so suitable for predicting clearance in humans. The prediction of CLh from in vitro clearance data is a stepwise process 32. First, the in vitro system is incubated with the test substrate and the depletion of this substrate in the in vitro assay medium is chromatographically measured at different time points. From this parameter the rate constant for the depletion of unchanged compound, k, can be calculated. The rate constant k can be then used to calculate the in vitro intrinsic clearance (CLint). CLint is the maximum ability of the liver to clear a drug in the absence of other physiological determinants such as hepatic blood flow and nonspecific binding of drugs to plasma proteins within the blood matrix 9. Nevertheless, non-specific drug binding within the in vitro matrix can also be a crucial determinant for accurately predicting the CLh. This matter will be further discussed in the next subsections. The next step is scaling the calculated in vitro CLint to the whole liver. Although there are several scaling factors (SF), the biological SF is the easiest and most often used. For example, in the case of hepatocytes as the in vitro system, first, the average number of hepatocytes per gram of liver is considered and then the average grams of liver per kilogram of body weight. Now that the in vivo CLint has been calculated the final step is the in vitro-in vivo extrapolation (IVIVE) by liver models. The most used liver model is the well-stirred model, which states that the free fraction of a compound is constant throughout the hepatic compartment and is equal to the free fraction within the plasma or blood matrix 32. In other words, only that fraction of the compound that has not bind to plasma proteins is able to reach the enzymes and be cleared. Thus, by incorporating the aforementioned physiological determinants via the well-stirred model, the CLh in humans can be predicted from in vitro data. The three commonly used human-based in vitro systems for this purpose are liver microsomes, hepatocytes and precision-cut liver slices. Each system will be further discussed in the following subsections. Human liver microsomes Human liver microsomes (HLM) are vesicles of endoplasmic reticulum (ER) prepared by centrifugation of liver homogenates from either fresh or frozen human liver tissue 30 . Coming from the ER, these HLM contain most of the CYP enzymes, which, as stated earlier, are the most important metabolizing enzymes for most drugs. Nevertheless, it has been reported that microsome preparation from frozen liver tissue causes a decrease in the CYP catalytic activity and content 47, 55. Therefore, microsome preparation from fresh human liver tissue is preferred. In contrast to some other in vitro systems, microsomes can be stored for a long period of time at 80C without any significant loss of neither CYP catalytic activity nor its content 62. Moreover, Pearce et al. showed that freezing at -80C followed by thawing at room temperature for up to 10 times did not cause significant loss of the CYP activity in 6 HLM 47. Due to this important aspect, HLM are commercially available thereby circumventing the limited availability that some in vitro systems face. Although high preparation-to-preparation variation in the CYP activity of HLM from different donors has been reported, pooling the HLM provide an easy and successful solution to this problem 51. In this way the pooled microsomal preparation reflects an average man and the predicted CLh may be representative for a given population. In addition to the CYP enzymes, HLM also contain UGTs, which are one of the phase II enzymes involved in conjugation of drugs. Microsomes are not intact systems and, therefore, they do not contain cofactors that are essential for metabolizing enzymes. By either supplementing the CYPs or the UGTs with cofactors, each metabolism pathway can be thoroughly studied separately 34. This makes liver microsomes among the most popular in vitro systems used in pharmacological studies. On the other hand, this system is only a simplistic model for a far more complex situation. During preparation of the HLM the outer plasma membrane is removed and along with it cytosolic phase II enzymes. Not surprisingly, these systems inaccurately predict the in vivo CLint of drugs predominantly metabolized by phase II enzymes 2, 55. Another crucial component that is being removed along with the plasma membrane are transporters. Nowadays, the importance of transport-mediated uptake as a determinant of the plasma clearance of drugs in humans is being more and more acknowledged 28, 54. For slow diffusing drugs, in particular, this can be a rate-limiting step in drug clearance 7. In addition, some drugs can influence their own clearance or that of other co-administered drugs by accelerating the rate at which they are metabolized by CYPs. Many CYP-inducing drugs exert their effects at a transcriptional level and because HLM do not contain cell nuclei, this is not taken into consideration when using these systems for predicting in vivo clearance 55. One other major limitation of this system is its limited incubation time. After only 2 hours of incubation the enzyme activities start decreasing making liver microsomes an inappropriate model for slow metabolizing drugs 9. Most importantly, it has been shown that the incubation matrix can have significant influence on the catalytic activity of CYP3A4 in microsomal preparations 24. In the literature different results regarding the ability of HLM to predict in vivo clearance are reported. One of the main causes of these differences is the nonspecific drug binding to the phospholipid bilayer membrane of HLM 45. Austin et al. showed using rat liver microsomes that the extent of non-specific microsomal binding of a given compound correlates with its lipophilicity 5. Most importantly, they showed that it correlates with the physicochemical properties of a given lipophilic compound. McLure et al. further support these findings by showing that acidic and neutral drugs do not bind appreciably to the microsomal membrane, but basic drugs bind to a greater extent 41. The reason behind this is thought to be due to favorable electrostatic interactions between the positively charged basic compounds and the negatively charged phosphate groups on the phospholipid bilayer 5. Due to this nonspecific binding the bound fraction of a given drug is no longer available for conversion by metabolic enzymes resulting in potential underestimation of the in vivo clearance of basic lipophilic drugs. It is, therefore, of importance to also take the nonspecific binding into consideration when predicting in vivo clearance for such drugs. On the other hand, Obach et al. showed that despite the unappreciable binding of acidic compounds the in vivo clearance of these drugs were accurately predicted when the non-specific binding was also taken into consideration 43, 44. Suggesting that this factor is an important determinant for accurately predicting clearance in humans from microsomal data. 7 Hepatocytes Fresh and cryopreserved primary human hepatocytes Fresh primary human hepatocytes (pHH) are liver cells isolated from liver tissue of humans, which are directly cultured afterwards. Consequently, their greatest advantage as in vitro systems for the prediction of in vivo drug clearance in humans is their intact plasma membrane. In contrast to microsomes, primary hepatocytes have the entire array of metabolizing enzymes of phase I and phase II, cofactors essential for these enzymes, and transporters that are responsible for drug uptake. Altogether, these components result in a representative scenario of the in vivo situation making pHH a “gold standard” for drug clearance studies. Unfortunately, fresh pHH in culture are subject to dedifferentiation. This process is triggered by the isolation method, which destroys tight and gap junctions between the cells 15. Under such trauma the quiescent primary hepatocytes enter the cell cycle and start proliferating what is also seen after partial removal of the liver in vivo 15. By starting proliferating the hepatocytes are no longer differentiated cells. Therefore, transcription factors involved in the expression of CYPs are altered resulting in decreased CYP mRNA levels and increased protein degradation 15, 50. Consequently, CYP catalytic activity and content is rapidly reduced in cultured pHH. However, it has been reported that the mRNA levels of some CYP enzymes is recovered to some extent after 72-96 hours of culture 18, 20. Moreover, the loss in CYP content has shown to be CYP specific 10. In addition to the dedifferentiation issue of pHH in culture, this in vitro system faces yet another issue, namely its short life span. They can only be kept for a maximum of 1 week in conventional monolayer cultures 10. Culturing of pHH sandwiched between layers of collagen, for example, can prolong their life span and to some extent preserve their catalytic activity 12. Drug clearance studies using sandwiched rat hepatocytes showed that these systems successfully predicted in vivo CLh for slow and fast metabolizing compounds 56. High preparationto-preparation variation in CYP activity is also found in pHH from different donors 17. This interindividual variation is seen both in the total CYP activity as well as individual CYP activity. As with HLM, pooling pHH from different donors is an easy and successful solution to overcome interindividual variation and obtain a relatively average human biotransformation profile. The only problem is that their limited availability makes it difficult to pool pHH from sufficient donors. Healthy fresh liver samples are often obtained from transplantation and surgical waste tissue 18. The limited availability of good quality samples continues to hinder the widespread use of pHH as in vitro systems for drug clearance. One way of dealing with the scarce availability of pHH is by optimizing preservation methods for these in vitro systems. Indeed, cryopreservation has led to the successful storage of pHH. By storing living material at the temperature of liquid nitrogen (-196C), all biological processes come to a standstill 12. With the help of this technique convenient use of isolated hepatocytes is possible as both phase I and phase II drug metabolizing activities are retained in cryopreserved pHH 37. Furthermore, transport activity and viability are also retained at similar levels as seen in fresh pHH 1, 11. Due to cryopreservation, pHH can be pooled thereby circumventing donor-to-donor variation, which can have major impact on the prediction of in vivo drug clearance. However, it was shown that the metabolic activity in cryopreserved pHH in culture decreased in the same way as in fresh hepatocytes in culture 37. Moreover, it has been reported that after thawing their ability to attach onto the 8 culture plate was impaired 35. Although cryopreservation made it possible to store fresh primary hepatocytes for convenient use and circumventing limited availability, the viability of these in vitro systems is still low. Several drug clearance studies showed that cryopreserved hepatocytes accurately predict in vivo clearance 8, 31, 40. On the other hand, Naritomi et al. showed that the predicted in vivo CLint of these systems for drugs with a wide range of in vivo hepatic clearance differed between 12.4 and 199-fold from the observed CLint 42. Furthermore, it was stated that underestimation of in vivo clearance by hepatocytes is dependent on the clearance rate of a compound 63. Indeed, Foster et al. showed that hepatocytes have the tendency to underestimate in vivo clearance of high clearance drugs 16. Hallifax et al. further support this by showing that underestimation by hepatocytes increased with increasing CLint 22. Both research groups suggest that this tendency may be caused by limited factors such as cofactor exhaustion or cell permeability of drugs, especially of slow diffusing compounds. As with HLM, lipophilic compounds can also bind non-specifically to the plasma membrane of hepatocytes. Moreover, Austin et al. showed that the extent of binding to hepatocytes also correlates with the physicochemical properties of a given lipophilic compound 6. Therefore, non-specific binding can affect the ability of this in vitro system to predict in vivo clearance if not taken into account. Human hepatic cell lines As pHH, human hepatic cell lines are liver-derived cells. However, they are not isolated from “normal” liver tissue, but often from primary tumors of the liver parenchyma 10. In other words, human hepatic cell lines are hepatoma cells. Therefore, these cells have long life spans and proliferate almost unlimitedly. Due to this, human hepatic cell lines are readily available. Furthermore, they are easily standardized among laboratories resulting in higher reproducibility for experiments and they have a relatively stable gene expression in culture over time 10, 14. Not surprisingly, human hepatic cell lines are sometimes considered as alternatives for pHH in drug clearance studies. There are various types of hepatic cell lines. However, HepG2 cell line is the most used and well-characterized one. In this subsection HepG2 is only used as an example to illustrate typical limitations of these in vitro systems in general and will not be used to discuss their ability to predict in vivo clearance. The latter will be discussed for another more advanced hepatic cell line below. When compared to pHH, HepG2 show similar expression of most phase II enzymes, but they lack or poorly express some phase I enzymes 60, 61. Consequently, the catalytic activities of these enzymes are also low. Westerink et al. showed that mRNA levels of most CYPs are between 100 and 1000-fold lower than those of primary hepatocytes 59. Moreover, it was reviewed that key transcription factors are poorly expressed in these cell lines thereby causing the low mRNA levels and catalytic activities of most of the CYPs 18. In addition, Guo et al. stated that cell culture environments such as the oxygen concentration in the medium matrix or its composition can alter the expression of drug metabolizing enzyme in HepG2 21. Incubation with low oxygen concentrations resulted in down-regulation of drugmetabolizing genes and using different types of medium up-regulated the expression levels of some CYPs. Furthermore, it was reported that CYP-induction is very poor in these cell lines 14. The newly established human hepatic cell line, HepaRG, is not subject to these typical limitations of hepatic cell lines. This cell line was derived from a female patient 9 suffering from hepatocarcinoma and hepatitis C infection 19. A whole genome gene expression profile comparison between HepaRG and HepG2 revealed that the former transcribe genes at similar levels to in vivo 23. Moreover, transcription factors in these systems are stable over a period of six weeks 27. Other studies showed that expressed mRNA levels of CYPs and phase II enzymes and their activity in cultured HepaRG are similar to those in pHH 20, 25, 63. Most importantly, the catalytic activity of these enzymes in culture also remains stable for a maximum of 6 weeks and can be induced at comparable levels to pHH 20, 57. Besides expressing metabolic enzymes they also express other specific markers of differentiated hepatocytes like drug transporters 14. However, as with HepG2, liver specific functions of HepaRG are altered by the cell culture environment 25. HepaRG are progenitor-like cells that have the ability to from hepatocyte-like colonies in culture. When cultured at low density and after reaching confluence, some of the undifferentiated proliferating cells differentiate into hepatocyte-like cells while others differentiate into biliary epitheliallike cells 3, 14, 19, 25. Altogether, these characteristics make this cell line a powerful tool to study drug clearance in humans. Nevertheless, one should keep in mind that with these similarities with pHH also come similar limitations. One such limitation is the aforementioned clearance-dependent underestimation of in vivo clearance. Zanelli et al. showed that extrapolation from in vitro CLint of HepaRG caused similar underestimation of the in vivo situation for high clearance drugs as pHH and suggested that this could worsen with increasing clearance 63. Moreover, their ability to predict in vivo clearance is also influenced by non-specific binding of lipophilic drugs. Precision-cut human liver slices The introduction of slicer devices enabled the cutting of thin liver slices with precise thickness ranging from 100 to 250 µm 12. Due to such small thickness considerable amounts of slices can be prepared from only a small piece of liver tissue. In comparison to the more disruptive isolation technique of hepatocytes, the preparation technique for liver slices maintains most of the architectural integrity of the liver cells thereby also maintaining the intercellular communication. In contrast to isolated primary hepatocytes, precision-cut liver slices also contain supporting cells such as Kupffer cells 30. This multicellular aspect is very important in maintaining the cell viability and activity. As with primary hepatocytes, these liver slices still have transporters after slicing 12. Most importantly, they contain active phase I and phase II enzymes 53. The complexity of these in vitro systems reflects that of the liver. Not surprisingly, they serve as mini-organ models in drug clearance studies. Unfortunately, there is a rapid loss of CYP expression and activity in culture 30, 49. This may be the cause of a loss in inductive stimuli in vitro compared to in vivo 12. Consequently, CYP mRNA levels are decreased what results in the loss of their expression and activity. The rate at which these cell functions decline was shown to be CYP-specific 49. This differential loss appears to be the result of an imbalance between production and degradation of some CYP proteins 12. Further proof for the possible cause of loss of CYP expression and activity in cultured liver slices comes from the fact that phase II enzymes are relatively stable in culture as these are less dependent on stimuli in vivo 12, 58. However, there also exists evidence that this loss might be due to dedifferentiation of liver cells in the slice edges presumably as a result of the cutting procedure 12. As with hepatocytes, precision-cut liver slices have also very short life span. If incubated with specialized incubation methods such as the dynamic organ culture (DOC) system, where slices are intermittently exposed to 10 medium and oxygen, these in vitro systems can be viable for up to 5 days 12, 46. However, the viability is still short. Another limitation is the scarcity of good healthy liver tissue for the preparation of the slices. What makes this even worse is the fact that there are no adequate protocols for preservation at present. Although Martignoni et al. successfully cryopreserved human liver slices, their viability was decreased 39. Not surprisingly, these in vitro systems are not commercially available yet. Several papers stated that liver slices poorly predict in vivo clearance, especially that of high clearance drugs 2, 10, 26, 55. By the rapid uptake of these drugs by the outer cell layer, the diffusion to the inner cell layer is limited 12. Consequently, only a fraction of the slice is intrinsically metabolically active thereby poorly predicting in vivo clearance. De Graaf et al. stated that reducing the thickness of the slices helps solve this problem 12. Despite of this many researches are still skeptical of the ability of this system to predict in vivo clearance. 11 Conclusion The drug development process costs pharmaceutical companies a great deal of money and time. With so many drugs failing to reach or stay on the market because of unfavorable drug metabolism, sufficient knowledge of the latter in an early stage of drug development is of utmost importance. In practice this is often achieved by determining the CLh of a NCE. This information gives insight into the susceptibility of a NCE to metabolism by the liver thereby providing the opportunity to disapprove NCEs with unfavorable hepatic metabolism in the earliest stages of drug development. On the other hand, clearance is also useful in determining the therapeutic dose range and regimen of a NCE in later stages. Laboratory animals have been often used as models for humans in drug clearance studies. However, at present species differences in drug metabolism is a well-known phenomenon. Most importantly, even among humans some important metabolic enzymes differ. It is for these reasons that human-derived materials are more preferred for predicting in vivo drug clearance. Therefore, the aim of this thesis was to determine what the most appropriate human-based in vitro system is for predicting hepatic clearance of drugs in humans. In order to do so, the advantages and disadvantage of the three most commonly used in vitro systems, namely HLM, human hepatocytes and precision-cut human liver slices were discussed. At present there is no “perfect” in vitro system to predict CLh in humans. Each system has its own set of advantages and limitations. Therefore, the usefulness of each in vitro system highly depends on the purpose of the study. HLM are plain simple subcellular fractions containing only some CYPs enzymes and UGTs, but they lack other determinants such as transporters, cytosolic phase II enzymes and the ability to be induced. Altogether, these aspects make it impossible for HLM to be representative models. While HLM may not be an appropriate in vitro system for predicting CLh in humans, this system can be very useful for studying various and separate metabolic pathways in drug metabolism studies. On the other hand, precision-cut human liver slices are multicellular intact systems maintaining a considerable architectural structure and intercellular communication. This complexity gives them a major advantage in serving as mini-organ models. To date, there are no adequate preservation techniques that allow their commercial availability. Most importantly, the poor penetration of compounds into the inner cell layers poses a threat to the accurate prediction of in vivo clearance from these systems. However, if preservation techniques and slice thickness were to be optimized, this in vitro system could be a powerful tool in drug clearance studies. As stated earlier, the liver is not the only metabolically active organ. Thus, slices prepared from various metabolically active extra-hepatic tissues allow direct inter-organ comparison of metabolism of a NCE 12. To date, pHH and HepaRG are, therefore, the most promising in vitro systems for predicting in vivo clearance. As intact systems possessing an intact plasma membrane, the most important metabolic enzymes of phase I and phase II, transporters, cofactors and the ability to be induced, they give a very well reflection of the in vivo situation. Even though rapid loss over time of CYP activity and content in cultured pHH due to dedifferentiation have been shown, sandwich culture between collagen layers maintains to some extent the CYP activity. Furthermore, due to the successful cryopreservation technique of fresh pHH, these in vitro systems are commercially available and pooling is possible. In contrast to pHH, HepaRG, has longer life span and a stable gene expression for up to 6 weeks in culture. 12 Progenitor-like cells like HepaRG can form hepatocyte-like colonies in culture thereby reflecting the multicellularity of the liver. Not only the capability of the in vitro systems have to be taken into account when deciding which is the most appropriate system for predicting in vivo clearance, but also influencing factors such as the culture matrix, culture method or preservation techniques that may interfere with their performance. Most importantly, it also highly depends on the class of compound to be studied and the prediction methodology used to predict in vivo clearance from the in vitro CLint data obtained from these systems. In the case of hepatocytes, more extensive researches have to be conducted on the cause of the tendency this system has to underestimate in vivo clearance of high clearance dugs. Finding the cause is crucial in choosing the most appropriate extrapolation method for accurately predicting in vivo clearance for these classes of drugs. Since the extent of non-specific binding is correlated with the physicochemical properties of a given lipophilic drugs, it would be perhaps better to use different models to correct for the unbound fraction for acidic and neutral compounds than for basic compounds in the in vitro assay medium. Austin et al. proposed using a model for acidic and neutral compound that only takes their lipophilicity into consideration, as these compounds do not bind to the bilayer membrane to a great extent 5, 6. For basic compounds he proposed a model that takes the ionized fraction into consideration, as this is the cause of non-specific binding to the phospholipid groups in the plasma membrane 5, 6. Finally, there is a need for studies that only investigate the physicochemical properties of a group of only a given class of compound in relation to the power of the in vitro systems discussed in this thesis to accurately predict in vivo clearance. By doing so, it would be much more easier to compare the different studies for a given class of compound and to choose the most appropriate in vitro system. 13 References 1. Adams RM, Wang M, Crane AM, Brown B, Darlington GJ, Ledley FD. Effective cryopreservation and long-term storage of primary human hepatocytes with recovery of viability, differentiation, and replicative potential. Cell Transplant. 1995;4:579-586.3 2. Andersson TB, Sjöberg H, Hoffmann K-, et al. An assessment of human liverderived in vitro systems to predict the in vivo metabolism and clearance of almokalant. Drug Metab Disposition. 2001;29:712-720. 3. Aninat C, Piton A, Glaise D, et al. Expression of cytochromes P450, conjugating enzymes and nuclear receptors in human hepatoma HepaRG cells. Drug Metab Disposition. 2006;34:75-83. 4. Ansede JH, Thakker DR. High-Throughput Screening for Stability and Inhibitory Activity of Compounds toward Cytochrome P450-Mediated Metabolism. J Pharm Sci. 2004;93:239-255. 5. Austin RP, Barton P, Cockroft SL, Wenlock MC, Riley RJ. The influence of nonspecific microsomal binding on apparent intrinsic clearance, and its prediction from physicochemical properties. Drug Metab Disposition. 2002;30:1497-1503. 6. Austin RP, Barton P, Mohmed S, Riley RJ. The binding of drugs to hepatocytes and its relationship to physicochemical properties. Drug Metab Disposition. 2005;33:419-425. 7. Ayrton A, Morgan P. Role of transport proteins in drug absorption, distribution and excretion. Xenobiotica. 2001;31:469-497. 14 8. Bachmann K, Byers J, Ghosh R. Prediction of in vivo hepatic clearance from in vitro data using cryopreserved human hepatocytes. Xenobiotica. 2003;33:475-483. 9. Baranczewski P, Stańczak A, Sundberg K, et al. Introduction to in vitro estimation of metabolic stability and drug interactions of new chemical entities in drug discovery and development. Pharmacological Reports. 2006;58:453-472. 10. Brandon EFA, Raap CD, Meijerman I, Beijnen JH, Schellens JHM. An update on in vitro test methods in human hepatic drug biotransformation research: Pros and cons. Toxicol Appl Pharmacol. 2003;189:233-246. 11. Brown HS, Griffin M, Houston JB. Evaluation of cryopreserved human hepatocytes as an alternative in vitro system to microsomes for the prediction of metabolic clearance. Drug Metab Disposition. 2007;35:293-301. 12. de Graaf IAM, Groothuis GMM, Olinga P. Precision-cut tissue slices as a tool to predict metabolism of novel drugs. Expert Opinion on Drug Metabolism and Toxicology. 2007;3:879-898. 13. DiPiro JT, Spruill WJ, Wade WE, Blouin RA, Pruemer JA. Lesson 2: Basic pharmacokinetics. In: Concepts in Clinical Pharmacokinetics. Fifth ed. American Society of Health-System Pharmacists, Inc; 2010:19-27. 14. Donato MT, Lahoz A, Castell JV, Gómez-Lechón MJ. Cell lines: A tool for in vitro drug metabolism studies. Curr Drug Metab. 2008;9:1-11. 15. Elaut G, Henkens T, Papeleu P, et al. Molecular mechanisms underlying the dedifferentiation process of isolated hepatocytes and their cultures. Curr Drug Metab. 2006;7:629-660. 15 16. Foster JA, Houston JB, Hallifax D. Comparison of intrinsic clearances in human liver microsomes and suspended hepatocytes from the same donor livers: Clearance-dependent relationship and implications for prediction of in vivo clearance. Xenobiotica. 2011;41:124-136. 17. Gómez-Lechón MJ, Donato MT, Castell JV, Jover R. Human hepatocytes in primary culture: The choice to investigate drug metabolism in man. Curr Drug Metab. 2004;5:443-462. 18. Gómez-Lechón MJ, Donato MT, Castell JV, Jover R. Human hepatocytes as a tool for studying toxicity and drug metabolism. Curr Drug Metab. 2003;4:292-312. 19. Gripon P, Rumin S, Urban S, et al. Infection of a human hepatoma cell line by hepatitis B virus. Proc Natl Acad Sci U S A. 2002;99:15655-15660. 20. Guillouzo A, Corlu A, Aninat C, Glaise D, Morel F, Guguen-Guillouzo C. The human hepatoma HepaRG cells: A highly differentiated model for studies of liver metabolism and toxicity of xenobiotics. Chem Biol Interact. 2007;168:66-73. 21. Guo L, Dial S, Shi L, et al. Similarities and differences in the expression of drugmetabolizing enzymes between human hepatic cell lines and primary human hepatocytes. Drug Metab Disposition. 2011;39:528-538. 22. Hallifax D, Foster JA, Houston JB. Prediction of human metabolic clearance from in vitro systems: Retrospective analysis and prospective view. Pharm Res. 2010;27:2150-2161. 23. Hart SN, Li Y, Nakamoto K, Subileau E-, Steen D, Zhong X-. A comparison of whole genome gene expression profiles of HepaRG cells and HepG2 cells to primary human hepatocytes and human liver tissues. Drug Metab Disposition. 2010;38:988994. 16 24. Hermann M, Kase ET, Molden E, Christensen H. Evaluation of microsomal incubation conditions on CYP3A4-mediated metabolism of cyclosporine A by a statistical experimental design. Curr Drug Metab. 2006;7:265-271. 25. Hewitt NJ, Lechón MJG, Houston JB, et al. Primary hepatocytes: Current understanding of the regulation of metabolic enzymes and transporter proteins, and pharmaceutical practice for the use of hepatocytes in metabolism, enzyme induction, transporter, clearance, and hepatotoxicity studies. Drug Metab Rev. 2007;39:159234. 26. Houston JB, Carlile DJ. Incorporation of in vitro drug metabolism data into physiologically- based pharmacokinetic models. Toxicology in Vitro. 1997;11:473478. 27. Kanebratt KP, Andersson TB. Evaluation of HepaRG cells as an in vitro model for human drug metabolism studies. Drug Metab Disposition. 2008;36:1444-1452. 28. Kitamura S, Maeda K, Sugiyama Y. Recent progresses in the experimental methods and evaluation strategies of transporter functions for the prediction of the pharmacokinetics in humans. Naunyn Schmiedebergs Arch Pharmacol. 2008;377:617-628. 29. Klaassen CD, Watkins III JB. Chapter 7: Toxicokinetics. In: Casarett & Doull's Essentials of Toxicology. First ed. McGraw-Hill Professional; 2003:98-107. 30. Kramer MA, Tracy TS. Studying cytochrome P450 kinetics in drug metabolism. Expert Opinion on Drug Metabolism and Toxicology. 2008;4:591-603. 31. Lau YY, Sapidou E, Cui X, White RE, Cheng K-. Development of a novel in vitro model to predict hepatic clearance using fresh, cryopreserved, and sandwichcultured hepatocytes. Drug Metab Disposition. 2002;30:1446-1454. 17 32. Lavé T, Chapman K, Goldsmith P, Rowland M. Human clearance prediction: Shifting the paradigm. Expert Opinion on Drug Metabolism and Toxicology. 2009;5:1039-1048. 33. Lewis DFV, Ioannides C, Parke DV. Cytochromes P450 and species differences in xenobiotic metabolism and activation of carcinogen. Environ Health Perspect. 1998;106:633-641. 34. Li AP. Screening for human ADME/Tox drug properties in drug discovery. Drug Discov Today. 2001;6:357-366. 35. Li AP, Lu C, Brent JA, et al. Cryopreserved human hepatocytes: Characterization of drug-metabolizing activities and applications in higher throughput screening assays for hepatotoxicity, metabolic stability, and drug-drug interaction potential. Chem Biol Interact. 1999;121:17-35. 36. Lin JH, Lu AYH. Role of pharmacokinetics and metabolism in drug discovery and development. Pharmacol Rev. 1997;49:403-449. 37. Loretz LJ, Li AP, Flye MW, Wilson AGE. Optimization of cryopreservation procedures for rat and human hepatocytes. Xenobiotica. 1989;19:489-498. 38. Martignoni M, Groothuis GMM, de Kanter R. Species differences between mouse, rat, dog, monkey and human CYP-mediated drug metabolism, inhibition and induction. Expert Opinion on Drug Metabolism and Toxicology. 2006;2:875-894. 39. Martignoni M, Monshouwer M, De Kanter R, Pezzetta D, Moscone A, Grossi P. Phase I and phase II metabolic activities are retained in liver slices from mouse, rat, dog, monkey and human after cryopreservation. Toxicology in Vitro. 2004;18:121128. 18 40. McGinnity DF, Soars MG, Urbanowicz RA, Riley RJ. Evaluation of fresh and cryopreserved hepatocytes as in vitro drug metabolism tools for the prediction of metabolic clearance. Drug Metab Disposition. 2004;32:1247-1253. 41. McLure JA, Miners JO, Birkett DJ. Nonspecific binding of drugs to human liver microsomes. Br J Clin Pharmacol. 2000;49:453-461. 42. Naritomi Y, Terashita S, Kagayama A, Sugiyama Y. Utility of hepatocytes in predicting drug metabolism: Comparison of hepatic intrinsic clearance in rats and humans in vivo and in vitro. Drug Metab Disposition. 2003;31:580-588. 43. Obach RS. Prediction of human clearance of twenty-nine drugs from hepatic microsomal intrinsic clearance data: An examination of in vitro half-life approach and nonspecific binding to microsomes. Drug Metab Disposition. 1999;27:1350-1359. 44. Obach RS. Nonspecific binding to microsomes: Impact on scale-up of in vitro intrinsic clearance to hepatic clearance as assessed through examination of warfarin, imipramine, and propranolol. Drug Metab Disposition. 1997;25:1359-1369. 45. Obach RS. The importance of nonspecific binding in in vitro matrices, its impact on enzyme kinetic studies of drug metabolism reactions, and implications for in vitroin vivo correlations. Drug Metab Disposition. 1996;24:1047-1049. 46. Olinga P, Meijer DKF, Slooff MJH, Groothuis GMM. Liver slices in in vitro pharmacotoxicology with special reference to the use of human liver tissue. Toxicology in Vitro. 1998;12:77-100. 47. Pearce RE, McIntyre CJ, Madan A, et al. Effects of freezing, thawing, and storing human liver microsomes on cytochrome P450 activity. Arch Biochem Biophys. 1996;331:145-169. 19 48. Rendic S, Di Carlo FJ. Human cytochrome P450 enzymes: A status report summarizing their reactions, substrates, inducers, and inhibitors. Drug Metab Rev. 1997;29:413-580. 49. Renwick AB, Watts PS, Edwards RJ, et al. Differential maintenance of cytochrome P450 enzymes in cultured precision-cut human liver slices. Drug Metab Disposition. 2000;28:1202-1209. 50. Rodríguez-Antona C, Donato MT, Boobis A, et al. Cytochrome P450 expression in human hepatocytes and hepatoma cell lines: Molecular mechanisms that determine lower expression in cultured cells. Xenobiotica. 2002;32:505-520. 51. Rodríguez-Antona C, Donato MT, Pareja E, Gómez-Lechón M-, Castell JV. Cytochrome p-450 mRNA expression in human liver and its relationship with enzyme activity. Arch Biochem Biophys. 2001;393:308-315. 52. Rowland M, Tozer NT. Basic considerations. In: Clinical Pharmacokinetics: Concepts and Application. Second ed. the United States: Lea & Febriger; 1989:9-16. 53. Ruiz-Garcia A, Bermejo M, Moss A, Casabo VG. Pharmacokinetics in drug discovery. J Pharm Sci. 2008;97:654-690. 54. Shitara Y, Horie T, Sugiyama Y. Transporters as a determinant of drug clearance and tissue distribution. European Journal of Pharmaceutical Sciences. 2006;27:425446. 55. Soars MG, McGinnity DF, Grime K, Riley RJ. The pivotal role of hepatocytes in drug discovery. Chem Biol Interact. 2007;168:2-15. 56. Treijtel N, Van Helvoort H, Barendregt A, Blaauboer BJ, Van Eijkeren JCH. The use of sandwich-cultured rat hepatocytes to determine the intrinsic clearance of 20 compounds with different extraction ratios: 7-Ethoxycoumarin and warfarin. Drug Metab Disposition. 2005;33:1325-1332. 57. Turpeinen M, Tolonen A, Chesne C, Guillouzo A, Uusitalo J, Pelkonen O. Functional expression, inhibition and induction of CYP enzymes in HepaRG cells. Toxicology in Vitro. 2009;23:748-753. 58. VandenBranden M, Wrighton SA, Ekins S, et al. Alterations of the catalytic activities of drug-metabolizing enzymes in cultures of human liver slices. Drug Metab Disposition. 1998;26:1063-1068. 59. Westerink WMA, Schoonen WGEJ. Cytochrome P450 enzyme levels in HepG2 cells and cryopreserved primary human hepatocytes and their induction in HepG2 cells. Toxicology in Vitro. 2007;21:1581-1591. 60. Westerink WMA, Schoonen WGEJ. Phase II enzyme levels in HepG2 cells and cryopreserved primary human hepatocytes and their induction in HepG2 cells. Toxicology in Vitro. 2007;21:1592-1602. 61. Wilkening S, Stahl F, Bader A. Comparison of primary human hepatocytes and hepatoma cell line HepG2 with regard to their biotransformation properties. Drug Metab Disposition. 2003;31:1035-1042. 62. Yamazaki H, Inoue K, Turvy CG, Guengerich FP, Shimada T. Effects of freezing, thawing, and storage of human liver samples on the microsomal contents and activities of cytochrome P450 enzymes. Drug Metab Disposition. 1997;25:168-174. 63. Zanelli U, Caradonna NP, Hallifax D, Turlizzi E, Houston JB. Comparison of cryopreserved HepaRG cells with cryopreserved human hepatocytes for prediction of clearance for 26 drugs. Drug Metab Disposition. 2012;40:104-110. 21 22