Emergency Procedures at the Burn Scene
advertisement

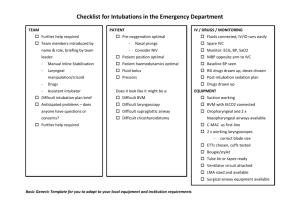
INITIAL ASSESSMENT DETERMINE ON ALL PATIENTS: 1. Age 2. Chief complaint. 3. Previous medical history. 4. Weight 5. Medications 6. Allergies 7. Immunizations 8. Source of routine care. NOTE: 1. Vital signs must be individualized for each patient. 2. Any patient seen at a health care facility earlier and brought back for return visit at the ER is a source of concern. BASIC and ADVANCED LIFE SUPPORT 1. Establish unresponsiveness. a. Gently shake patient. b. Raise your voice to awaken the patient. 2. Call for help. 3. Position patient on a firm flat surface. 4. Open the airway: Head tilt – chin lift method; jaw thrust maneuver if with cervical spine injury. Note: A posteriorly placed tongue is a common cause of airway obstruction. 5. Assess breathing. Look, feel and listen. Observe for chest rise Listen for breath sounds Feel for expired air 6. Establish a seal. a. Infant – apply Mouth to Nose and Mouth. b. Older child – apply Mouth to Mouth; pinch nose 7. Give two slow breaths using enough volume to cause the chest to rise. If chest does not rise – obstructed airway. 8. Begin rescue breathing if breathing is not noted. 9. Assess pulse for cardiac function. a. Infants < 1 year – use brachial or femoral arteries. b. Older children – carotid artery 10. Begin chest compression if no pulse present. a. Infant <1 year – compress one finger width below the imaginary line between the nipples on the sternum b. Older children and adolescents – compress over the lower half of the sternum 11. Coordinate compression and breathing – 5:1 compression/ventilation ratio. 12. Airway obstruction a. Infants < 1 year – i. Do five back blows with the child straddled over the rescuer’s arm. ii. Then do five chest thrusts at the location described for chest compression. iii. Repeat sequence until relieved. b. Older children – Perform Heimlich maneuver or abdominal thrust. Repeat until obstruction is relieved. Note: Endotracheal intubation – best way to manage the airway during CPR. ETT size = width of the 5th finger or diameter of the nares. = 4 plus (Patient’s age) / 4 13. Fluid Administration Isotonic crystalloid – plain lactated Ringer’s solution or plain NSS o 20 ml/kg 14. Drugs Endotracheal Drug Administration o Epinephrine o Atropine o Lidocaine o Naloxone IV Administration o Epinephrine First dose: 0.1 ml/kg (1:10,000) Subsequent doses: 0.1 ml/kg (1:1000) Repeat every 3 – 5 mins o Atropine 0.2 ml/kg 1.0 ml min; 5 ml max for child o Sodium bicarbonate 1 – 2 ml/kg o Naloxone < 5 yrs or < 20 kg – 0.1 mg/kg o Lidocaine 1 mg/kg 15. Defibrillation a. Ventricular fibrillation b. Pulseless ventricular tachycardia c. First dose: 2 J/kg d. Subsequent doses: 4 J/kg 16. Cardioversion a. Tachyarrhythmias with shock b. Dose: 0.5 – 1.0 J/kg SHOCK Definition – occurs when perfusion is inadequate to meet the metabolic demands of the tissues; leads to deterioration of organ function and multiple end-organ failure and death. Type of Shock Hypovolemic: pump is empty Etiology Trauma Dehydration Excessive sweating Diabetes Cardiogenic: Weak pump Dysrhythmias CHF Cardiomyopathy Distributive: Fluid distribution Sepsis Anaphylaxis Spinal cord injury Signs of Shock Early Narrowed pulse pressure Orthostatic hypotension Delayed capillary filling Tachycardia Hyperventilation Late Decreased systolic pressure Decreased diastolic pressure Cold,pale skin Altered mental state Diaphoresis Decreased urine output Management 1. Position – Assume position of comfort 2. 100% Oxygen 3. Assisted ventilation as indicated. 4. IV access – start 2 large bore IV lines 5. Fluids – NSS or Plain LR; 20 ml/kg IV bolus ; may repeat 2 more times if still with decreased BP or poor urine output 6. Inotropes a. Dopamine – 5 – 20 ug/kg/min b. Dobutamine – 5 – 20 ug/kg/min BURNS Diagnostic Findings: Depth: 1. Superficial partial thickness or first-degree burns: epidermis; erythema and local pain 2. Partial thickness or second-degree burns: epidermis and dermis a. Partial thickness – erythema and blisters b. Deep partial thickness – white and dry; have reduced sensitivity to touch and pain; blanch with pressure 3. Full – thickness or third degree burns: skin and deeper layers; numb with a tough, brownish surface Severity: 1. Major burn: a. Burns of the hands, face, eyes, ears, feet or perineum b. Patients with inhalation injury, electrical burns, burns complicated by fractures or other major trauma c. Poor risk patients including those with underlying disease and suspected child abuse d. Partial thickness burns: > 25% BSA (adults); > 20% BSA (children) e. Full thickness burns: > 10% BSA 2. Moderate uncomplicated burn: a. Partial thickness burns: 15 % to 25% BSA adults; 10% to 20% BSA children b. Full thickness burns: 2% to 10% BSA 3. Minor burns: a. Partial thickness burns: <15 % BSA adults; <10% BSA children b. Full thickness burns: <2% BSA Emergency Procedures at the Burn Scene 1. Extinguish the flames. a. “ Drop and roll !” b. Use blanket, rug or coat. c. Disconnect the electrical source. 2. Cool the burn. a. Soak the burned area with cool water. b. Never i. Apply ice directly to the burn. ii. Wrap burn victims in ice. iii. Use cold soaks or dressing for longer than several minutes. 3. Remove restrictive objects. a. If possible, remove clothing immediately. b. Remove all jewelries. 4. Cover the wound. a. Cover burn wound immediately to prevent bacterial contamination. b. Use dry clean cloth. 5. Irrigate Chemical Burns. a. Rinse all areas of the body. b. Rinse eyes with cool clean water At the Emergency Department: 1. Maintain patent airway and adequate airway clearance. a. Provide humidified oxygen. b. Suction secretions as needed. c. Maintain proper patient positioning. d. Assess breath sounds, respiratory rate, rhythm, depth and symmetry. e. Report labored breathing, decreased depth of respiration or signs of hypoxia to physician immediately. f. Prepare for endotracheal intubation. 2. Control pain related to tissue and nerve injury. a. Assess pain level using pain intensity scale. b. Provide emotional support and reassurance. c. Administer analgesics as prescribed. d. Assess response to analgesic. 3. Restore optimal fluid and electrolyte balance. a. Monitor vital signs and urine output at least every hourly until stable. Be alert for signs of hypovolemia or fluid overload. b. Maintain IV lines and regulate fluids at appropriate rates as prescribed. i. Immediately place a large bore IV catheter in either a central or peripheral vein in an unburned area. ii. Administer a bolus of 20 ml/kg NSS or Plain LR. iii. Dopamine 5 – 20 ug /kg/min if poor perfusion persists. c. Be alert for decreasing blood pressure and urine output and increasing pulse rate. 4. Prevent burn complications such as paralytic ileus and Curling’s ulcer. a. Auscultate for bowel sounds and observe for abdominal distention. b. Prepare for NGT insertion and monitor NGT drainage. c. Administer antacids and histamine blockers as prescribed. 5. Prevent wound infection. a. Practice aseptic technique in caring for wounds. b. Clean wounds and change dressings regularly. c. Administer systemic and topical antibiotics. d. Administer tetanus immunization. i. Tetanus toxoid – 0.5 ml IM if last immunization was 5 yrs ago ii. Add tetanus immune globulin 0.5 ml IM if patient received less than 3 tetanus toxoid boosters SEIZURES Febrile Seizure: 1. 2. 3. 4. Presence of fever. Age range: 3 months to 6 years. No more than 15 minutes. Family history of seizures. 5. 6. 7. Generalized tonic-clonic seizures. No neurologic deficit. EEG normal. Management: 1. Maintain patent airway and adequate airway clearance. a. Provide humidified oxygen. b. Suction secretions as needed. c. Prepare to assist with endotracheal intubation. 2. Protect the head from injury. 3. Insert oral airway. 4. Secure an IV line. 5. If febrile, administer tepid sponge bath. 6. Keep side rails up. Never allow patient to be left alone. 7. Administer anticonvulsant and antipyretic medication. a. Diazepam (Valium) 0.1 – 0.3 mg/kg; max 10 mg b. Phenobarbital 20 mg/kg c. Phenytoin 20 mg/kg 8. After the seizure, keep patient in side-lying position to prevent aspiration. FOREIGN BODY IN THE AIRWAY Epidemiology: 1. Any object may be aspirated ! Most common - food and vegetable matter. 2. Round objects -> complete airway obstruction. 3. Highest risk group – birth to 48 months. 4. Peak age group: between 1 and 2 years. Diagnostic Findings: 1. Acute airway obstruction: a. Due to material lodged in the laryngotracheal airway b. Results in acute, life-threatening respiratory distress. c. Cyanosis, apnea, stridor, wheezing, cough and dysphonia. d. Facial petechia. e. Remember: Wheezing, coughing and decreased breath sounds ! 2. Subacute obstruction: a. Due to bronchial foreign bodies and partial obstruction of the LT segment. b. At least one component in the triad is not present. Management: 1. For infants < 12 months: a. Apply 5 back blows to expel or loosen a FB. b. If not expelled, administer 5 manual chest thrusts. 2. For older children: a. Heimlich maneuver – primary technique. Repeat as indicated. b. Open airway by the jaw thrust maneuver. Remove FB if visualized. 3. A combination may be more effective than any single method. HEAD TRAUMA Epidemiology: 1. Head injury due to falls. 2. Primary insult is injury to the brain at the time of impact. 3. Secondary insult is due to progressive deficit caused by increased ICP, cerebral ischemia and hypoxia. 4. Brain swelling most common cause of death. 5. Suspect child abuse in children < 1 year old. History: 1. Mechanism of injury: direct blow or acceleration/deceleration. 2. Circumstances of injury: fall, motor vehicle, blow, etc. 3. Chronology: a. Progression of deficits b. Loss of consciousness immediately or shortly after the injury 4. Associated findings a. Nausea and vomiting b. Headache c. Seizures d. Amnesia e. Disorientation f. Sensorimotor abnormalities g. Visual disturbances Physical Examination 1. Airway. 2. Examine cervical spine and other areas of trauma. 3. Check BP. 1. 2. 3. 4. 5. 6. 4. 5. 6. Cushing’s reflex – Increased BP, slow PR and irregular respiration. Due to increased ICP. Monitor I and O. a. Fluid overload – cerebral edema. b. Diabetes insipidus – increased urine output. Neurologic examination: a. Level of consciousness i. A – awake verbal child ii. V - if unconscious, denotes a child who is responsive to Verbal stimuli i.e. eye opening iii. P – responds to Painful stimuli i.e. moaning or crying iv. U – unresponsive to any stimuli b. Pupils – unilateral pupillary dilatation suggests a mass lesion with impending brain stem herniation. c. Infants – bulging anterior fontanels may suggest increased ICP Specific Brain Injuries 1. Concussion – not demonstrable by radiographic studies; may be associated with transient loss of consciousness. 2. Contussion – area of focal edema with or without bleeding seen on CT scan; with loss of consciousness; may have focal deficits. 3. Epidural hematoma – tear in the middle meningeal artery; concussion followed by a lucid interval then loss of consciousness with signs of increased ICP. 4. Subdural hematoma – tearing of veins between the cortex and the dura; associated with severe brain injury. 5. Basilar skull fracture – fx’s of the base of the skull; hemotympanum, Battle’s sign, CSF otorrhea, facial palsy Criteria for hospitalization: 1. Documented prolonged loss of consciousness (> 5 minutes). 2. Coma, altered mental status or seizure. 3. Focal neurologic deficit. 4. Presence of skull fracture. 5. Persistent vomiting. 6. Severe and persistent headache. 7. Suspicion of child abuse or unreliable caregiver. Who may be sent home for observation? 1. Loss of consciousness < 5 minutes. 2. Normal physical examination. 3. Absence of severe or progressive symptoms of headache or vomiting. 4. Normal skull X-ray study/ CT scan Emergency Management: 1. Airway. a. Oxygenate. b. Suction blood and secretions. c. Remove FB. d. Prepare to assist in endotracheal intubation. 2. Breathing. Assisted ventilation as necessary. 3. Circulatory status. a. Assist in IV insertion – D10 Water. b. Maintain prescribed IV flow rate usually 2/3’s maintenance. c. Monitor BP – to maintain adequate cerebral perfusion and detect shock. d. Monitor I and O. 4. Immobilize cervical spine. 5. Reduction of intracranial pressure. a. Hyperventilate patient – to decrease cerebral blood flow. b. Elevate head of bed to approximately 30 45 degrees. c. Administer diuretics. i. Furosemide (Lasix) ii. Mannitol 0.5 – 1 gm/kg d. Dexamethasone – 0.2 mg/kg 6. Administer anticonvulsants as prescribed. i. Phenobarbital ii. Phenytoin ANAPHYLAXIS Definition: a syndrome involving a rapid and generalized immunologically mediated reaction; occurs after exposure to foreign allergens in previously sensitized individuals Signs and symptoms 1. Respiratory system a. Upper – stridor, hoarseness, angioedema of the tongue, lips and uvula, nasal discharge or obstruction b. Lower – wheezing, chest tightness 2. Cardiovascular system a. Dizziness, syncope b. Hypotension c. Chest pain d. dysrhythmias e. cardiac arrest 3. Gastrointestinal tract a. Nausea and vomiting b. Abdominal cramps c. Diarrhea 4. Skin a. Urticaria b. Flushing c. Pruritus 5. Others a. Headache b. Uterine contractions Management 1. Treat as a Medical Emergency. 2. Monitor ABC’s 3. Aqueous epinephrine – primary drug used; given SQ 4. Diphenhydramine 1 mg/kg 5. Cimetidine 4 mg/kg 6. For shock – give initial bolus of 20 ml/kg NSS or Plain LR 7. Hydrocortisone 5 mg/kg 8. Salbutamol nebulization – for bronchoconstriction POISONING: SPECIFIC INGESTIONS I. SALICYLATE (ASPIRIN) 1. Decreased incidence - acetaminophen 2. Toxic dose - > 250 mg/kg 3. Methyl salicylate - 1365 mg salicylate/ml 4. Diagnostic findings a. Tachypnea and deep labored breathing b. Hyperthermia 5. II. c. Tinnitus d. Changes in sensorium – seizures and coma Management a. Stabilize ABC’s. b. Induce emesis or assist in gastric lavage. c. Monitor neurovital signs. BP and urine output. d. Treat hyperpyrexia with TSB or cooling blanket. e. Seizure precautions. e. Administer emergency drugs as prescribed. i. Sodium bicarbonate and KCl ii. Activated charcoal ( 1-2 gm/kg/dose) iii. Diazepam for seizures ACETAMINOPHEN 1. Widely used antipyretic – analgesic. 2. Metabolized in the liver. 3. Recommended dose – 10 – 20 mg/kg/dose q 4 hours. 4. Diagnostic findings: a. Gastric irritation – diarrhea, vomiting. b. Diaphoresis c. Hepatic failure d. Encephalopathy, coma and death 5. Management a. Stabilize ABC’s. b. Induce emesis or assist in gastric lavage. c. Monitor neurovital signs. BP and urine output. d. Seizure precautions. e. Administer emergency drugs as prescribed. i. N-acetylcysteine 20% (Mucomyst) – w/in 8 to 24 hrs of ingestion ii. Activated charcoal ( 1-2 gm/kg/dose) iii. Diazepam for seizures iv. Antiemetics III. HYDROCARBONS 1. Viscosity a. < 60 SSU: kerosene, gasoline b. < 100 SSU: diesel oil, mothballs, lubricating grease 2. Diagnostic findings: a. Initial ingestion: coughing, dyspnea and choking. b. Pulmonary symptoms: i. tachypnea ii. wheezing iii. respiratory distress c. CNS depression or excitement d. Nausea, vomiting and abdominal pain e. Cyanosis 3. Management: a. Stabilize ABC’s. b. Decontaminate patient: remove clothing and wash skin. b. Induce emesis or assist in gastric lavage. i. Severe GI symptoms ii. Severe CNS symptoms c. Monitor RR. Observe character of respirations. d. Administer drugs as prescribed. i. Antibiotics ii. Steroids IV. ORGANOPHOSPHATES 1. Widely used as pesticides. 2. Action: inhibit acetylcholinesterase a. S - salivation b. L - lacrimation c. U - urinary incontinence d. D - defecation e. G - GI cramping f. E - emesis 3. Management a. Stabilize ABC’s b. Decontaminate patient. c. d. d. V. Induce emesis or assist in gastric lavage. Monitor vital signs. Administer drugs as prescribed. i. Atropine – drying of secretions ii. Pralidoxime – reactivates acetylcholinesterase IRON 1. Diagnostic Findings a. Stage 1: initial period ( ½ to 6 hrs after ingestion) vomiting, diarrhea, abdominal pain, hematemesis b. Stage 2: latent period (2 to 12 hrs) – patient improves. c. Stage 3: systemic toxicity 4 to 24 hours after ingestion – shock, fever, hyperglycemia, bleeding, metabolic acidosis d. Stage 4: hepatic failure beginning at 48 to 96 hrs – associated with seizures and coma. e. Stage 5 – Late sequelae of pyloric stenosis 2. Management a. Stabilize ABC’s b. Induce emesis or assist in gastric lavage. c. Monitor neurovital signs. BP and urine output. d. Seizure and aspiration precautions. e. Administer emergency drugs as prescribed. ii. Deferoxamine – 15 mg/kg/hr for 8 hrs IV DROWNING AND NEAR – DROWNING Definition: 1. Drowning - situation wherein the victim of a submersion episode dies immediately or within 24 hours of the hypoxic insult. 2. Near – drowning – victim may survive but require intensive support. Incidence: 1. Peak incidence – children < 4 years and ages between 15 to 24 years 2. Alcohol related – 38% among boys 15 – 19 years Pathology: 1. Freshwater drowning – disrupts surfactant -> atelectasis and pulmonary edema 2. Saltwater drowning – causes fluid movement along an osmotic gradient -> flooding of alveoli with protein-rich plasma and pulmonary edema Cause of Death: 1. Laryngospasm 2. Cerebral hypoxia 3. Carbon dioxide narcosis 4. Cardiac arrest 5. Aspiration Diagnostic findings: 1. Rales or crackles 2. Frothy sputum 3. Rhonchi or wheezing 4. Respiratory failure 5. Dysrhytmias 6. Seizures 7. Coma Poor outcome: 1. < 3 years of age 2. Maximum submersion time > 5 minutes 3. Resuscitation efforts not attempted for at least 10 minutes after rescue 4. Seizures, fixed and dilated pupils, flaccid extremities, coma 5. Arterial pH 7.10 or less Emergency management: 1. Stabilize ABC’s 2. Remove foreign body in airway. 3. Administer humidified oxygen. 4. Maintain ventilation. Insert endotracheal tube. Indications: a. apnea b. oxygen saturation < 90% while inspiring 100% oxygen c. signs of neurologic dysfunction 5. Meticulous monitoring of vital signs. 6. Insert NGT and urinary catheter. 7. Administer medications as prescribed. a. sodium bicarbonate b. anticonvulsants c. antibiotics d. steroids e. analgesics 8. Emotional support for the family.