Advanced Paediatric Nurse Practitioner (APNP) Competencies
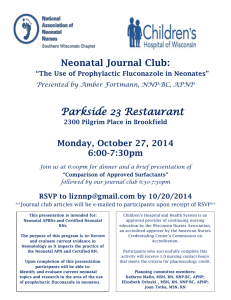
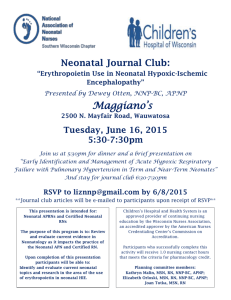
advertisement

ADVANCED PAEDIATRIC NURSE PRACTITIONER (APNP) COMPETENCIES (Barnes, 2004)1 (Adapted from the National Organisation of Nurse Practitioner Faculties, USA2, 3) DOMAIN 1: Health Promotion, Health Protection, Disease Prevention and Illness Management The APNP, as provider of direct health care services, synthesises theoretical, scientific and contemporary clinical knowledge for the assessment, diagnosis and management of health and illness states among infants, children and adolescents. These competencies incorporate the health promotion, health protection, disease prevention and illness management components of APNP practice. Section A: Assessment of health status A1. Obtains, analyses and documents a relevant history (comprehensive and/or problem-focused). A2. Performs and interprets age-appropriate screenings for health, developmental and behavioural concerns (i.e. speech/language development, learning disabilities, and behavioural/mental health issues, etc). A3. Assesses and interprets the child/young person’s health and developmental status, recognising individual differences in temperament, reactions to selected developmental tasks/situational crises, and coping styles/strategies. A4. Identifies and analyses factors that affect the child’s health, growth and/or development. For example: genetic background, prenatal factors, temperament, family and cultural influences, parenting style, and environmental milieu (e.g. nursery, school, living situation, etc.). A5. Adapts, performs and interprets history and screening procedures according to the child’s developmental age, behaviour and reason for health care contact/consultation. A6. Performs, analyses and records a complete, accurate and systematic paediatric physical assessment (comprehensive and/or problem-focused). A7. Recognises and analyses variations of normal including genetic, ethnic, physiologic, anatomic and developmental differences. A8. Assesses for evidence of child abuse/neglect and the effects of violence on the child. This includes identifying and analysing situations and conditions of the child, family, school and community that put the child at risk for abuse/neglect; identifying and interpreting behavioural signs in the child that are associated with abuse/neglect; and differentiating normal physical findings or health practices from those findings of child abuse/neglect. A9. Assesses and analyses the family system to identify factors that influence the health of the child (including parent occupation/education; family support systems; family dynamics and development; family values and beliefs; family management style, stressors and social morbidities such as poverty and illiteracy; management of and coping with acute/chronic illness, etc.). A10. Assesses and analyses the child or young person’s health risks (including developmental level, genetic/family history, immunisation status, nutritional status, risk taking behaviours, environmental factors, family issues, social supports, etc.). A11. Assesses and analyses the child and young person’s knowledge and behaviour with regard to leading health indicators (including: physical activity, eating disorders, tobacco use, substance use and misuse, responsible sexual behaviour, mental health, injury and violence, environment, immunisations and access to health care, etc.). Section B: Diagnosis of health status B1. Differentiates between normal and abnormal development over time, in relation to anatomical, physiological, motor, cognitive, psychological findings and/or the social behaviour of the child. B2. Identifies and synthesises the aetiology, natural history, developmental considerations, pathogenesis and clinical manifestations of disease processes (in addition to the history, physical and diagnostic information) from children and young people to develop and prioritise appropriate differential diagnoses and/or problem lists. B3. Diagnoses and prioritises nutritional conditions and behavioural feeding issues. B4. Orders, interprets and monitors age and situation appropriate screening, laboratory, and other diagnostic tests (including FBC, urinalysis, ova and parasite, X-rays, urine culture, etc.). B5. Collaborates in the diagnosis of children and young people with special health needs and disabilities (using appropriate terminology, format and technology). B6. Seeks consultation, advice and referral appropriately from the multidisciplinary team (using appropriate terminology, format and technology). Section C: Plan of care and implementation of treatment C1. Promotes healthy nutritional practices including promotion and management of breast-feeding, national nutrition guidelines, and healthy nutritional intake considering food preferences, cultural practices and food sensitivities. v4 APNP competencies 1 January 2006 Katie Barnes C2. Provides interventions to modify behaviour associated with health risks such as tobacco, substance use/misuse, lack of physical activity, nutritional patterns, sexual activity and violence. C3. Refers children and young people with developmental disabilities and chronic illness to appropriate community services, family support, and specialty care as needed (using appropriate terminology, format and technology). C4. Incorporates health objectives into individual education plans for children and young people with special needs. C5. Formulates a prioritised action plan, implements interventions (that facilitate the child and young person’s developmental potential) and monitors actions to assist the parent/child in coping with complex, chronic, acute, primary care and/or emergency conditions and behaviours. C6. Prioritises and manages acute, chronic, emergency and/or primary care paediatric illness/conditions, injuries and behavioural problems in children over time (including follow-up) and demonstrates critical thinking and diagnostic reasoning skills in clinical decision-making. C7. Performs a variety of acute, emergency and/or primary care interventions/procedures (e.g. suturing, splinting, smear tests, phlebotomy, cannulation and culturing) that are based on scientific rationale, evidenced-based standards of care and/or practice guidelines. C8. Develops, implements and evaluates health maintenance and health promotion services for the child/family by incorporating teaching, counselling, anticipatory guidance and parental support into paediatric nurse practitioner (APNP) care provision. C9. Develops, implements and evaluates health interventions over time (including non-drug-based treatments, counselling and supportive strategies) that are intrinsic to APNP care provision (e.g. CAMHS interventions, drug regimes, response to iron therapy, etc.). C10. Activates and/or manages child protection services (including follow-up) and other resources on behalf of children at risk. C11. Prescribes (if legally authorised) and/or integrates appropriate drugs and other therapies into the management plan (including non-drug-based therapies) recognising the impact of pharmacodynamics, pharmacokinetics, interaction potential, safety, cost implications and the effects of drug selection and dosing regimens on children. C12. Collaborates in the transition planning for adult health care services. C13. Conducts, utilises and/or applies child-centred, evidence base practice that contributes to positive change in paediatric health care delivery and includes attention to the safety, cost, invasiveness, simplicity and acceptability of interventions to children, young people and their families. C14. Seeks consultation, advice and referral appropriately from the multidisciplinary team (using appropriate terminology, format and technology). DOMAIN 2: Relationships Between Child/Young Person (CYP)/Family and APNP Clinician Competencies in this area demonstrate the collaborative, collegial, and personal approach that enhances the APNP’s effectiveness and quality of care for children, young people and their families. The competencies address the critical importance of interpersonal interactions as they relate to therapeutic outcomes for children, young people and their families. Section D: Relationships between child/young person(CYP)/family and clinician D1. Creates a climate of mutual trust and establishes partnerships with children and families that: verifies/validates findings; acknowledges their strengths; and assists them in addressing their health and social care needs. D2. Evaluates and adapts the relationship between the APNP and the CYP/family to the changing nature of the child’s cognitive, physical and psychosocial development (including the termination of the therapeutic relationship when necessary) through: reflecting and monitoring own emotional response to the relationship; providing a safe transition to another care provider; and using this understanding to further own therapeutic interactions. D3. Communicates effectively (including a sense of ‘being there’) with children and young people of all developmental levels in addition to evaluating the impact of development on health and illness, and/or, the impact of health and illness on development. D4. Communicates effectively with family members, including multi-generational family members. D5. Maintains confidentiality while communicating information, plans of care and results in a manner that preserves the dignity and privacy of the child and young person and provides a legal record of care. D6. Considers the unique needs of children and young people in care with regard to their autonomy in health care access and management by: applying (developmentally appropriate) principles of empowerment; preserving the (developmentally appropriate) control of the CYP; negotiating a mutually acceptable (and developmentally appropriate) plan of care; and fostering (developmentally appropriate) personal responsibility for health. v4 APNP competencies 2 January 2006 Katie Barnes DOMAIN 3: Teaching and Coaching Function These competencies describe the APNP’s ability to impart knowledge, self-care skills and associated psychomotor abilities to children, young people (CYP) and their families. The competencies involve the skills of interpreting and individualising therapies through the activities of modelling, tutoring, support and advocacy. Section E: Teaching and Coaching E1. Assesses the child, young person and family’s motivation for learning in addition to their on-going and changing needs for teaching based on: their growth and developmental stage; the specific skills requisite for care management; and their understanding of the health issue(s). E2. Provides anticipatory guidance and assists learning with an age and/or developmentally appropriate learning plan that considers the principles and stages of learning and behaviour change (in an environment that is conducive to learning). E3. Assists and supports effective parenting skills (and other health advice) using a child-centred evidence-base which includes (when appropriate) the use of community resources. E4. Assists the child and young person in assuming responsibilities for self-care and healthy behaviours in accordance with their age and developmental readiness. E5. Negotiates a plan of care that is mutually acceptable to the child, young person and family that is based on a continual assessment of their readiness and motivation and includes the re-setting of goals and optimal outcomes as necessary. E6. Monitors behaviours and specific outcomes as a useful guide to evaluating the effectiveness and need to change or maintain teaching/coaching strategies. E7. Coaches the child, young person and family through the application of modelling, tutoring, supporting, encouraging, empathising and advocacy behaviours. E8. Elicits from the child, young person and family their (respective): teaching and learning needs (including barriers, supports and modifiers of learning), learning styles; and cultural influences that may impact their learning experience(s). DOMAIN 4: Professional Role These competencies describe the varied role of the APNP as it specifically relates to advancing the profession, enhancing direct care and improving management. The APNP demonstrates a commitment to the development, implementation and evolution of the APNP role. In addition, the APNP develops leadership skills and builds the collaborative and interdisciplinary relationships that are required for the provision of optimal care to children and their families. Section F: Develops and implements the APNP role F1. Interprets and markets the APNP role to the public, legislators, policy-makers, and other health care professionals. F2. Uses scientific theories and research to develop and implement the APNP role. F3. Functions in a variety of role dimensions as necessary (including health care provider, co-ordinator, consultant, educator, coach, team-builder, advocate, administrator, researcher and leader). Section G: Directs care G1. Prioritises, co-ordinates and meets multiple needs for culturally diverse children, young people and their families. G2. Uses sound judgement in assessing conflicting priorities and needs. G3. Obtains specialist advice, consultation and referral for children as required (from other health, social care and/or education professionals; and/or public/independent agencies). G4. Acts as an advocate for the child, young person and family to ensure health needs are met. G5. Incorporates current technology appropriately in care delivery. G6. Uses information systems and technology to support decision-making and to improve care. Section H: Provides leadership H1. Participates in a professional organisation that influences the health of children and supports the role of APNP. H2. Serves as a resource in the design, development and evaluation of paediatric community-based health services and child health policy. v4 APNP competencies 3 January 2006 Katie Barnes H3. Participates in legislative, policy-making and community activities that influence advanced nursing practice and the health of children, young people and their families and communities. H4. Advocates for access to appropriate and quality health care for children and young people. H5. Evaluates the relationship between acute/community/public health issues and social problems as they impact on the health of children, young people and their families (e.g. poverty, violence, illiteracy). DOMAIN 5: Managing and Negotiating Health Care Delivery These competencies describe the APNP’s ability to achieve improved health outcomes for children, young people and their families by overseeing and directing the delivery of clinical services within an integrated system of health care. Section I: Managing health care delivery I1. Maintains current knowledge about the organisation and financing of care for children and young people within the larger health system, including local and regional referral sites. I2. Participates in (and/or) manages organisational decision-making with regard to child health, interprets variations in outcomes and uses data from information systems to improve practice. I3. Demonstrates knowledge of the APNP role and relevant regulations for advanced paediatric nursing practice (including the NMC Code of Professional Conduct and other applicable legislation). I4. Provides care for children, young people, their families, and communities within an integrated system of health care services and considers issues of access, cost, efficacy and quality in care management and decision-making. I5. Demonstrates knowledge of business management strategies and principles (e.g. efficient use of resource, provision of quality care, etc.) that affect the long-term financial viability of a practice and therefore the provision of services to children, young people and their families. Section J: Negotiating health care delivery J1. Collaboratively assesses, plans, implements and evaluates care in conjunction with other health and social care professionals. J2. Participates as a key member of the multidisciplinary team through the development of collaborative and innovative practices. J3. Advocates for policies that reduce environmental health risks, address cultural sensitivity issues and increase access to health care for children, young people and their families. DOMAIN 6: Monitoring and Ensuring the Quality of Health Care Practice These competencies describe the APNP’s role in ensuring quality of care through consultation, collaboration, continuing professional development and evaluation of care. The monitoring function addresses the issues of clinical governance and clinical supervision. Section K: Ensuring quality of health care practice K1. Interprets own professional strengths, role and scope of practice to children, young people, families and colleagues. K2. Incorporates professional and legal standards into practice. K3. Acts ethically to meet the needs of children, young people and their families. K4. Monitors public issues that impact on the delivery of health care services for children, young people and their families. K5. Assumes accountability for own practice and strives to attain the highest standards of practice. K6. Engages in clinical supervision and self reflection to improve care and practice for children, young people and their families. K7. Collaborates and consults with other member of the multi-disciplinary team with regard to care management and health outcomes. K8. Uses an evidence-based approach to the management of child health and illness (including critical enquiry, evaluation and application of research) that is relevant to the management of children, young people and their families. K9. Evaluates the child and young person’s response to care and the effectiveness of care provided. K10. Uses the outcomes of care to revise subsequent management plans and improve the quality of care provided. v4 APNP competencies 4 January 2006 Katie Barnes K11. Accepts personal responsibility for continuing professional development and the maintenance of professional competence and credentials. Section L: Monitoring quality of health care practice L1. Monitors the quality of own practice and participates in continuous quality improvements that include the evaluation of patient follow-up, outcomes, consultations and referrals. L2. Monitors current research and policy guidance in order to improve quality of care. DOMAIN 7: Cultural and Diversity These competencies describe the APNP’s role in providing culturally competent care. More specifically, delivering care to children, young people and their families with respect to cultural and spiritual beliefs including the accessibility of quality health care resources within a dominant culture. Section M: Culture and diversity M1. Recognises the influence of cultural variations and spiritual beliefs on child health practices (including child rearing, nutrition, and family dynamics) and incorporates these into a culturally sensitive plan of care. M2. Shows respect to the inherent dignity of every child, young person and family member irrespective of their age, gender, race, religion, socio-economic class, sexual orientation, ethnicity, spiritual beliefs or cultural group. Assists them in accessing quality care within a dominant culture. M3. Acknowledges own personal biases and prevents these from interfering with the delivery of quality care to children, young people and families from other cultures and/or races. M4. Develops and/or accesses child, young people and family appropriate educational materials (and other resources) that address their language, spiritual and cultural beliefs (thereby assisting them to access care within a dominant culture). M5. Accepts the rights of children, young people and families to choose their care provider, participate in care and refuse care (as developmentally appropriate), including the provision of appropriate information and opportunity to discuss their wishes for end-of-life decisions and care. References Competencies adapted by Katie Barnes as part of work commissioned by the RCN Children’s and Young People’s Field of Practice. 1 National Organisation of Nurse Practitioner Faculties. (2000). Domains and competencies of nurse practitioner practice. Newly revised. Washington, DC: Author. 2 National Organisation of Nurse Practitioner Faculties. (2002). Nurse practitioner Primary Care Competencies in Specialty Areas: adult, family, gerontological, paediatrics and women’s health. Washington, DC: Author. 3 v4 APNP competencies 5 January 2006 Katie Barnes