Care Cluster 1: Other Harmful Higher Risk
advertisement

DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Alcohol Harm and the
need for Specialist
Alcohol Treatment
Clustering Tool
Pilot Version 1
DRAFT
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Introduction
This example clustering tool is based on four existing instruments; the Alcohol Use Disorders
Identification Test (AUDIT)1, Severity of Alcohol Dependence Questionnaire (SADQ)2, Leeds
Dependence Questionnaire (LDQ) [Ref needed], the Mental Health Clustering Tool
(encompassing the Health of the Nation Outcome Scales (HoNOS)3, and the Summary of
Assessments of Risk and Need (SARN)4) and the Straus Bacon Social Stability Index5
The AUDIT was developed by the World Health Organization (WHO) as a simple method of
screening for excessive drinking and to assist in assessment.
The SADQ is a self-administered, 20-item questionnaire developed by the Addiction
Research Unit at the Maudsley Hospital. It measures the severity of dependence on alcohol.
The LDQ is a short, self-administered, 10-item questionnaire developed by the Leeds Addiction
Unit. It measures the severity of dependence on alcohol.
The Straus Bacon Social Stability Index (SSI) is a prognostic indicator for the outcomes of
specialist alcohol treatment (see Appendix).
The Mental Health Clustering Tool (MHCT) is based on the HoNOS and SARN scales:
HoNOS is an internationally recognised outcome measure developed by the Royal College of
Psychiatrists Research Unit (CRU) to measure health and social functioning outcomes in mental
health services. The aim of the HoNOS was to produce a brief measure capable of being
completed routinely by clinicians and recorded as part of a minimum mental health dataset.
SARN was developed by the Care Pathways and Packages Project to aid in the process of
establishing a classification of service users based on their needs so that appropriate service
responses could be developed both at the individual and service level.
The MHCT and SSI scores can be helpful when assigning a patient to an appropriate
cluster. For example, a patient whose AUDIT and SADQ score may indicate that they
should be assigned to the Moderate/Severe Dependence cluster may be assigned to the ‘+
complex needs cluster’ because of additional complicating factors – identified through
the MHCT and SSI items and the package of care they should receive.
In this example, clients are allocated into clusters following a routine assessment, principally
using AUDIT, SADQ or LDQ scores and ‘units per day’ together with their scores on the SSI, and
MHCT scales. These clusers are:
1. Harmful/mild dependence
2. Moderate dependence
3. Severe dependence
4. Moderate/severe dependence + complex needs
1
Babor, T.F.; de la Fuente, J.R.; Saunders, J.; and Grant, M. AUDIT. The Alcohol Use Disorders
Identification Test. Guidelines for use in primary health care. Geneva, Switzerland: World Health
Organization, 1992
2 Stockwell, T., Sitharan, T., McGrath, D. & Lang (1994). The measurement of alcohol dependence and impaired
control in community samples. Addiction, 89, 167–174
3 Wing J, Curtis RH & Beevor A (1999) Health of the Nation Outcome Scales for Children and Adolescents
(HoNOSCA). Glossary for HoNOS score sheet. The British Journal of Psychiatry May 174: 432-434
4 Self, R., Rigby, A. M., Leggett, C. & Paxton, R. 2007. Clinical Decision Support Tool: A Rational Needs-Based
Approach to Making Clinical Decisions. Journal of Mental Health, 17(1):33-48
5 Straus, R. & Bacon, S. D. (1951). A study of occupational integration of 2023 male clinic patients. Quarterly Journal
of Studies on Alcohol, 12, 231-260.
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
2
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Care Cluster 1: Harmful/mild dependence
Description
This group will have definite but minor problems, including:
A desire to drink alcohol at every appropriate opportunity (e.g. evenings, lunchtimes, weekends)
{HoNOS 3}
During periods of drinking, has occasional difficulties in controlling behaviour in terms of its onset,
termination, or levels of use of alcohol {HoNOS 1}
Increasingly opting to drink rather than pursuing alternative pleasures or interests
Levels of alcohol becoming a concern to self and/or others
Neglect of family or household chores {HoNOS 9, 10}
Repeated absences or poor work performance related to alcohol consumption {HoNOS 12}
Consumes alcohol in situations that could be physically hazardous (e.g. driving, working with
machinery)
Occasionally low in mood as a consequence of heavy drinking {HoNOS 7}
Diagnoses
F10 - Mental and behavioural disorders due to use of alcohol
F19 - Mental and behavioural disorders due to multiple drug use and use of other psychoactive substances
Impairment
Unlikely to cause disruption to wider functioning
Risk
Unlikely to be an issue
Course
The problem is likely to be short term if addressed and related to life events
Audit
SADQ or
LDQ
Units per day
No
1
2
3
4
5
6
7
8
9
10
11
12
13
A
B
C
D
E
16+
<15
<10
<15
Stable employment
Stable residence
Current residence
Current marital (or
cohabiting) relationship
Yes
Yes
Yes
Yes
No
No
No
No
Likely to score
May score
Unlikely to score
Item Description
HoNOS
Overactive, aggressive, disruptive or agitated behaviour (current)
Non-accidental self-injury
Problem-drinking or drug-taking (current)
Cognitive problems (current)
Physical Illness
Problems associated with hallucinations and delusions (current)
Depressed Mood
Other Symptoms
Relationships
Activities of Daily Living
Living Conditions
Occupation and Activities
Strong unreasonable beliefs occurring in non-psychotic disorders only.
(current)
SARN
Agitated behaviour/ expansive mood (historical)
Repeat self-harm (historical)
Safeguarding children & vulnerable dependent adults
Engagement
Vulnerability
0
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
1
Score
2
3
3
4
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Care Cluster 2: Moderate dependence
Description
This group will have a range of symptoms, including:
An urge to drink alcohol at appropriate and often inappropriate times (e.g. during working hours)
{HoNOS 3}
Has occasional difficulties in controlling behaviour in terms of its onset, termination, or levels of use of
alcohol
Some evidence of physiological symptoms when alcohol use has ceased or been reduced
Evidence of tolerance
Increasingly neglects alternative pleasures or interests because of alcohol use {HoNOS 10}
Occasionally spending more time to obtain or drink alcohol or to recover from its effects
Persisting with alcohol use despite expressed concern of others
Depressive mood states consequent to periods of heavy drinking {HoNOS 7}
Diagnoses
F10 - Mental and behavioural disorders due to use of alcohol
F19 - Mental and behavioural disorders due to multiple drug use and use of other psychoactive substances
Impairment
Impaired role functioning and problems with relationships
Risk
Self harm, physical injury due to intoxication, safeguarding may be an issue
Course
Ongoing problems
Audit
SADQ or
LDQ
Units per day
No
1
2
3
4
5
6
7
8
9
10
11
12
13
A
B
C
D
E
20+
16 - 30
10 - 22
>15
Stable employment
Stable residence
Current residence
Current marital (or
cohabiting) relationship
Yes
Yes
Yes
Yes
Likely to score
May score
Unlikely to score
No
No
No
No
Item Description
HoNOS
Overactive, aggressive, disruptive or agitated behaviour (current)
Non-accidental self-injury
Problem-drinking or drug-taking (current)
Cognitive problems (current)
Physical Illness
Problems associated with hallucinations and delusions (current)
Depressed Mood
Other Symptoms
Relationships
Activities of Daily Living
Living Conditions
Occupation and Activities
Strong unreasonable beliefs occurring in non-psychotic disorders
only. (current)
SARN
Agitated behaviour/ expansive mood (historical)
Repeat self-harm (historical)
Safeguarding children & vulnerable dependent adults
Engagement
Vulnerability
0
1
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Score
2
3
4
4
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Care Cluster 3: Severe dependence
Description
This group will have a wide range of symptoms, including:
strong desire or sense of compulsion to drink alcohol {HoNOS 3}
difficulties in controlling behaviour in terms of its onset, termination, or levels of use of alcohol
physiological withdrawal state when alcohol use has ceased or been reduced
evidence of tolerance; neglect of alternative pleasures or interests because of alcohol use
increased amount of time necessary to obtain or drink alcohol or to recover from its effects
persisting with alcohol use despite clear evidence of overtly harmful consequences, such as harm to
the liver through excessive drinking {HoNOS 5}
depressive mood states consequent to periods of heavy drinking, or impairment of cognitive
functioning {HoNOS 7}
Diagnoses
F10 - Mental and behavioural disorders due to use of alcohol
F19 - Mental and behavioural disorders due to multiple drug use and use of other psychoactive substances
Impairment
Poor role functioning with severe problems with relationships
Risk
Self harm, physical injury due to intoxication, over dependent and often hostile engagement with service,
safeguarding may be an issue
Course
Enduring problems
Audit
SADQ or
LDQ
Units per day
No
1
2
3
4
5
6
7
8
9
10
11
12
13
A
B
C
D
E
20+
>30
>22
>30
Stable employment
Stable residence
Current residence
Current marital (or
cohabiting) relationship
Yes
Yes
Yes
Yes
No
No
No
No
Likely to score
May score
Unlikely to score
Item Description
HoNOS
Overactive, aggressive, disruptive or agitated behaviour (current)
Non-accidental self-injury
Problem-drinking or drug-taking (current)
Cognitive problems (current)
Physical Illness
Problems associated with hallucinations and delusions (current)
Depressed Mood
Other Symptoms
Relationships
Activities of Daily Living
Living Conditions
Occupation and Activities
Strong unreasonable beliefs occurring in non-psychotic disorders
only. (current)
SARN
Agitated behaviour/ expansive mood (historical)
Repeat self-harm (historical)
Safeguarding children & vulnerable dependent adults
Engagement
Vulnerability
0
1
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Score
2
3
5
4
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Care Cluster 4: Moderate/severe dependence + complex needs
Description
This group will have a range of symptoms, as described above for moderate or severe dependence and in
addition may have significant health, psychological or social problems which out them at more risk, such as:
Behavioural problems
Cognitive problems
Physical illness/health problems
Hallucinations/delusions
Lack of supportive relationships
Poor living conditions/homelessness
Self-harm
Diagnoses
F10 - Mental and behavioural disorders due to use of alcohol
F19 - Mental and behavioural disorders due to multiple drug use and use of other psychoactive substances
Impairment
Poor role functioning with severe problems with relationships
Risk
Self harm, physical injury due to intoxication, over dependent and often hostile engagement with service,
safeguarding may be an issue
Course
Enduring problems
Audit
SADQ or
LDQ
Units per day
No
1
2
3
4
5
6
7
8
9
10
11
12
13
A
B
C
D
E
20+
>15
>10
>15
Stable employment
Stable residence
Current residence
Current marital (or
cohabiting) relationship
Yes
Yes
Yes
Yes
No
No
No
No
Likely to score
May score
Unlikely to score
Item Description
HoNOS
Overactive, aggressive, disruptive or agitated behaviour (current)
Non-accidental self-injury
Problem-drinking or drug-taking (current)
Cognitive problems (current)
Physical Illness
Problems associated with hallucinations and delusions (current)
Depressed Mood
Other Symptoms
Relationships
Activities of Daily Living
Living Conditions
Occupation and Activities
Strong unreasonable beliefs occurring in non-psychotic disorders
only. (current)
SARN
Agitated behaviour/ expansive mood (historical)
Repeat self-harm (historical)
Safeguarding children & vulnerable dependent adults
Engagement
Vulnerability
0
1
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Score
2
3
6
4
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Measuring outcome
Measures:
A battery of measures could be used for outcome measurement, including:
HoNOS, SADQ/LDQ, AUDIT, all of which are quick and easy to administer and are validated.
HoNOS is an internationally recognised outcome measure developed by the Royal College of
Psychiatrists Research Unit (CRU) to measure health and social functioning outcomes in mental
health services. It could be used to evaluate outcome against some of the areas of complexity that
treatment interventions (services) may address (e.g. physical health problem, depression,
relationships, living conditions etc).
The SADQ/ LDQ measure levels of dependence. The instruments are capable of measuring
change in dependence and can therefore be used to follow treatment progress and evaluate
treatment outcomes.
The AUDIT was developed by the World Health Organization (WHO) as a simple method of
screening for excessive drinking and to assist in assessment, however, re-administration of the
AUDIT can serve as the basis for measuring quantitative outcomes.
The Straus Bacon Social Stability Index (SSI) is a prognostic indicator for the outcomes of
specialist alcohol treatment.
Process:
Services providers would routinely use AUDIT, SASQ / LDQ, SSI and HoNOS/SARN in order to
track each individual’s progress. Ratings would be carried at initial assessment, admission,
review and discharge as part of the service user’s routine care pathway. Outcome data from the
scores would be used with commissioners and service users in order to provide an indication of
progress and future care provision.
Completion of the scales should only take a few minutes and can be used alongside other
outcome measures, such as the Alcohol Star, should local commissioners and providers choose
to do so. However, these locally determined measures would not form part of the minimum data
set.
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
7
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
APPENDIX
HoNOS Items
1. Overactive, aggressive, disruptive or agitated behaviour (current)
Include such behaviour due to any cause 0 No problem of this kind during the period rated.
(eg drugs, alcohol, dementia, psychosis,
1 Irritability, quarrels, restlessness etc not
depression, etc).
Do not include bizarre behaviour rated at requiring action.
Scale 6.
2 Includes aggressive gestures, pushing or
pestering others; threats or verbal aggression;
lesser damage to property (eg broken cup,
window);marked over-activity or agitation.
3 Physically aggressive to others or animals
(short of rating 4); threatening manner; more
serious over-activity or destruction of property.
4 At least one serious physical attack on others
or on animals; destructive of property (eg firesetting); serious intimidation or obscene
behaviour.
Rate 9 if not known
Could include: criminal damage, public disorder, domestic violence
2. Non-accidental self-injury (current)
Include such behaviour due to any cause
(eg drugs, alcohol, dementia, psychosis,
depression, etc).
Do not include bizarre behaviour
rated at Scale 6.
0 No problem of this kind during the period rated.
1 Fleeting thoughts about ending it all but little
risk during the period rated; no self-harm.
2 Mild risk during the period rated; includes nonhazardous self-harm (eg wrist-scratching).
3 Moderate to serious risk of deliberate self-harm
during the period rated; includes preparatory acts
(eg collecting tablets).
4 Serious suicidal attempt and/or serious
deliberate self-injury during the period rated.
Rate 9 if Not Known
3. Problem-drinking or drug-taking (current)
Do not include aggressive/destructive
behaviour due to alcohol or drug use,
rated at Scale 1.
Do not include physical illness or
disability due to alcohol or drug use,
rated at Scale 5.
0 No problem of this kind during the period rated.
1 Some over-indulgence but within social norm.
2 Loss of control of drinking or drug-taking, but
not seriously addicted.
3 Marked craving or dependence on alcohol or
drugs with frequent loss of control; risk taking
under the influence.
4 Incapacitated by alcohol/drug problem.
Rate 9 if Not Known
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
8
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
4. Cognitive problems (current)
Include problems of memory, orientation
and understanding associated with any
disorder: learning disability, dementia,
schizophrenia, etc
Do not include temporary problems (eg
hangovers) resultingfrom drug/alcohol
use, rated at Scale 3.
0 No problem of this kind during the period rated.
1 Minor problems with memory or understanding
(eg forgets names occasionally).
2 Mild but definite problems (eg has lost the way
in a familiar place or failed to recognise a familiar
person); sometimes mixed up about simple
decisions.
3 Marked disorientation in time, place or person;
bewildered by everyday events; speech is
sometimes incoherent; mental slowing.
4 Severe disorientation (eg unable to recognise
relatives); at risk of accidents; speech
incomprehensible; clouding or stupor.
Rate 9 if Not Known
5. Physical illness or disability problems (current)
0 No physical health problem
Include illness or disability from any
during the period rated.
cause that limits or prevents
movement, or impairs sight or
1 Minor health problems during the period (eg
hearing, or otherwise interferes with
cold, non-serious fall, etc).
personal functioning.
Include side-effects from medication;
2 Physical health problem imposes mild
effects of drug/alcohol use; physical
restriction on mobility and activity.
disabilities resulting from accidents or
3 Moderate degree of restriction on activity
self- harm associated with cognitive
due to physical health problem.
problems, drink-driving, etc
4 Severe or complete incapacity due to
physical health problem.
Rate 9 if Not Known
Could include: Pregnant
6. Problems associated with hallucinations and delusions (current)
0 No evidence of hallucinations or delusions
Include hallucinations and delusions
during the period rated.
irrespective of diagnosis.
Include odd and bizarre behaviour
1 Somewhat odd or eccentric beliefs not in
associated with hallucinations or
keeping with cultural norms.
delusions.
Do not include aggressive, destructive or
2 Delusions or hallucinations (eg voices, visions)
overactive behaviours attributed to
are present, but there is little distress to patient or
hallucinations or delusions, rated at
manifestation in bizarre behaviour, ie clinically
Scale 1.
present but mild.
3 Marked preoccupation with delusions or
hallucinations, causing much distress and/or
manifested in obviously bizarre behaviour, ie
moderately severe clinical problem.
4 Mental state and behaviour is seriously and
adversely affected by delusions or hallucinations,
with severe impact on patient.
Rate 9 if Not Known
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
9
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
7. Problems with depressed mood (current)
Do not include suicidal ideation or
attempts, rated at Scale 2.
0 No problem associated with depressed mood
during the period rated.
1 Gloomy; or minor changes in mood.
2 Mild but definite depression and distress (eg
feelings of guilt; loss of self-esteem).
3 Depression with inappropriate self-blame;
preoccupied with feelings of guilt.
4 Severe or very severe depression, with
guilt or self-accusation.
Rate 9 if Not Known
8. Other mental and behavioural problems (current)
Rate only the most severe clinical problem 0 No evidence of any of these problems during
period rated.
not considered at scales 7 as follows.
1 Minor problems only.
Specify the type of problem by
entering the appropriate letter: A
2 A problem is clinically present at a mild level
phobic; B anxiety; C obsessive(eg patient has a degree of control).
compulsive; D mental strain/tension;
E dissociative; F somatoform; G
3 Occasional severe attack or distress, with
loss of control (eg has to avoid anxiety
eating; H sleep; I sexual; J other,
provoking situations altogether, call in a
specify.
neighbour to help, etc) ie moderately severe
level of problem.
4 Severe problem dominates
most activities.
Rate 9 if Not Known
9. Problems with relationships (current)
Rate the patient's most severe
problem associated with active or
passive withdrawal from social
relationships, and/or non-supportive,
destructive or self-damaging
relationships.
0 No significant problem during the period.
1 Minor non-clinical problems.
2 Definite problem in making or sustaining
supportive relationships; patient complains
and/or problems are evident to others.
3 Persisting major problem due to active or
passive withdrawal from social relationships
and/or to relationships that provide little or no
comfort or support.
4 Severe and distressing social isolation due to
inability to communicate socially and/or
withdrawal from social relationships.
Rate 9 if Not Known
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
10
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
10. Problems with activities of daily living (current)
0 No problem during period rated; good ability
Rate the overall level of functioning in
to function in all areas.
activities of daily living (ADL) (eg
problems with basic activities of self-care
1 Minor problems only (eg untidy,
such as eating, washing, dressing, toilet;
disorganised).
also complex skills such as budgeting,
2 Self-care adequate, but major lack of
organising where to live, occupation and
performance of one or more complex skills
recreation, mobility and use of transport,
(see left).
shopping, self- development, etc).
3 Major problem in one or more areas of self Include any lack of motivation
care (eating, washing, dressing, toilet) as well
for using self-help opportunities,
as major inability to perform several complex
since this contributes to a lower
skills.
overall level of functioning.
Do not include lack of opportunities
4 Severe disability or incapacity in all or nearly all
areas of self-care and complex skills.
for exercising intact abilities and
skills, rated at Scales 11-12.
Rate 9 if Not known
11. Problems with living conditions (current)
Rate the overall severity of problems with
the quality of living conditions and daily
domestic routine. Are the basic
necessities met (heat, light, hygiene)? If
so, is there help to cope with disabilities
and a choice of opportunities to use skills
and develop new ones?
Do not rate the level of functional
disability itself, rated at Scale 10.
NB: Rate patient's usual situation. If in
ward/hostel, rate activities during period
before admission. If information not
available, rate 9.
0 Accommodation and living conditions are
acceptable; helpful in keeping any disability
rated at Scale 10 to the lowest level
possible, and supportive of self-help.
1 Accommodation is reasonably acceptable
although there are minor or transient problems
(eg not ideal location, not preferred option,
doesn't like the food, etc).
2 Significant problem with one or more aspects
of the accommodation and/or regime (eg
restricted choice; staff or household have little
understanding of how to limit disability or how to
help use or develop new or intact skills).
3 Distressing multiple problems with
accommodation (eg some basic necessities
absent); housing environment has minimal or
no facilities to improve patient's independence.
4 Accommodation is unacceptable (eg lack of
basic necessities, patient is at risk of eviction, or
'roofless', or living conditions are otherwise
intolerable) making patient's problems worse.
Rate 9 if Not Known
Could include: Living alone, unsupported at home
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
11
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
12. Problems with occupation and activities (current)
0 Patient's day-time environment is acceptable:
Rate the overall level of problems with
helpful in keeping any disability rated at Scale
quality of day-time environment. Is
10 to the lowest level possible, and supportive
there help to cope with disabilities, and
of self help.
opportunities for maintaining or
improving occupational and recreational
1 Minor or temporary problems (eg late giro
cheques): reasonable facilities available but
skills and activities? Consider factors
not always at desired times, etc
such as stigma, lack of qualified staff,
access to supportive facilities eg
2 Limited choice of activities; lack of
staffing and equipment of day centres,
reasonable tolerance (eg unfairly refused entry
to public library or baths, etc); handicapped by
workshops, social clubs, etc.
lack of a permanent address; insufficient carer
Do not rate the level of functional
or professional support; helpful day setting
disability itself, rated at Scale 10.
available but for very limited hours.
NB: Rate patient's usual situation. If in a
ward/hostel, rate activities during period
before admission. If information not
available, rate 9
3 Marked deficiency in skilled services available
to help minimise level of existing disability; no
opportunities to use intact skills or add new ones;
unskilled care difficult to access.
4 Lack of any opportunity for daytime activities
makes patient's problems worse.
Rate 9 if Not Known
Could include: Employment problems, readiness to work, volunteering
13. Strong unreasonable beliefs occurring in non-psychotic disorders only. (current)
0 No Strong unreasonable beliefs evident.
Rate any apparent strong unreasonable
beliefs (found in some people with
disorders such as Obsessive Compulsive 1 Holds illogical or unreasonable belief(s) but has
insight into their lack of logic or reasonableness
Disorder, Anorexia Nervosa, personality
and can challenge them most of the time and
disorder, morbid jealousy etc)
they have only a minor impact on the individual’s
Do not include Delusions rated at scale
life.
6.
Do not include Severity of disorders listed
2 Holds illogical or unreasonable belief(s) but
above where
individual has insight into their lack of logic or
strong unreasonable beliefs are not
reasonableness. Belief(s) can be successfully
present – rated at Scale9.
challenged by individual on occasions. Does not
Do not include Beliefs / behaviours
have a significant negative impact on the
consistent with aperson’s culture.
person’s life.
3 Holds strong illogical and unreasonable
belief(s) but has some insight into the relationship
between the beliefs and the disorder. Belief(s)
can be ‘shaken’ by rational argument. Tries to
resist belief but with little
effect. Has a significant negative impact on
person’s life. The disorder makes treatment more
difficult than usual.
4 Holds strong illogical or unreasonable belief(s)
with little or no insight in the relationship between
the belief and the disorder. Belief(s) cannot be
‘shaken’ by rational argument. Does not attempt
to resist belief(s). Has a significant negative
impact on the person’s life or other people’s lives
and the disorder is very resistant to treatment.
Rate 9 if not known
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
12
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
Historical Ratings
For scales C-E, rate problems that occur in an episodic or unpredictable way. Whilst there may
not be any direct observation or report of a manifestation during the last two weeks the
evidence and clinical judgement would suggest that there is still a cause for concern that
cannot be disregarded (ie no evidence to suggest that the person has changed since the last
occurrence either as a result of time, therapy, medication or environment etc). In these
circumstances, any event that remains relevant to the current plan of care should be included
A. Agitated behaviour/ expansive mood (historical)
Rate agitation and overactive behaviour
causing disruption to social role functioning.
Behaviour causing concern or harm to others.
Elevated mood that is out of proportion to
circumstances.
Include such behaviour due to any cause (eg
drugs, alcohol, dementia, psychosis,
depression etc).
Excessive irritability, restlessness,
intimidation, obscene behaviour and
aggression to people animals or property.
Do not include odd or bizarre behaviour to be
rated at Scale 6.
0 No needs in this area.
1 Presents as irritable, argumentative with some
agitation. Some signs of elevated mood or agitation not
causing disruption to functioning.
2 Makes verbal/gestural threats. Pushes/pesters but no
evidence of intent to cause serious harm. Causes
minor damage to property (eg glass or crockery). Is
obviously over-active or agitated.
3 Agitation or threatening manner causing fear in
others. Physical aggression to people or animals.
Property destruction. Serious levels of elevated mood,
agitation, restlessness causing significant disruption to
functioning.
4 Serious physical harm caused to persons/animals.
Major destruction of property. Seriously intimidating
others or exhibiting highly obscene behaviour.
Elevated mood, agitation, restlessness causing
complete disruption.
Rate 9 if not known
B. Repeat self-harm (historical)
Rate repeat acts of self harm with the
intention of managing people, stressful
situations, emotions or to produce mutilation
for any reason.
Include self cutting, biting, striking, burning,
breaking bones or taking poisonous
substances etc.
Do not include accidental self-injury (due eg
to learning disability or cognitive impairment);
the cognitive problem is rated at Scale 4 and
the injury at Scale 5.
Do not include harm as a direct consequence
of drug/alcohol use (eg liver damage) to be
rated at Scale 3. Injury sustained whilst
intoxicated to be rated at Scale 5.
Do not include harm with intention of killing
self rated at Scale 2.
0 No problem of this kind.
1 Superficial scratching or non-hazardous doses of
drugs.
2 Superficial cutting, biting, bruising etc or small
ingestions of hazardous substances unlikely to lead to
significant harm even if hospital treatment not sought.
3 Repeat self-injury requiring hospital treatment.
Possible dangers if hospital treatment not sought.
However, unlikely to leave lasting severe damage even
if behaviour continues providing hospital treatment
sought.
4 Repeat serious self-injury requiring hospital
treatment and likely to leave lasting severe damage if
behaviour continues (ie, severe scarring, crippling or
damage to internal organ) and possibly to death.
Rate 9 if not known
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
13
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
C. Safeguarding Children & Vulnerable Dependent Adults (historical)
0 No obvious impact of the individuals' illness or
Rate the potential or actual impact of the
behaviour on the safety or well being of vulnerable
patient's mental illness, or behaviour, on the
persons.
safety and well being of vulnerable and
dependent persons, including children,
1 Mild concerns about the impact of the individual's
illness or behaviour on the safety or well-being of
vulnerable adults and dependent elders.
vulnerable persons.
Include any patient who lives in a household
with children under the age of 18 years.
2 Illness or behaviour has an impact on the safety
Include any patient who has substantial access or well being of vulnerable persons. The
and contact with children or other vulnerable
individual is aware of the potential impact but is
supported and is able to make adequate
persons.
arrangements.
Do not include challenge to relations covered
in scale 9
3 Illness or behaviour has an impact on the safety
or well being of vulnerable persons but does not
meet the criteria to score 4. There may be
delusions, suicide risk or self-harm. However, the
individual has insight, can take action to
significantly reduce the impact of their behaviour
on the children and is adequately supported.
4 Without action the illness or behaviour is likely to
have direct or indirect significant impact on the safety
or well-being of vulnerable persons. Problems such as
delusions, severe suicide risk or problems of impulse
control may be present. There may be lack of insight,
an inability or unwillingness to take precautions to
protect vulnerable persons and/or lack of adequate
support and protection for vulnerable persons.
Rate 9 if not known
D. Engagement (historical)
Rate the individual's motivation and
understanding of their problems, acceptance
of their care/treatment and ability to relate to
care staff.
Include the ability, willingness or motivation
to engage in their care/ treatment
appropriately, agreeing personal goals,
attending appointments. Dependency
issues.
Do not include failure to comply due to
practical reasons.
0 Has ability to engage/disengage appropriately
with services. Has good understanding of problems
and care plan.
1 Some reluctance to engage or slight risk of
dependency. Has understanding of own
problems.
2 Occasional difficulties in engagement ie missed
appointments or contacting services between
appointments inappropriately. Some
understanding of own problems.
3 Contacts services inappropriately. Has little
understanding of own problems. Unreliable
attendance at appointments. Or attendance
depends on prompting or support.
4 Contacts multiple agencies ie GP, A & E etc,
constantly. Little or no understanding of own
problems. Fails to comply with planned care. Rarely
attends appointments. Refuses service input. Or
Attendance and compliance dependent on intensive
prompting and support.
Rate 9 if not known
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
14
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
E. Vulnerability (historical)
Rate failure of an individual to protect
themselves from risk of harm to their health
and safety or well-being.
Include physical, sexual, emotional and
financial exploitation or harm/ harassment
Do not include problems of engagement rated
at scale D
0 No vulnerability evident.
1 No significant impact on person's health,
safety or well-being.
2 Concern about the individual's ability to protect their
health, safety or well-being requiring support or
removal of existing support would increase concern.
3 Clear evidence of significant vulnerability
affecting the individuals ability to protect their
health and safety or well-being that requires
support (but not as severe as a score of 4). Or
removal of existing support would increase risk.
4 Severe vulnerability - total breakdown in individual's
ability to protect themselves resulting in major risk to
the individual's health, safety or well- being.
Rate 9 if not known
Could include: Past medical history, history of fits when in withdrawal
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
15
AUDIT
Scoring system
Questions
0
1
2
3
4
Never
Monthly
or less
2-4
times
per
month
2-3
times
per
week
4+
times
per
week
How many units of alcohol do you drink on a
typical day when you are drinking?
1 -2
3-4
5-6
7-9
10+
How often have you had 6 or more units if female, or 8
or more if male, on a single occasion in the last year?
Never
Less
than
monthly
Monthly
Weekly
Daily or
almost
daily
How often during the last year have you found that you
were not able to stop drinking once you had started?
Never
Less
than
monthly
Monthly
Weekly
Daily or
almost
daily
How often during the last year have you failed to do
what was normally expected from you because of your
drinking?
Never
Less
than
monthly
Monthly
Weekly
Daily or
almost
daily
How often during the last year have you needed an
alcoholic drink in the morning to get yourself going after
a heavy drinking session?
Never
Less
than
monthly
Monthly
Weekly
Daily or
almost
daily
How often during the last year have you had a feeling of
guilt or remorse after drinking?
Never
Less
than
monthly
Monthly
Weekly
Daily or
almost
daily
How often during the last year have you been unable to
remember what happened the night before because you
had been drinking?
Never
Less
than
monthly
Monthly
Weekly
Daily or
almost
daily
How often do you have a drink containing alcohol?
Have you or somebody else been injured as a result of
your drinking?
No
Has a relative or friend, doctor or other health worker
been concerned about your drinking or suggested that
you cut down?
No
Yes, but
not in
the last
year
Yes, but
not in
the last
year
Your
score
Yes,
during
the last
year
Yes,
during
the last
year
Scoring: 0 – 7 Lower risk, 8 – 15 Increasing risk,
16 – 19 Higher risk, 20+ Possible dependence
SCORE
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
16
SEVERITY OF ALCOHOL DEPENDENCE QUESTIONAIRE (SADQ-C)1
NAME____________________________________AGE____________No._______
DATE:
Please recall a typical period of heavy drinking in the last 6 months.
When was this? Month:. Year..
Please answer all the following questions about your drinking by circling your most appropriate
response.
During that period of heavy drinking
1. The day after drinking alcohol, I woke up feeling sweaty.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
2. The day after drinking alcohol, my hands shook first thing in the morning.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
3. The day after drinking alcohol, my whole body shook violently first thing in the morning if I didn't
have a drink.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
4. The day after drinking alcohol, I woke up absolutely drenched in sweat.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
5. The day after drinking alcohol, I dread waking up in the morning.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
6. The day after drinking alcohol, I was frightened of meeting people first thing in the morning.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
7. The day after drinking alcohol, I felt at the edge of despair when I awoke.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
8. The day after drinking alcohol, I felt very frightened when I awoke.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
9. The day after drinking alcohol, I liked to have an alcoholic drink in the morning.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
17
10. The day after drinking alcohol, I always gulped my first few alcoholic drinks down as
quickly as possible.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
11. The day after drinking alcohol, I drank more alcohol to get rid of the shakes.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
12. The day after drinking alcohol, I had a very strong craving for a drink when I awoke.
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
13. I drank more than a quarter of a bottle of spirits in a day (OR 1 bottle of wine OR 7
beers).
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
14. I drank more than half a bottle of spirits per day (OR 2 bottles of wine OR 15 beers).
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
15. I drank more than one bottle of spirits per day (OR 4 bottles of wine OR 30 beers).
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
16. I drank more than two bottles of spirits per day (OR 8 bottles of wine OR 60 beers)
ALMOST NEVER
SOMETIMES
OFTEN
NEARLY ALWAYS
Imagine the following situation:
1. You have been completely off drink for a few weeks
2. You then drink very heavily for two days
How would you feel the morning after those two days of drinking?
17. I would start to sweat.
NOT AT ALL
SLIGHTLY
MODERATELY
QUITE A LOT
18. My hands would shake.
NOT AT ALL
SLIGHTLY
MODERATELY
QUITE A LOT
19. My body would shake.
NOT AT ALL
SLIGHTLY
MODERATELY
QUITE A LOT
20. I would be craving for a drink.
NOT AT ALL
SLIGHTLY MODERATELY
QUITE A LOT
SCORE
CHECKED BY:
ALCOHOL DETOX PRESCRIBED: YES/NO
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
18
NOTES ON THE USE OF THE SADQ
The Severity of Alcohol Dependence Questionnaire was developed by the Addiction
Research Unit at the Maudsley Hospital. It is a measure of the severity of
dependence. The AUDIT questionnaire, by contrast, is used to assess whether or not
there is a problem with dependence.
The SADQ questions cover the following aspects of dependency syndrome:
• physical withdrawal symptoms
• affective withdrawal symptoms
• relief drinking
• frequency of alcohol consumption
• speed of onset of withdrawal symptoms.
Scoring
Answers to each question are rated on a four-point scale:
Almost never Sometimes Often
Nearly always -
0
1
2
3
A score of 31 or higher indicates "severe alcohol dependence".
A score of 16 -30 indicates "moderate dependence"
A score of below 16 usually indicates only a mild physical dependency.
A chlordiazepoxide detoxification regime is usually indicated for someone who scores
16 or over.
It is essential to take account of the amount of alcohol that the patient reports drinking prior to
admission as well as the result of the SADQ.
There is no correlation between the SADQ and such parameters as the MCV or GGT.
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
19
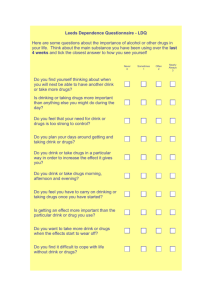
Leeds Dependence Questionnaire - LDQ
Here are some questions about the importance of alcohol or other drugs in your life. Think
about the main substance you have been using over the last 4 weeks and tick the closest
answer to how you see yourself
Never
0
Sometimes
1
Often
2
Nearly
Always
3
Do you find yourself thinking about when you will next
be able to have another drink or take more drugs?
Is drinking or taking drugs more important than
anything else you might do during the day?
Do you feel that your need for drink or drugs is too
strong to control?
Do you plan your days around getting and taking drink
or drugs?
Do you drink or take drugs in a particular way in order
to increase the effect it gives you?
Do you drink or take drugs morning, afternoon and
evening?
Do you feel you have to carry on drinking or taking
drugs once you have started?
Is getting an effect more important than the particular
drink or drug you use?
Do you want to take more drink or drugs when the
effects start to wear off?
Do you find it difficult to cope with life without drink or
drugs?
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
20
Leeds Dependence Questionnaire (LDQ)
The LDQ (www.leedspft.nhs.uk/our_services/leeds_addiction_unit/RESULT) is derived from a
psychological understanding of the nature of dependence and is, therefore, suitable for measuring
dependence during periods of substance use or abstinence. The LDQ is an indicator of how
addicted a person is and, therefore, how difficult it will be to achieve a positive outcome.
For help seeking populations the LDQ is a reasonable proxy for substance use, however, for
people who are socially quite stable, employed and having functional families, heavy drinking or
other drug use is less well correlated with dependence.
There are 10 items scored 0-3.
Cut offs are:
<10 = low dependence;
10-22 = medium dependence; and
>22 = high dependence.
Straus Bacon Social Stability Index
On this 4-point scale, subjects receive 1 point for the presence (yes) of each of the following
criteria:
1. Stable employment over the past 3 years
Yes
No
Yes
No
Yes
No
Yes
No
2. Stable residence for the past 2 years
3. Current residence with at least 1 other individual (not currently living alone)
4. Current marital (or cohabiting) relationship.
DRAFT – for use in Alcohol Treatment PbR Pilot Programme
21