prognostic relevance of specific chromosomal abnormalities in

PROGNOSTIC RELEVANCE OF SPECIFIC CHROMOSOMAL ABNORMALITIES IN
CHRONIC MYELOMONOCYTIC LEUKEMIA
Such E, Cervera J, Costa D, Solé F, Luño E, Nomdedeu B, Vallespí T, Carbonell F, Ardanaz
MT, Ramos F, Tormo M, del Cañizo C, Mallo M, Xicoy B, Gomez V, Marco V, Bonanad S,
Collado R, Calasanz MJ, CruzCigudosa J, Hernández-Rivas JM, Senent ML, Pedro C, Bernal
T, Bueno J, and Sanz GF.
Spanish Registry of Myelodysplastic Syndromes
Background: Chronic myelomonocytic leukemia (CMML) is a clonal disorder sharing features of both myelodysplastic syndromes (MDS) and chronic myeloproliferative disorders.
Cytogenetics findings have a key role in prognostic stratification in MDS but the prognostic value of karyotype in CMML is unknown.
Aims: To evaluate the prognostic significance of specific chromosomal abnormalities in a large series of patients with CMML from the Spanish Registry of MDS.
Patients and methods : 414 of 564 patients with a diagnosis of de novo CMML according to
FAB and WHO classifications had a successful cytogenetic analysis at diagnosis (73%) and were included in the study. Median age was 73 yr and 287 (69%) were males. 248 patients
(60%) had myelodysplastic CMML (absolute WBC count ≤13 x 10 9 /L) and 166 (40%) had myeloproliferative CMML (absolute WBC count >13 x 10 9 /L) according to FAB criteria.
Morphological subtypes by WHO classification were CMML-1 in 366 (89%) and CMML-2 in 46
(11%).
Results: Karyotype was normal in 304 patients (73%) and abnormal in 110 (27%). The most frequent chromosomal aberrations were +8 (n=30) [either alone (n=24) or with one additional abnormality (n=6)], -Y (n=18), complex abnormalities (>2 abnormalities; n=12), and -7/7q (n=7).
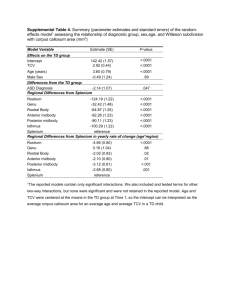
Other miscellaneous abnormalities were evident in 41 patients. With a median follow-up of 33 months, the median overall survival (OS) was 35 months and median time to transformation to acute myeloid leukemia (AML) had not been reached. A new cytogenetic classification with 3 categories (good-risk, normal karyotype or -Y as a single anomaly; poor-risk, trisomy 8 or complex karyotype; and intermediate-risk, all other abnormalities) was better for prognostication than the IPSS cytogenetic classification, even in patients with myelodysplastic CMML. 3-yr OS for patients in the good, intermediate, and poor-risk cytogenetic categories was 55%, 35%, and
19% respectively (P<0.0001). Multivariate analysis confirmed that this cytogenetic risk classification was an independent prognostic variable for OS (P=0.0012), along with absolute
WBC count (≤13 vs. >13, P<0.0001), platelet count (<100 vs. ≥100 x 10 9 /L, P=0.004) and blasts in marrow (≤10% vs. >10%, P<0.0001). Patients belonging to the poor-risk cytogenetic category had a higher risk of AML evolution on univariate analysis (40% vs. 18% for all other patients;
P=0.0015) but the only variable independently associated with evolution to AML on multivariate analysis was the percentage of blasts in marrow (P<0.0001). When RBC transfusion dependency at diagnosis was included in multivariate analyses the variables entering the regression models were RBC transfusion dependency (P<0.0001), absolute WBC count
(P<0.0001), and blasts in marrow (P<0.0001) for OS and transfusion dependency (P<0.0001) for evolution to AML.
Conclusions: The results of this study demonstrate the prognostic impact of conventional cytogenetics in patients with CMML. The proposed new cytogenetic classification was able to segregate patients into 3 risk categories for OS and 2 categories for AML evolution but its real prognostic value needs confirmation in other series. Similarly to other MDS subtypes, the presence of transfusion dependent anemia in CMML confers poorer OS and higher risk of AML evolution.
This study was supported in part by the Instituto de Salud Carlos III grants PI05/1224,
RD06/0020/0031 and CA08/00141.