Lipid metabolism
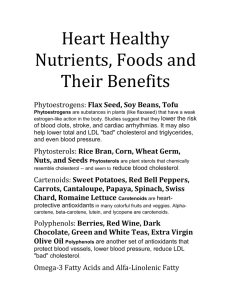
advertisement
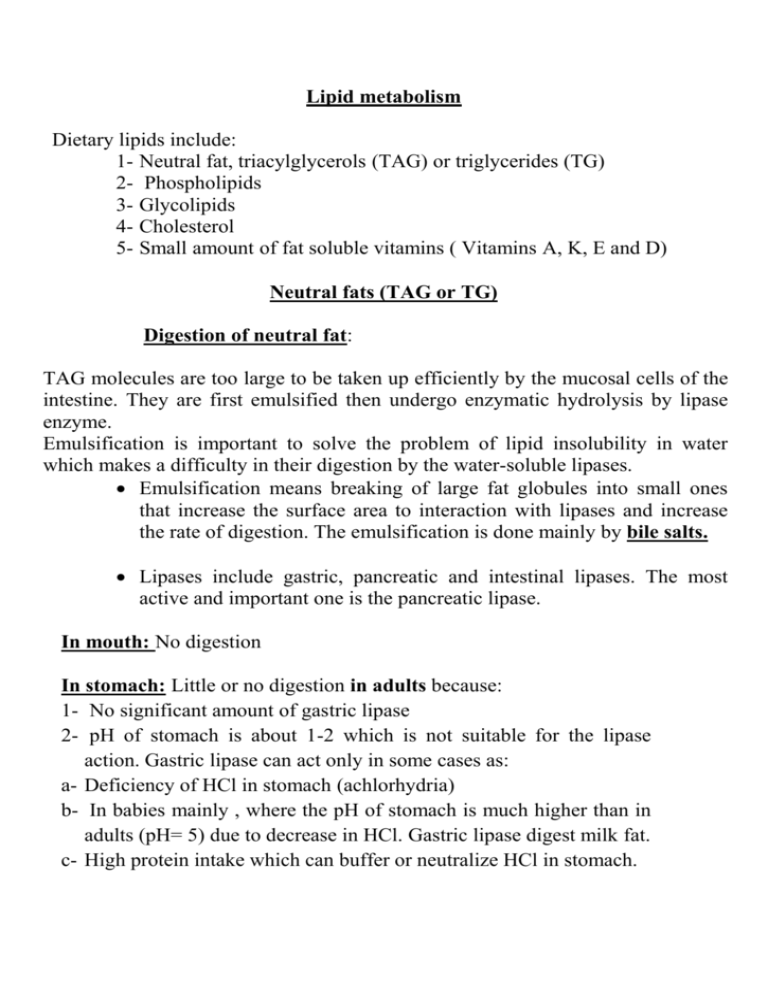
Lipid metabolism Dietary lipids include: 1- Neutral fat, triacylglycerols (TAG) or triglycerides (TG) 2- Phospholipids 3- Glycolipids 4- Cholesterol 5- Small amount of fat soluble vitamins ( Vitamins A, K, E and D) Neutral fats (TAG or TG) Digestion of neutral fat: TAG molecules are too large to be taken up efficiently by the mucosal cells of the intestine. They are first emulsified then undergo enzymatic hydrolysis by lipase enzyme. Emulsification is important to solve the problem of lipid insolubility in water which makes a difficulty in their digestion by the water-soluble lipases. Emulsification means breaking of large fat globules into small ones that increase the surface area to interaction with lipases and increase the rate of digestion. The emulsification is done mainly by bile salts. Lipases include gastric, pancreatic and intestinal lipases. The most active and important one is the pancreatic lipase. In mouth: No digestion In stomach: Little or no digestion in adults because: 1- No significant amount of gastric lipase 2- pH of stomach is about 1-2 which is not suitable for the lipase action. Gastric lipase can act only in some cases as: a- Deficiency of HCl in stomach (achlorhydria) b- In babies mainly , where the pH of stomach is much higher than in adults (pH= 5) due to decrease in HCl. Gastric lipase digest milk fat. c- High protein intake which can buffer or neutralize HCl in stomach. In intestine: The major site of lipid digestion occurs in small intestine, mainly by pancreatic lipase (steapsin) Secretion of pancreatic lipase is stimulated (regulated) by: 1- Passage of the acid gastric content (chyme) into the duodenum. 2- Hormonal regulation by secretin and cholecystokinin ( CCK, formerly called pancreozymin). Secretin: stimulates liver and pancrease to secrete watery solution rich in bicarbonate which make pH suitable for lipase action. Cholecystochinin (CCK): causes contraction of gall bladder and discharge of bile into duodenum. Also act on cells of pancrease to release digestive enzymes, lipase. Steapsin is secreted as zymogen or inactive form called: Steapsinogen that is converted into active steapsin by: bile salts ( produced by the liver and stored in gall bladder), Co-lipase (a protein produced by the pancrease) and calcium ions (Ca++) Action of steapsin (pancreatic lipase): remove fatty acids in positions 1, 3 in neutral fat, leaving 2- monoacyl glycerol (2- monoglyceride) and two fatty acids. 28% of 2- monoacyl glycerol are digested into glycerol and fatty acid as follow: So the end products of digestion are: - Glycerol, Fatty acids and monoacylglycerol 1 & 2 (α and β) Factors increasing the activity of steapsin ( pancreatic lipase): 1- Calcium ions which help to convert inactive steapsin into active one. 2- Bile salts which decrease pH from 8.5 to 6.5 which is the optimum pH for lipase 3- Number of fatty acids (FA) in fat: increase the number of FA lead to increase activity of the enzyme i.e lipase act on TG more than di and monoglycerides. 4- Length of FA in lipid: palmitic (16 C) or stearic (18 C) more hydrolysed rapidly than butyric (4C) or caproic acid. 5- Degree of unsaturation: As increase in double bond lead to increase of enzyme activity. Absorption: Long chain free fatty acids (FFA) and monoacylglycerols enter the intestinal mucosa by passive diffusion and by the help of bile salts which convert them into water soluble compounds called micells (hydrotropic action of bile salts). Lipid malabsorption: leads to increase of lipids in stool (fatty stool diarrhea or steatorrhea). Causes: 1- cystic fibrosis: decrease steapsin and lipid digestion and absorption. 2- Decrease of bile salts: decrease lipid digestion and absorption Re-synthesis of TG: FFA and monoacylglycerols in the mucosa are activated and used for re-synthesis of TAG which passes through lymphatics to blood stream and lastly to all tissues. Lipoprotein lipase or clearing factor: After fatty meal , there is a transient elevation of lipid in blood plasma usually occurs after half to 3 hours and return to normal in 5 to 6 hrs. When the lipids (TAG) are present in high concentration in blood after fatty meal, the plasma become turbid. This turbidity disappears by the action of lipoprotein lipase which hydrolyze TAG into fatty acids and glycerol. The enzyme is found also in adipose tissues, heart, lungs and skeletal muscles and activated by heparin. Free fatty acids produced by lipoprotein lipase may be oxidized to produce energy or used for synthesis of other triglycerides. Fate of TAG in tissues: A- Storage in the form of depot fat: Mainly under the skin, acting as insulator against loss of heat. Neutral fats also stored in the abdominal cavity which help in fixation of certain organs e.g. kidney. B- Excreted in milk of lactating women C- Excreted in stool D- Oxidation for energy production: Fatty acids stored in adipose tissue, in the form of neutral TAG, serve as the major fuel storage reserve in the body. In addition, fatty acid oxidation is the major source of energy to the body during starvation. Steps of fat oxidation: A- Release of fatty acids from TAG (lipolysis): This process is initiated by hormone- sensitive lipase (HSL) which removes a fatty acid from carbon 1 and/or carbon 3 of the TAG. Additional lipases specific for diacylgycerol or monoacylglycerol remove the remaining fatty acid (s). It is present in two forms: active (phosphorylated) and inactive form ( dephosphorylated). B- Oxidation of fatty acids: There are different methods of fatty acid oxidation: 1- Beta oxidation 2- Omega oxidation 3- Alpha oxidation 1- Beta oxidation( β- oxidation) It is the major pathway of oxidation (catabolism or breakdown) of saturated fatty acids in which two carbons are removed from activated fatty acid, producing acetyl CoA, NADH and FADH2 Site: in the mitochondria of all tissues particularly in the liver. So there is no fatty acid oxidation in RBCs which have no mitochondria Activation of fatty acids: Before its oxidation, fatty acid must be firstly activated. Long chain fatty acid (more than 12 carbons) are activated in cytoplasm or outer mitochondrial membrane to its active form called fatty acyl CoA. In the presence of ATP and Coenzyme A, the enzyme thiokinase (fatty Acyl CoA synthetase) catalyses the activation of long chain fatty acids into acyl CoA. Several thiokinase ar present, each specific for fatty acids of different chain length. Transport of long chain acyl CoA into mitochondria: Carnitine shuttle Activation of long chain fatty acids occur outside mitochondria. Long chain fatty acyl CoA cannot penetrate mitochondrial membrane. They need a carrier to transport them into mitochondria. This carrier is Carnitine which transports active fatty acid by the help of 3 enzymes: 1- Carnitine acyltransferase I 2- Carnitine - acylcarnitine translocase 3- Carnitine acyltransferase II Steps of transport: see figure Inhibitor of carnitine shuttle: malonyl CoA which inhibits carnitine acyltransferase I Sources of carnitine: diet (meat products), synthesized from amino acids lysine and methionine in liver and kidney. Medium and short chain fatty acids: Fatty acids shorter than 12 carbons can cross the inner mitochondrial membrane without the aid of carnitine. Once enter mitochondria, they are activated into their acyl CoA. Steps of β- oxidation: See figure Energy yield from β- oxidation: Each β- oxidation cycle yields: one NADH+H+ (which give 3 ATP via respiratory chain) one FADH2 (which give 2 ATP via respiratory chain) In addition each produced acetyl CoA oxidized through Kreb's cycle to yield 12 ATP. Note: 2 ATP are lost (utilized) in each cycle Question: Oxidation of one molecule of palmitic acid yields 129 ATP ( How?) Regulation of β- oxidation: Oxidation of fatty acids is controlled by the rate of release of free fatty acids from adipose tissues, which is inhibited by food intake and insulin, and stimulated by starvation, adrenaline, glucagon, thyroxin, glucocorticoids and growth hormone β-Oxidation of odd number fatty acids: is the same of even number fatty acids, except in the last step of oxidation, it gives propionyl CoA. Fate of Acetyl CoA: 1- Oxidation in kreb's cycle to CO2 + H2O and energy 2- Synthesis of: a- fatty acids b- ketone bodies c- cholesterol d- Adrenal cortical hormones e- Acetyl choline 3- Detoxication by conjugation e.g. sulfonamides Comparison between de novo synthesis and degradation (β-oxidation) of long chain saturated fatty acids: Synthesis Greatest flux of pathway Hormonal state favoring pathway Major tissue site Degradation After carbohydrate-rich meal In starvation High insulin Low anti-insulin hormones Low insulin High anti-insulin hormones Muscle, Liver Tissue location Primarily liver Mammary glands cytoplasm Carrier of acyl/acetyl groups between mitochondria and cytosol Citrate ( carry acetyl group from mitochondria to cytoplasm) Carnitine carry acyl group from cytosol to mitochondria mitochondria Coenzyme (H-carrier) NADPH (for reduction) NAD, FAD ( for oxidation) Two-carbon donor/product Malonyl CoA (donor of 2 carbons) Acetyl CoA (2 carbons are lost from each β-oxidation in the form of Acetyl CoA). Activator Citrate Inhibitor Long chain fatty acyl CoA (inhibits acetyl CoA carboxylase) Palmitic acid Product of pathway Malonyl CoA ( inhibits carnitine acyl transferase -I,CAT) Acetyl CoA Comparison between lipolysis and lipogenesis Lioplysis Definition Degradation of depot fat (release of FFA from depot fat) Enzymes Hormone sensitive lipase Hormonal regulation Inhibited by insulin Stimulated by glucagon, adrenaline Lipogenesis Synthesis of fat (triglycerides) from CHO and protein that exceed the body need Acetyl CoA carboxylase Fatty acid synthase Stimulated by insulin Inhibited by glucagon, adrenaline Steps of lipogenesis: 1- De novo synthesis of FA 2- Activation of fatty acids 3- Activation of glycerol 4- Condensation between FA and glycerol Activation of FA: Activation of glycerol: Types of body fat 1-Depot fat (stored fat) Definition: It is a fat stored in the fat cells of adipose tissues. The amount and composition of depot fat varies according to the nutritional state of the individuals so it is called variable elements. Source: The origin of depot fat is dietary fat and lipogenesis. Composition: Triglycerides mainly Fate: Source of energy for body by first lipolysis (release of fatty acids from fats) by hormone sensitive lipase (HSL) which is inhibited by insulin and activated by adrenaline and glucagon. 2-Tissue fat (constant element) Def. It is the fat present in each cell. It is the lipids that enter in the structure of body cells as cell membrane and mitochondria. It is not affected by hormones. It is never used as source of energy i.e. never oxidized to give energy. Depot fat 1- Variable element Tissue fat Constant element 2- Present in certain tissues as liver and adipose tissues under the skin, around certain organs as kidney 3- Formed mainly from triglycerides Present in every cells 4- Contain C, H and O only Formed mainly of cholesterol, phospholipids and glycolipids Contain C, H, O, P and N. 5- Affected by hormones (How?) Not affected by hormones 6- Used in starvation 7- Functions: source of energy, protection and insulator of heat, fixation of certain organs as kidney Not used Enter in the structure of cell membrane Never used as source of energy. Ketone bodies: Liver mitochondria have the capacity to convert acetyl CoA derived from fatty acid oxidation into ketone bodies which are: 1-Acetoacetic acid 2- β-hydroxy butyric acid 3- Acetone Functions of ketone bodies: 1- Used as source of energy. They are converted into acetyl CoA which is oxidized in Kreb's cycle to give energy. 2In prolonged fasting and starvation, ketone bodies can be used as source of energy by most tissues including brain N.B. Brain never oxidizes fatty acids but can oxidize ketone bodies within 5 to6 days of starvation. A. Synthesis of ketone bodies by the liver (Ketogenesis) Site of ketogenesis: Mitochondria of liver cells due to high activity of HMGCoA synthase, HMG- CoA- lyase. Steps of ketogenesis: See Figure Notes on ketogenesis: 1- HMG-CoA is also a precursor of cholesterol ( see latter) 2- HMG- CoA synthase is the rate limiting enzyme in the synthesis of ketone bodies and is present in significant amounts only in the liver. 3- Acetone is a volatile, nonmetabolized product that can be released in the breath. Regulation of ketogenesis: A. Inhibited after CHO diet (after meal) where insulin increases and inhibits lipolysis →↓ FFA→↓ FA oxidation → ↓ Acetyl CoA → ↓ ketogenesis. B. Simulated in fasting & starvation, low CHO diet, high fat diet and in DM (insulin decrease) →↑ lipolysis→ ↑ FFA→ ↑ FA oxidation→ ↑ Acetyl CoA → ↑ synyhesis of ketone bodies (ketogenesis). Ketolysis ( Use of Ketone bodies by peripheral tissues) Def. It is the complete oxidation (breakdown) of ketone bodies into energy + CO2 + H2O Site: Mitochondria of the extrahepatic tissues. Oxidation not occurs in liver due to the absence of thiophorase and acetoacetate thiokinase in the liver. Ketolysis also not occur in RBCs due to lack of mitochondria Steps: see figure N.B. Liver does not contain enzymes for ketolysis, so can't oxidize them Ketosis Ketone bodies formed in the liver must be passed to blood to be oxidized. Normal blood ketone bodies must not exceed 1.5-2 mg%. Ketonemia: is the increase of blood ketone bodies above normal levels. It occurs if the rate of ketogenesis increases and exceeds the rate of ketolysis. The excess ketone bodies pass to urine (ketonuria). If the condition is severe this leads to ketoacidosis (ketosis), Mechanism of ketoacidosis (ketosis): The increase of ketone bodies in blood is neutralized by blood buffers mainly bicarbonate. So bicarbonate will be decreased and this leads to decreased blood pH (acidosis). In severe cases of ketosis as in uncontrolled D.M. coma may be developed and the condition may be fatal. Causes of ketonemia and ketosis: 1- Severe diabetes mellitus There is insulin deficiency, which leads to decrease in CHO oxidation, thus the body is forced to use depot fat as the main source of energy. Lipolysis is stimulated, so acetyl CoA is produced in large amounts exceeding the capacity of kreb's. Excess acetyl CoA condenses to give more ketone bodies. 2- Starvation, low CHO and protein diet: Ketogenesis is stimulated during fast (starvation), low carbohydrate or protein diet, where the body is forced to use depot fat as source of energy. Also, there is a decrease of insulin and increase of anti insulin hormones so lipolysis is stimulated. Fatty acid (released from depot fat by hormone sensitive lipase) will transfer from adipose tissue to liver and degraded (by β-oxidation) into acetyl CoA. Elevated hepatic acetyl CoA will exceed the capacity of Kreb's. Excess acetyl CoA is condensed into ketone bodies. 3- High intake of fat diet: Excess fat intake → Excess fat oxidation → Excess acetyl CoA → increase ketogenesis → ketosis Phospholipids Phospholipids are lipids containing phosphate. They also contain alcohol (glycerol or sphingosine), fatty acids and base (choline, ethanolamine or serine). See the structures (lecture of Dr. Laila). Sources: Exogenous: from diet e.g. eggs Endogenous: In all cell. Liver is responsible for plasma phospholipids synthesis and degradation Plasma levels: The average total phospholipids are about 200 mg/dl (60% lecithins, 25% cephalins and 15% sphingomyelins). Digestion and absorption: begins in the intestine Phospholipids reaching the intestine whether in food (exogenous) or in intestinal secretion (bile or pancreatic lipase) of endogenous source are absorbed as such or hydrolyzed by certain pancreatic phospholipases: see page 1. Phospholipase A1: Act on ester bond in position1: removes the unsaturated fatty acid from lecithin or cephalin producing lysolecithin or lysocephalin. 2. Phospholipase A2 (B): act on position 2 removes the second fatty acid (saturated) from lysolecithin or lysocephalin producing glycerophosphoryl choline or glycerophosphoryl ethanolamine, respectively. 3. Phospholipase C (phosphodiesterase): act on linkage between the glycerol and phosphate giving free glycerol and phosphoryl choline or phosphoryl ethanolamins. 4. Phospholipase D (phosphatase): act on linkage between phosphate and base giving free phosphate and free base. If phospholipids absorbed as it is, they are usually absorbed with triglycerides and cholesterol. All are bound to protein called apolipoprotein B to form chylomicrons (TG + phospholipids + cholesterol + apolipoprotein B). Functions of phospholipids: 1- Enter in the structure of cell membranes and affect its permeability. 2- Help triglycerides absorption from GIT and their synthesis in liver and adipose tissues. 3- Sphingomyelines play role in nerve impulse conduction 4- Blood clooting: Platelet factor III and IV are phospholipids. 5- Phospholipids containing choline (e.g. lecithin) act as methyl donor in transmethylation reactions. 6- Phospholipids act as lipotropic factors i.e. prevent accumulation of fats in liver hence prevent fatty liver 7- Phospholipids in bile make cholesterol soluble. Their deficiency leads to cholesterol gallstones. 8- Dipamityl lecithin acts as surfactant in the lung. Synthesis of Phospholipids: A- Synthesis of lecithin (phosphatidyl choline) and cephalins (phosphatidyl ethanolamine and phosphatidyl serine): Their synthesis needs 1. Glycerol activated by ATP (by glycerokinase) giving 3- glycerophosphate. 2. Two fatty acids activated by CoA (by thiokinase) giving acyl CoA (active FA). 3. Choline (for synthesis of lecithin), ethanolamine or serine (for synthesis of cephalines) activated by ATP followed by reaction with CTP to give CDP choline or CDP ethanolamine or CDP serine. Steps of synthesis: see page 30 B- Synthesis of sphingomyelins: It is formed of sphingosine base, fatty acyl CoA, phosphate and choline. 1- Palmitic acid is activated by CoA to give palmitoyl CoA. 2- Serine is activated by PLP ( pyridoxal phosphate) 3- Combination of palmitoyl CoA with serine to form sphingosine base. 4- Then sphingosine reacts with acyl CoA to form ceramide 5- Ceramide then reacts with CDP-choline to form sphingomyreline Steps of synthesis of sphingosine base then sphingomyleine: page 32 Degradation of phospholipids: A- Lecithin and cephalins are degraded by phospholipases A1, A2 , C and D. see before (pages 27, 28) B- Sphigomyelin is degraded by sphingomyleinase (lysosomal enzymes) C- A plasma enzyme called: LCAT ( Lecithin Cholesterol Acyl Transferase) can act on the second fatty acid of lecithin converting it into lysolecithin. Lecithin + cholesterol → lysolecithin + cholesteryl ester N.B Two enzymes can give lysolecithin: phospholipase A1 and LCAT Niemann-pick disease: in children Disease resulting from deficiency of sphingomyelinase enzyme leading to accumulation of sphingomyeline in liver and spleen leading to enlargement of these organs. The disease is fatal in early life. Glycolipids or Cerebrosides - Glycolipids are composed of sphingosine base + one fatty acid + carbohydrate (usually galactose) - They do not contain phosphate group. - Glycolipids are present in large amounts in the myeline sheath of brain and nerve cells. They are present in cerebral hemispheres and so called also Cerebrosides - They are important constituent of cell membranes. Types of Glycolipids: Four types of glycolipids are known according to type of fatty acid: Kerasin → contain lignoceric acid (24 C) Phrenosin or cerebron → contain cerebronic ( hydroxy lignoceric acid) Nervon → contain nervonic acid (unsaturated lignoceric acid) Oxynervon → contain oxynervonic acid (hydroxy nervonic acid). Biosynthesis of glycolipids: 1. Synthesis of sphingosine (as before) 2. Formation of ceramide (as before) 3. Activation of galactse: Sphingosine → UDP-glucose → UDP- galactose ceramide → cerebrosides Cholesterol Sources: 1) Exogenous: from diet, it is present in egg yolk, liver and brain. 2) Endogenous: synthesized in all cells of the body from acetyl CoA. e.g. in liver (mainly), intestine, adrenal cortex, tests and skin. Plasma cholesterol: normal cholesterol level in blood is 150-250 mg/dL (average 200 mg/dL). Plasma cholesterol is derived mainly from liver and intestine. Digestion and absorption: mainly in intestine Cholesterol either exogenous (in food) or endogenous (present in intestinal secretion and bile) enter the intestine in the form of cholesterol ester. Cholesterol esterase secreted in pancreatic juice acts on cholesterol ester giving free cholesterol and fatty acids. Bile acids are necessary for activation of this enzyme. Cholesterol ester → cholesterol+ fatty acids Free cholesterol diffuses into the epithelial cells of intestine. In intestinal mucosa, the major amounts of cholesterol (about 80-90%) combine with fatty acids to form cholesterol esters which pass directly to the lymphatics to flow in lymph. Some of free cholesterol pass directly to flow in lymph then to blood. Functions of cholesterol: 1- Enter in the structure of every cell (cell membrane). 2- Gives vitamin D3 by UV radiation 3- Gives bile acids and salts and this is activated by thyroid hormone. 4- Give steroidal hormones ( hormones of adrenal cortex and sex hormones) Synthesis: Occurs mainly in cytoplasm of liver from acetyl CoA. See page 37 Regulation of cholesterol synthesis: HMG- CoA reductase is the key (rate limiting) enzyme in the biosynthesis of cholesterol. It is regulated by: - Its activity is decreased by cholesterol (feed back inhibition). Cholesterol (the end product of the pathway) acts as feed back inhibitor of the enzyme. - Its activity is stimulated by insulin and inhibited by glucagon. - Drug inhibition: Statins such as lovastatin and mevastatin are drugs structurally similar to HMG-CoA so competitively inhibit HMG-CoA reductase. They are used to decrease cholesterol levels in patients with hypercholesterolemia. - Diet: its activity activated by high CHO and fat diet and inhibited in starvation. Catabolism of cholesterol: 80-90% of cholesterol is converted (oxidized) into bile acids then to bile salts. This is activated by thyroxin hormone. Bile acids: See page 38 for synthesis Two bile acids are synthesized in liver from cholesterol, these are: cholic acid (3,7,12 trihydroxy cholanic acid) and chenodeoxy cholic acid (3,7 dihydroxy cholanic acid). Cholic acid is the most abundant bile acid in bile itself. In intestine, intestinal bacteria removes OH group at C7 (from cholic and chenodeoxy cholic acids) forming deoxycholic acid and 3-hydroxy cholanic acid (lithocholic acid), respectively. Note: Primary bile acids are cholic and chenodeoxy cholic acid Secondary bile acids are deoxycholic acid and lithocholic acid Formation of bile salts: Cholic acid is conjugated with either glycine or taurine forming glycocholic acid or taurocholic acid which then combines with Na+ or K+ to form bile salts. So, bile salts are Na+ or K+ salts of glycocholate or taurocholate. Functions of bile salts in fat metabolism: 1- Help emulsification of fats: help digestion and absorption of fats 2- Activate pancreatic lipase and cholesterol esterase 3- Stimulate the liver to secret bile juice containing more bile salts 4- Keep cholesterol in soluble form in bile juice so, prevent deposition of cholesterol and prevent cholesterol stone formation 5- Has a bactericidal effect. Disturbances in cholesterol metabolism 1- Hypercholesterolemia: i.e increased cholesterol level in blood than 250 mg/dL: Causes: 1. Hypothyrodism: lead to decreased conversion of cholesterol from blood to tissues, as thyroxin hormone help mobilization of cholesterol from blood to tissues. 2. D. M.: due to excess amount of acetyl CoA which increase synthesis of cholesterol and activation of key enzyme. 3. Obstructive jaundice: because the blocking of bile duct → ↓ excretion of cholesterol. 4. Diet rich in carbohydrates, and fats: increase the synthesis of cholesterol in liver due to: a- Increased the activity of the key enzyme (HMG-CoA reductase). b- Formation of excess acetyl CoA (from fats and CHO) than the requirements of oxidation and fatty acid synthesis. 5. Diet rich in cholesterol: ↑ amount absorbed → ↑ blood level Hypocholesterolemia: decrease of cholesterol level in blood below 150 mg/dL: 1. Hyperthyrodism: ↑ thyroid hormone→ a- ↑ oxidation of cholesterol into bile salts. b- increase mobilization of cholesterol from blood to tissues. 2. Liver disease: leads to decreased cholesterol synthesis which occurs in liver 3. Starvation: inhibits cholesterol synthesis by decreasing HMG-CoA reductase. 4. Estrogens: decrease cholesterol and prevent atherosclerosis, so, coronary heart disease rarely occurs in females during reproductive period of life. Lipoproteins The serum lipoproteins are complexes of lipids and specific proteins called "apoproteins". These proteins are synthesized in liver and are of 5 types: A, B, C, D and E. Plasma lipoproteins are: 1- Chylomicrons (CM) 2- Very low density lipoprotein (VLDL) 3- Low density lipoprotein (LDL) 4- High density lipoprotein (HDL) Function of lipoproteins: Help to transport lipids in blood. Since lipids are water insoluble, they can't be transported in blood. For their transport, they are conjugated with apoprotiens forming lipoproteins which are water soluble and can be transported in blood. e.g.: chylomicrons transport dietary lipids mainly TG from intestine→ blood→ peripheral tissues. VLDL transport lipids from liver to blood to tissues. LDL transport cholesterol from blood to tissues Composition of lipoproteins: 1. Lipoproteins are composed of a neutral lipid core (TG) surrounded by a shell of apoproteins, phospholipids and free cholesterol, all oriented so that their polar proteins are exposed to the surface of lipoprotein, thus making the particle soluble in aqueous solution. 2. Chylomicrons are the lowest of lipoproteins in density and the largest in size, contain the highest lipid and smallest protein contents. 3. VLDLs and LDLs are more dense, having higher content of protein and lower content of lipid 4. HDL is the most dense, contain the lowest amount of lipid and the highest of protein. Composition of Lipoproteins: CM VLDL LDL HDL 85 60 8 3 Protein % 2 10 22 50 Phospholipid % 8 15 20 30 Cholesterol % 5 15 50 17 apo E apo C apo E apo C apo B apo A-1 apo E apo C Neutral fat (TG) % Type of apoprotein Separation of lipoproteins: Lipoproteins can be separated by electrophoresis depending on their density and size. HDL moves faster to the anode (the smallest size) followed by VLDL, LDL, and chylomicrons which moves slowest (the largest size). Plasma lipoproteins and atherosclerosis (accumulation of cholesterol in the inner surfaces of large and medium sized arteries): Since LDL represents transport of cholesterol to tissue and HDL represents the removal of cholesterol from tissues thus: 1. Decreased HDL is associated with atherosclerosis and coronary heart disease 2. Increased HDL protects against atherosclerosis and coronary heart disease 3. LDL/HDL ratio help in predicting atherosclerosis and coronary heart disease: ↑ LDL/HDL → atherosclerosis ↓ LDL/HDL → No atherosclerosis Fatty liver Def. Accumulation of abnormal large amount of neutral fat in liver. NB. Normal amount of fat in liver is about 4% of its weight. In sever cases; amount of fat may reach up to 40% of the liver weight. If the condition is prolonged the liver cells die and replaced by fibrous tissues leading to liver cirrhosis and impaired liver function. Causes: 1) Over feeding of fats. 2) Over synthesis of fats from CHO, this due to over feeding of CHO. 3) Over mobilization of fat from depot fat to liver. This occur in starvation, DM and low CHO diet where body is forced to oxidize fats and so depot fat is mobilized into liver. 4) Under mobilization of fats from liver to blood, this due to deficiency of certain substances which are necessary for mobilization of liver fats. These substances are called" lipotropic factors" Lipotropic factors These are substances that prevent accumulation of fat in the liver. These substances convert neutral fats into phospholipids which are easily mobilized from liver to blood. Lipotropic factors include: a) Essential fatty acids: necessary for phospholipid synthesis b) Choline: necessary for phospholipid synthesis (lecithin) c) Vitamin B12 and folic acid d) Lipoic acid: it is a pancreatic hormone necessary to mobilize fat from liver e) Pantothenic acid as it gives CoA necessary for the synthesis of phospholipids f) Estrogen g) Organic compounds containing selenium