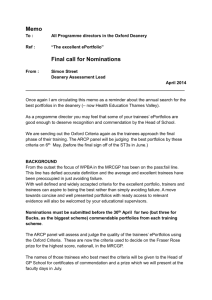
OXFORD DEANERY SPECIALTY TRAINING PROGRAMME IN
advertisement

OXFORD DEANERY SPECIALTY TRAINING PROGRAMME IN INTENSIVE CARE MEDICINE About Oxford Deanery The Oxford Deanery covers the counties of Oxfordshire, Berkshire and Buckinghamshire, with Banbury and Milton Keynes in the North, to Reading and Slough in Berkshire and High Wycombe and Aylesbury in the West. The Oxford Deanery is part of NHS South of England which comprises South Central, South West and South East Coast Strategic Health Authorities. The Oxford Deanery is responsible for the training of some 1500 trainees. The Oxford Deanery is a relatively small deanery with a defined geographical area which serves as a single unit of application. In the majority of cases successful candidates will be asked to preference their choice of location for either one or two years. Some programmes will require successful candidates to indicate a location and specialty. Future placements will usually be based on individual training and educational needs. Please note that applications are to the Oxford Deanery as a whole. This may mean that you may be allocated to any geographic location within the Oxford Deanery depending on training needs. Currently hospitals involved in the ICM programme are The Oxford hospitals group and the Royal Berkshire Hospital in Reading. The Intensive Care Medicine Training Programme The Intensive Care Medicine training programme is a five year programme, starting at ST3. During this time, the trainee's work will be monitored for satisfactory progress and subject to annual reviews in the form of ARCPs. Progression on the programme will be dependent upon these reviews. The posts on this rotation have been approved for Specialist Training by the Faculty for Intensive Care Medicine. The posts attract National Training Numbers and provide training towards a Certificate of Completion of Training. The Postgraduate Dean has confirmed that this post has the necessary educational and staffing approvals. The programme is based currently at the Oxford University Hospitals Trust and the Royal Berkshire hospital Trust. The other Trusts in the deanery are listed below and with time the programme may expand to these other hospitals. Trainees may find themselves employed by any of the following Trusts and placed in any of the following hospitals. Specialist training such as ECMO or liver may occur at other hospitals if this is deemed necessary. Trust Oxford University Hospitals Trust Hospitals and Locations Adult Intensive Care Unit, John Radcliffe Hospital, Oxford http://www.ouh.nhs.uk/ Adult Intensive Care Unit, Churchill Hospital, Oxford http://www.ouh.nhs.uk/ Neurosciences Critical Care Unit, Oxford Radcliffe Hospitals, Oxford http://www.ouh.nhs.uk/ Cardiothoracic Critical Care Unit, Oxford Radcliffe Hospitals, Oxford http://www.ouh.nhs.uk/ Paediatric Critical Care Unit, Oxford Radcliffe Hospitals, Oxford http://www.sort.nhs.uk/home.aspx Milton Keynes Hospital Trust Heatherwood and Wexham Park Hospitals Trust Milton Keynes Hospital, Milton Keynes Royal Berkshire Hospital Trust Royal Berkshire Hospital, Reading Buckingham Hospitals Trust Wycombe General Hospital, High Wycombe http://www.mkgeneral.nhs.uk/ Wexham Park Hospital, Slough http://www.heatherwoodandwexham.nhs.uk/location/wexhampark-hospital-slough http://www.royalberkshire.nhs.uk/ http://www.buckshealthcare.nhs.uk/ Stoke Mandeville Hospital http://www.buckshealthcare.nhs.uk/ Rotation Information The expected rotation arrangements for this programme are: ST3 12 months in the two Adult Intensive Care Units in the teaching hospital (Oxford University Hospitals Trust). It is during this time that we would expect you to complete your Stage 1 competencies. In Oxford all trainees will be FICE trained in this year, a unique opportunity to develop early echo skills. ST4 12 months in acute medicine/anaesthesia training as required. It is likely that this will be in one of the district general hospitals in view of the case mix and clinical support experience available. ST5 Four months each in regional specialist ICUs (Neurosciences, Cardio-thoracic and Paediatric ICU at the John Radcliffe Hospital. The PICU may involve time at Southampton PICU too). ST6 12 months ICM with special skill training. The likely available options would be echocardiography training or simulation / medical education training. Please see below for further details. It is during this Stage 2 training that the final FFICM must be taken. Teaching will be adapted to ensure high exam success rates. With the previous ICM DICM pass rates were > 95%. ST7 12 months advanced ICM training in the Adult Intensive Care Units (Oxford University Hospitals Trust), with up to 6 months in another General Adult ICU in the region. This will compete Stage 3 training and ensure you are able to function as a consultant Intensivist. Rotations may at times change in response to clinical need from the Trusts and training requirements. Training Centre Information Adult Intensive Care Unit (AICU) and Churchill Intensive Care Unit (CICU) These two general Intensive Care Units admit over 1000 patients per year. The majority of patients are level 3. Approximately 20% of admissions are elective surgical patients and the remainder critically ill emergency patients with a wide range of medical and surgical pathologies. Oxford is the tertiary referral centre for major trauma, spinal, interventional cardiology, oesophageal, vascular, major maxillo-facial surgery, interventional radiology, haematological malignancy and transplantation (including bowel and pancreas). This is reflected in the pathology of patients on the AICU/CICU. The Standardised Mortality Ratio is significantly below the national average. A full range of invasive monitoring and all major forms of organ support are employed. The majority of patients require multi-organ support and invasive monitoring. Trainees can expect to gain experience of oesophageal Doppler monitoring, thrombo-elastography, renal replacement techniques, echocardiography, bronchoscopy, ultrasound, invasive and non-invasive ventilation as well as more basic procedures such as line placement and resuscitation. The units are medically staffed in multiple groups: three groups of trainees (from both an anaesthetic and non-anaesthetic background) and the consultant tier. The presence of trainees from a variety of backgrounds provides a fantastic training environment and so represents a rare opportunity given the UK system of early specialisation. It is particularly useful for those trainees doing professional exams and helps our high success rate in the FRCA final/DICM and EDIC. The twelve consultants cover each unit separately on a split week system. The consultants come from a background in anaesthesia, medicine, military services and research. There is local expertise in clinical trials research, bench research, sepsis and genomics, ventilation, difficult airways, teacher training, simulation, international transfer, primary trauma in developing countries, resuscitation, follow up, ultrasound and echocardiography. The unit has an active teaching programme. This includes protected teaching, weekly unit meetings, daily microbiology rounds and various yearly meetings. The senior trainees have an active exam orientated program in addition to one half-day per month of protected teaching. This contributes to the high success rate in the Diploma. There is a very strong trainee drive for training in the Oxford region. There are monthly OXDAT meetings www.oxdat.co.uk which is a forum to advance ideas and ensure high standards of training in all hospitals within the rotation. The Neurosciences Intensive Care Unit The Oxford Neuroscience Unit is one of the busiest regional neurosurgical units in the country with an international reputation for the quality of its services. It is involved in many aspects of pioneering work including functional neurosurgery and radiological interventional techniques. The busy unit will provide trainees with unrivalled exposure to all aspects of neurosurgical work. The Oxford Neurosciences Unit moved to a new purposebuilt modern facility in the West Wing of the John Radcliffe Hospital in January 2007. The Neurosciences Intensive Care Unit provides level 2 and level 3 specialist critical care to both neurosurgical and neurological patients from the region. The Unit currently contains 11 level 3 critical care beds, with planned expansion over the next few years to a 17 bed unit. Training is provided in the management of the full range of neurosurgical and neurological pathologies, with particular emphasis on the management of traumatic brain injury and subarachnoid haemorrhage. Cardiothoracic Critical Care Unit The John Radcliffe Hospital is a tertiary referral centre for cardiac and thoracic disease. The Cardiothoracic Critical Care (CTCC) is an 11 bedded unit supporting an annual caseload of approximately 950 adult cardiac cases of which 65% represent patients undergoing coronary bypass grafting, 20% valve repair or replacement and 15% combined or complex procedures. About 100-200 thoracic cases are performed each year. There is local expertise and training in trans-oesophageal echocardiography. In addition there is close work with the interventional cardiac laboratory where a 24 hour PCI is run. The Paediatric Intensive Care Unit The tertiary Paediatric Intensive care Unit serves the Oxfordshire population and supports a wide range of both surgical and medical paediatric specialties in all the Oxford hospitals. Elective surgical specialties include general and urological surgery, orthopaedics, craniofacial, plastics, neurosurgery, ENT, dental and ophthalmology whilst the medical specialities include oncology, radiology (including MRI), radiotherapy, gastroenterology and cardiology. There were 350 admission last year and the unit has been merged with Southampton to form the SORT service and critical services for South Central. www.sort.nhs.uk Southampton admit about 1000 cases per year and manage the regional transport service. The biggest part of PICU is probably the stabilisation of the sick child in a DGH who then get’s retrieved. There is scope to obtain training in retrieval of these children. The Royal Berkshire Hospital Intensive Care Unit This ICU has 11 beds and there is an 8 bedded HDU opening in April 2013. Currently there are 750 admissions per year but this will increased to 1200 with the surgical HDU. The 8 consultants work a weekly rota incorporating a second consultant for extra supervision and teaching. There are 2 advanced/senior ICM trainees doing a traditional oncall rota and 8 trainees on a 1 in 8 full shift rota. There is a weekly journal club and radiology sessions which are particularly well evaluated. The unit has a progressive approach to educational supervision. The unit is fully computerised with the Philips clinical information system. In addition to standard pathologies, patients are treated after major urological, vascular and oesophageal surgery and spinal trauma. Level two paediatric patients are also supported. Trainees can expect exposure to a variety of advanced monitoring and therapeutic procedures. Examples include percutaneous tracheostomy (100 per year), ultrasound, ODM, echocardiography, bronchoscopy, PICCO and intracranial pressure monitoring (inserted by the ICU staff). Audit and research are encouraged and supported by a powerful clinical information system, research nurses and a data manager. The research team are the leading recruiters to many national trials. Reading also has expertise beyond the traditional boundaries of Intensive Care. The follow-up clinic is the second oldest in the UK and there is a 24/7 outreach service which sees 8000 patients per year. A centrally funded bereavement expert co-ordinates relative follow-up, organ donation and staff pastoral care. Buckinghamshire Intensive Care Units These 2 expanding ICUs have 16-20 beds with input from 15 consultants. In addition to the usual DGH specialties, the unit is the regional centre for acute spinal injury and major burns. This provides exposure to these highly specialised areas of the Intensive Care syllabus including free flap reconstructive surgery, weaning and rehabilitation of acute spinal injury and burns patients. In addition to routine procedures, percutaneous tracheostomy and Doppler flow monitoring are performed on the ICU. Wexham Park Intensive Care Unit This unit has recently been rebuilt into a state of the art general ICU with 12 level 2 and level 3 beds. Nine consultants contribute to dedicated 24 hour cover and lead three ward rounds per day. The midday round is actively supported by specialist pathology / microbiology, pharmacy, clinical biochemistry and respective surgical specialties. There is a very busy outreach service which provides trainees an insight into flagging up potential ICU admissions and their management in the wards. An ICU follow up clinic is well established. Research & audit is greatly encouraged and actively taken up by most trainees. A weekly formal teaching programme is conducted within the department and all trainees have a protected half day for this activity. Practical procedures training is provided in routine ICU procedures such as lines, haemofiltration etc. Specialist procedures include percutaneous tracheostomy (about 50/yr), intra-cranial pressure transducer placement & monitoring, oesophageal Doppler and PiCCO cardiac output monitoring. Milton Keynes Intensive Care Unit This unit runs flexibly up to a maximum of nine level 2/3 patients. There is dedicated daytime consultant sessional commitment. Specialist procedures performed routinely on the unit include percutaneous tracheostomy (about 50/yr), oesophageal Doppler cardiac output monitoring, Bi-Spectral Index monitoring and fibre-optic guided airway training. Training information The Oxford region has a strong tradition of training excellent which was reflected in the 2011 GMC training survey ranking of the program as the highest in the country for overall satisfaction. All joint CCT trainees have secured consultant post in ICM at the end of their training and the DICM pass rate is over 95%. The training environment is continually monitored using the PHEEM questionnaire and all training centres offer active teaching programs and host regional meetings. The programme offers an outstanding range of training opportunities. In addition to attachments to standard specialist units the region has a tradition of offering extra short attachments to related specialities. Popular attachments have included microbiology, radiology and hepato-biliary ICM and there is currently a fully funded travel bursary to Hong Kong awarded yearly to an Intensive Care trainee in the region. The ST6 year represents a particularly interesting opportunity for the ICM trainee to develop expertise in an area related to Intensive Care. At this early stage of curriculum development the intention is to adapt 2 existing and successful ICM posts in the region that currently offer Echocardiography and Simulation training. The echocardiography training post combines ICM-specific trans-thoracic echocardiography with further advanced ICM experience. The post provides comprehensive training from both ICM and cardiology trainers, taking the novice up to British Society of Echocardiography standard. The successful program has run for several years and a report was published recently (JICS 11:1 2010). The fellowship represents an opportunity to develop a sought-after clinical skill with applications in any ICU. The medical education post offers a subsidiary interest in Simulation training. The training rota includes protected time for work with OxStar, the state of the art “Simulation Centre” based at the John Radcliffe Hospital. The successful candidate develops expertise in simulation, leads simulation training on the Intensive Care units, undertakes a higher level formal teaching qualification and can take up research opportunities as offered by the OxStar centre. The post has the potential to provide a thorough grounding for a trainee with an interest in teaching and training. Duties of Post The appointee will be responsible for the day-to-day running of the unit, including the management of individual patients, management of bed availability, and supervision of junior staff. Further responsibilities are rotated between trainees: Significant self directed study is expected. An appointee will be responsible for organising and running the regular teaching sessions. This will include arranging speakers, and ensuring the programme is advertised in a timely fashion. The appointee will be expected to undertake some work with a view to producing published results. As an alternative to a research/review project the appointee may wish to consider undertaking an audit, retrospective or prospective, of patients on the Intensive Care Unit. It is expected that the audit will be of a sufficient standard to be published or presented at national meetings. There is an expectation the appointee will assist with any contract research undertaken on the Intensive Care Units. It is expected the appointee will attend at least one national meeting on Intensive Care during their appointment. This will be funded in the usual way from the study leave budget. The appointee will assist in teaching of the more junior trainees and medical students on attachment to the Intensive Care Unit. The appointee will be expected to attend, as an observer, some of the management meetings of the Critical Care Centre and Intensive Care Unit and take an active role in the practical running and development of the unit. This may include managing the junior and senior trainee rota. The appointee will be expected to complete Competency Based Assessment documentation as outlined by the GMC/FICM. There is a full shift resident commitment with internal leave cover. The progress of the appointee will be continually monitored by the Consultant staff. This will include regular appraisal. The appointee will also receive regular assessment covering skill, knowledge and attitudes and any other relevant areas. The appointee will work towards sitting a higher exam(s) in Intensive Care in the course of training. Main Conditions of Service Appointments to this programme are subject to the Terms and Conditions of Service (TCS) for Hospital Medical and Dental Staff (England and Wales). In addition appointments are subject to: Applicants having the right to work and be a doctor or dentist in training in the UK Registration with the General Medical Council Pre-employment checks carried out by the Trust HR department in line with the NHS employment check standards, including CRB checks and occupational health clearance. The employing Trust’s offer of employment is expected to be on the following nationally agreed terms: Hours – The working hours for junior doctors in training are now 48-hours (or 52-hours if working on a derogated rota) averaged over 26 weeks (six months). Doctors in training also have an individual right to opt-out if they choose to do so, but they cannot opt-out of rest break or leave requirements. However, the contracts for doctors in training make clear that overall hours must not exceed 56 hours in a week (New Deal Contract requirements) across all their employments and any locum work they do. http://www.nhsemployers.org/PlanningYourWorkforce/MedicalWorkforce/EWTD/Pag es/EWTD.aspx Pay – you should be paid monthly at the rates set out in the national terms and conditions of service for hospital medical and dental staff and doctors in public health medicine and the community health service (England and Wales), “the TCS”, as amended from time to time. The payscales are reviewed annually. Current rates of pay may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircularsMedi calandDental.aspx Part time posts will be paid pro-rata Pay supplement –depending upon the working pattern and hours of duty you are contracted to undertake by the employer you should be paid a monthly additional pay supplement at the rates set out in paragraph 22 of the TCS. The current payscales may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircularsMedi calandDental.aspx . The pay supplement is not reckonable for NHS pension purposes. The pay supplement will be determined by the employer and should be made clear in their offer of employment and subject to monitoring. Pension – you will be entitled to join or continue as a member of the NHS Pension Scheme, subject to its terms and rules, which may be amended from time to time. If you leave the programme for out of programme experience you may have a gap in your pension contributions. More information can be found at http://www.nhsbsa.nhs.uk/pensions Annual Leave – your entitlement to annual leave will be five or six weeks per annum depending on your previous service/incremental point, as set out in paragraphs 205-206 of the TCS. The TCS may be viewed at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTSGPR EG/Pages/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx Sick pay – entitlements are outlined in paragraph 225 of the TCS. Notice –you will be required to give your employer and entitled to receive from them notice in accordance with paragraphs 195-196 of the TCS. Study Leave –the employer is expected to offer study leave in accordance with paragraphs 250-254 of the TCS. Local policy and procedure will be explained at induction. Travel Expenses – the employer is expected to offer travel expenses in accordance with paragraphs 277-308 of the TCS for journeys incurred in performing your duties. Local policy and procedure should be explained at induction. Subsistence expenses – the employer is expected to offer subsistence expenses in accordance with paragraph 311 of the TCS. Local policy and procedure should be explained at induction. Relocation expenses – the employer will have a local policy for relocation expenses based on paragraphs 314 – 315 of the TCS and national guidance at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTSGPR EG/Pages/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx. You are advised to check eligibility and confirm any entitlement with the employer before incurring any expenditure. Pre-employment checks – all NHS employers are required to undertake pre-employment checks. The employer will confirm their local arrangements, which are expected to be in line with national guidance at http://www.nhsemployers.org/RecruitmentAndRetention/Employmentchecks/Pages/Employment-checks.aspx Professional registration – it will be a requirement of employment that you have professional registration with the GMC/GDC for the duration of your employment. Though the post is covered by NHS Indemnity, you are strongly advised to register with the MPS for professional indemnity. Health and Safety – all employers have a duty to protect their workers from harm. You should be advised by the employer of local policies and procedures intended to protect your health and safety and expected to comply with these. Disciplinary and grievance procedures – the employer will have local policies and procedures for dealing with any disciplinary concerns or grievances you may have. They should advise you how to access these, not later than eight weeks after commencement of employment. Educational Supervisor – the employer or a nominated deputy (usually the Director of Medical Education) will confirm your supervisor on commencement. General information on the Deanery’s management of Specialty Training programmes, including issues such as taking time out of programme and dealing with concerns or complaints, is available at www.oxforddeanery.nhs.uk and in the national ‘Gold guide’ to Specialty Training at http://www.mmc.nhs.uk Please ensure that you inform Oxford Deanery of any changes to your contact details. December 2012