Ecology of Increasing Disease Population growth and
advertisement

Ecology of Increasing Disease
Population growth and environmental degradation
Bioscience Vol. 48 No. 10 October, 1998
David Pimentel, Maria Tort, Linda D’Anna, Anne Krawic, Joshua Berger, Jessica Rossman, Fridah
Mugo, Nancy Doon, Michael Shriberg, Erica Howard, Susan Lee, and Jonathan Talbot
David Pimentel ( email: dpl8@cornell. edu ) is a professor in the College of Agriculture and Life
Sciences, Cornell University, Ithaca, NY 14853-0901. Maria Tort, Linda D’Anna, Anne Krawic, Joshua
Berger, Jessica Rossman, Fridah Mugo, Nancy Doon, Michael Shriberg, Erica Howard, Susan Lee, and
Jonathan Talbot are graduate students in the College of Agriculture and Life Sciences, Cornell
University, Ithaca. NY 14853-0901.
All populations of organisms, including humans, are limited partially or completely by diseases in their
ecosystems (Real 1996). Disease prevalence in populations and ecosystems is influenced by numerous
environmental factors, including infectious organisms such as fungi and viruses, pollutants such as
chemical and biological wastes, and shortages of food and nutrients (Dubos 1965). This complex of
factors and their interactions makes tracking and assessing the causes and effects of individual
diseases extremely difficult (McMichael 1993). For example, when a human is infected by a parasite
that is drawing heavily on nutrients in the human, such as a blood parasite, it is difficult to
determine whether the individual died from malnutrition or from the parasitic infection. It is more
likely that death was due to a combination of factors. In addition, air, water, or soil pollutants or
other stresses that affect humans and other species in the ecosystem add to the complexity of the
situation.
Disease dynamics are further complicated by the increased density of humans because high
densities facilitate the increase and spread of infectious organisms among people (Lederberg et al.
1992, WHO 1992). Rapidly expanding human populations and widespread environmental degradation
contribute to expanded world disease problems (WHO 1992, 1996c). Human plagues such as the
Black Death, cholera, tuberculosis (TB), and HIV are essentially problems of dense urban
populations. Crowded conditions in urban areas provide the ideal environment for the culture and
spread of old diseases, such as cholera and TB, as well as for many newly emerging diseases, such as
HIV (McMichael 1993).
Today, infectious diseases cause approximately 37% of all deaths worldwide (Real 1996). Moreover,
we have calculated that an estimated 40% of world deaths can be attributed to various
environmental factors, especially organic and chemical pollutants. In addition, more than 3 billion
humans suffer from malnutrition (WHO 1996e), and 4 million infants and children die each year from
diarrhea, which is caused largely by contaminated water and food (WHO 1992, 1995).
Newly developed chemicals also have increased the varieties, potencies, and quantities of chemicals
that are available to humans and released into the air, soil, and water. These chemicals have
increased ecosystem pollution and caused serious disease problems in humans. Worldwide, an
estimated 100,000 different chemicals are used each year (Nash 1993). The United States uses
over 2700 billion kg of chemicals each year, of which at least 20 billion kg are considered hazardous
(WRI 1994).
In this article, we assess the relationship between high population density and increasing
environmental degradation. We also examine the effects of both factors (separately and in
combination) on present and future disease incidence throughout the world.
Population growth and disease transmission
Based on current growth rates, the world’s population will double to 12 billion in the next 50 years,
intensifying pollution and disease problems. The US population alone will double to 540 million during
the next 70 years (PRB 1996, USBC 1996). Environmental problems are already particularly severe in
urban areas of the world, in which the number of people continues to double especially quickly (i.e.,
every 20-25 years). By the turn of the century, according to projections, more than one-half of the
world's population will live in cities that have more than 1 million people, and by 2025, two-thirds of
the world's population will have settled in large urban areas (WRI 1994).
Densely crowded urban environments, especially those without adequate sanitation, are of great
public health concern because they are sources of disease epidemics (Iseki 1994). For example,
dengue fever -- spread by the mosquito Aedes aegypti, which breeds in tin cans, old tires, and other
water-holding containers -- is already expanding rapidly in crowded tropical cities (Lederberg et al.
1992). Dengue fever has increased dramatically since 1980, with 30-60 million dengue infections now
occurring each year (Table 1; Monath 1994).
Table 1. Human infections and deaths from water-related diseases each year
worldwide.
Disease
Number of infected people
Number of deaths
Reference
Diarrhea
2 billion
4 million
WHO 1992
Ascariasis
0.8-1 billion
20,000
WHO 1992
Filariasis
900 million
NA
WHO 1992
Schistosomiasis
600 million
1 million
Nash 1993
Malaria
300-500 million
2.7 million
Travis 1997
Amoebiasis
500 million
NA
WHO 1992
Trichuriasis
500 million
100,000
WHO 1992
Dengue fever
30-60 million
21,000
WHO 1992
Onchocerciasis (river blindness)
18 million
20,000-50.000
WHO 1992
Leishmaniasis
12 million
NA
WHO 1992
Dracunculiasis
10 million
NA
WHO 1992
Trachoma (blindness)
6-9 million
NA
WHO 1992
Typhoid and Paratyphoid
1 million
25,000
WHO 1992
Cholera
210,000
10,000
WHO 1992
Yellow fever
10-25,000
NA
WHO 1992
Total
~ 5 billion
~ 6 million
Based on the increase in air, water, and soil pollutants worldwide, we estimate that 40% of human
deaths each year result from exposure to environmental pollutants and malnutrition. These deaths
are in addition to the toll taken by infectious diseases. Automobile use and energy consumption,
which are steadily increasing in densely populated cities, are just two of the many sources of
environmental pollution that contribute to the growing number of human illnesses and deaths (WHO
1992, 1995).
The toxic chemicals to which humans are exposed include benzene, lead, pesticides, and cyanides. In
addition, approximately 3.5 billion kg of toxic metals are released into the US environment annually
(WRI 1994). Environmental factors, including various chemicals, ultraviolet and ionizing radiation, and
tobacco smoke, are estimated to cause roughly 80% of all cancers (Murray and Lopez 1996). Of the
approximately 80,000 chemicals in use today, including many pesticides used in the United States,
nearly 10% are recognized as carcinogens (Darnay 1994, Newton and Dillingham 1994). Annually,
approximately 5 million cancer deaths are reported worldwide (Murray and Lopez 1996). In the
United States, cancer-related deaths from all causes increased from 331,000 in 1970 to
approximately 521,000 in 1992 (USBC 1996). Of these, an estimated 30,000 can be attributed to
chemical exposure (McGinnis and Forge 1993).
Moreover, human exposure to chemicals may be increasing in the United States (Pimentel and
Bashore 1998). The use of chemicals increased from approximately 3500 kg per person per year in
1941 to more than 10,000 kg per person per year in 1995 (FASE 1996). The prevalence of illnesses
due to chemical exposure has also grown.
Water pollution and diseases
Waterborne infections account for 80% of all infectious diseases world wide and 90% of all
infectious diseases in developing countries (Table 1; Epstein et al. 1994). Lack of sanitary conditions
contributes to approximately 2 billion human infections of diarrhea, resulting in approximately 4
million deaths each year, mostly among infants and young children (WHO 1992). Even in developed
countries, waterborne diseases are significant. In the United States, they account for 940,000
infections and approximately 900 deaths each year (Seager 1995).
Approximately 1.2 billion people in developing nations lack clean, safe water because most household
and industrial wastes are dumped directly into rivers and lakes without treatment, which contributes
to the rapid increase in waterborne diseases in humans (Gleick 1993). Developing countries discharge
approximately 95 % of their untreated urban sewage directly into surface waters (WHO 1993c). For
example, of India's 3119 towns and cities, just 209 have partial treatment facilities, and only 8 have
full wastewater treatment facilities (WHO 1992). Furthermore, 114 cities dump untreated sewage
and partially cremated bodies directly into · the sacred Ganges River (NGS 1995). Then, downstream,
the untreated water is used for drinking, bathing, and washing. This situation is typical of many
rivers in developing countries. Similarly, in Alexandria, the production site for approximately 40 % of
Egypt's total industrial output, untreated wastes are discharged into the Mediterranean Sea and
Lake Maryut (WHO 1992). Over the past decade, pollution has resulted in an 80% decline in fish
production in Lake Maryut and has contributed to the malnutrition problem (WHO 1992).
Agricultural runoff threatens the world's drinking water because of the animal and chemical wastes
present in field runoff entering rivers and other aquatic ecosystems. In the United States, nearly
50% of lake water is polluted by erosion runoff containing nitrates, phosphates, and other
agricultural chemicals (Gleick 1993).
Some disease outbreaks in the United States are due to microbial pollution and the spread of two
protozoan pathogens, Cryptosporidium parum and Giardia lamblia. A water survey conducted in 1992
revealed that nearly 40% of treated drinking-water supplies in the United States are contaminated
with these organisms (Platt 1996k During tile past 30-40 years, the number of infections in the
United States caused by these waterborne organisms has increased (Guerrant 1997). For example, a
serious outbreak of cryptosporidiosis that occurred in Milwaukee, Wisconsin, in the spring of 1993
was attributed to the contamination of the city's drinking water. As a result, 403,000 cases of
diarrhea and 4400 hospitalizations occurred (CDC 1994).
Cholera, a well-known waterborne disease, continues to be a serious global problem. Vibrio cbolerae
outbreaks are closely associated with climatic cycles (e.g., El Niño Southern Oscillation) and ocean
plankton blooms (Colwell 1996). These associations suggest the potential influence of global warming
on the spread of certain diseases (Colwell 1996). In 1988, there were approximately 50,000 cases of
cholera, but by 1991 that number rose to 600,000; deaths increased from 2000 to 18.000 over the
same period (Gleick 1993). However, from 1991 to 1995 the number of cholera cases declined
worldwide to approximately 210,000 per year because of effective public health efforts.
Schistosomiasis, which is associated with contaminated fresh water, is expanding worldwide and
currently causes an estimated 1 million deaths annually (Table 1). This expansion is due to an increase
in suitable habitats for the snail intermediate-host population resulting from various human
activities, including construction of dams and irrigation channels (Shiklomanov 1993). For example,
construction of the Aswan High Dam in Egypt and related irrigation systems in 1968 led to an
explosion in the prevalence of Schistosoma mansoni in the population; it increased from 5% in 1968
to 77% in 1993 (Shiklomanov 1993).
Also associated with water is mosquito-borne malaria. This disease infects more than 500 million
humans each year, killing approximately 2.7 million (Table 1; Marshall 1997, Travis 1997).
Approximately 90% of all malaria cases occur in Africa, as do 90-95% of the world's malaria-related
deaths. Between 1970 and 1990 in the African countries of Rwanda and Togo, the increase in malaria
incidence ranged from fourfold to more than 150-fold, and it continues to rise (Figure 1).
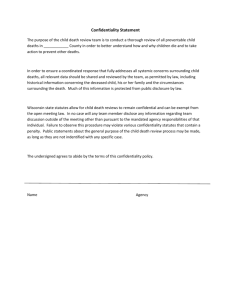
Figure 1. Trends of malaria incidence in Rawanda and Togo.
Solid line Rawanda, dashed line Togo.
After Brinkmann and Brinkmann 1991.
In some regions of Asia and South America, malaria prevalence decreased from 1950 until 1980 and
has since remained fairly stable, at approximately 5 million cases per year (Najera et al. 1992). But
in other regions, the number of malaria cases is now increasing. For example, Peru recorded
approximately 34,000 cases of malaria in 1991 but approximately 55,000 cases in 1992 (WHO
1996g). Similarly, in Bangladesh, malaria prevalence increased from approximately 33,000 cases in
1988, to 64,000 cases in 1991, to 125,000 cases in 1993 (WHO 1996h).
Environmental changes, including more polluted water, have fostered the high incidence and increase
of malaria. Deforestation in parts of Africa has exposed land to sunlight and promotes the
development of temporary pools of water, thus favoring the breeding of human-biting, malariatransmitting mosquitoes, Anopheles gambiae (Coluzzi 1994). With some African populations doubling
every 20 years, more people are living in close proximity to water ecosystems that are suitable for
mosquito breeding. Concurrently, mosquito vectors are evolving resistance to insecticides that are
polluting aquatic ecosystems, and protozoan pathogens are evolving resistance to antimalarial drugs,
reducing the effectiveness of control efforts (Georghiou 1990, Olliaro et al. 1996).
Atmospheric pollution and diseases
Each year, air pollutants adversely affect the health of 4-5 billion people worldwide (World Bank
1992, Leslie and Haraprasad 1993, WHO/UNEP 1993). Air pollution is increasing because of the
activities of the expanding world population: the burning of fossil fuels, the increased emissions of
industrial chemicals, and the increased use of automobiles. In particular, automobile numbers are
growing approximately three times faster than the world population (WHO/UNEP 1993). Although
governmental efforts since the 1950s have led to significant improvements in urban air quality in
many developed nations, overall emissions continue to rise with the expanding human population.
Because developing and East European nations have negligible pollutant emission controls, living
conditions are becoming especially hazardous in their growing urban areas.
By 1993, air pollution levels in all 20 of the world's largest cities exceeded World Health
Organization guidelines (WHO/UNEP 1993). For example, during the winter months, particulate
concentrations in Santiago, Chile, were among the highest observed in world urban areas {300-400
ug/m3). Los Angeles has the highest density of automobiles per person in the world, so it is not
surprising that EPA standards for ozone levels were exceeded at all city monitoring stations in 1990.
Moreover, the average exposure to carcinogens from automobiles in Los Angeles is as much as 5000
times greater than the level considered acceptable by the EPA (Mann 1991, Wilken 1995).
Air pollution is also rampant in China, where less than 1% of 500 Chinese cities surveyed have clean
air (Zimmerman et al. 1996). From 1955 to 1984, the prevalence of respiratory diseases in China rose
by 50%. Respiratory diseases occur at a rate five times higher in China than in the United States;
indeed, they are the leading cause of death in China (Zimmerman et al. 1996).
Compounding this public health problem is a nearly fivefold increase in cigarette use in China over
the past few decades, from approximately 360 to nearly 1800 cigarettes per person each year
(World Bank 1992). Although Chinese males smoke 98% of the cigarettes, mortality due to lung
cancer is approximately equal in males and females (Leslie and Haraprasad 1993).
The problem of respiratory diseases is not limited to China. Worldwide, the incidence of respiratory
disease is increasing along with cigarette use. In fact, the two major underlying causes of premature
death in the world are the significant increases in tobacco use and HIV. Exhaled tobacco smoke
contains more than 3800 chemicals, including numerous carcinogens (Hulka 1990). Smoking causes
approximately 3 million deaths annually, 2 million in developed countries and 1 million in developing
countries (WHO 1995, Murray and Lopez 1996). In industrialized nations as a whole, the prevalence
of lung cancer increased approximately threefold from 1950 to 1986. US death rates from lung
cancer alone increased nearly fourfold between 1950 and 1990 (WHO 1994). In 1990, nearly 419,000
US deaths were attributed to smoking (WHO 1994). By 2020, predictions are that tobacco will
cause 10 million deaths per year worldwide (Murray and Lopez 1996).
Globally, but especially in developing nations where people cook with fuelwood and coal over open
fires, approximately 4 billion humans suffer continuous exposure to smoke (WHO 1992, World Bank
1992, Leslie and Haraprasad 1993, WHO/UNEP 1993). This smoke, which contains large quantities of
particulate matter (Leslie and Haraprasad 1993) and over 200 chemicals, including several
carcinogens (Godish 1991), results in pollution levels that are considerably above those considered
acceptable by the World Health Organization (WHO 1992, World Bank 1992, Leslie and Haraprasad
1993, WHO/UNEP 1993). Fuelwood cooking smoke is estimated to cause the death of 4 million
children each year worldwide (World Bank 1992). In India, where people cook with fuelwood and
dung, particulate concentrations in houses are reported to range from 8300 to 15,000 ug/m 3, greatly
exceeding the 75 ug/m3 maximum standard for indoor particulate matter in the United States
(Christiani 1993).
Radon radiation from the earth, another indoor air pollution hazard, is a growing problem, in part
because of the modern construction of airtight houses. During the past 30 years there has been a
four- to five-fold increase in radon concentration in houses in Sweden (Lindvail 1992). In the United
States, radon radiation is considered to be a significant cause of lung cancer, causing approximately
14,000 deaths per year (CEQ 1996).
In general, air pollutants exacerbate asthma, which ultimately can become severe enough to cause
death. Worldwide, the incidence of asthma has increased nearly 50%, from 1.3 cases per 100,000
people in 1980 to 1.9casesper 100,000in 1989 (WHO 1993a). Deaths of children younger than 5
years of age from acute respiratory infections more than doubled, from 2.2 million worldwide in
1985 (USBC 1996) to the current level of approximately 5 million per year (WHO 1995). In addition,
400 million cases of acute lower respiratory infections are reported each year, of which an
estimated 4.4 million are fatal (WHO 1996f).
Atmospheric pollution also adversely affects the stratospheric ozone layer, which protects
organisms from heavy doses of ultraviolet radiation (McMichael 1993). Before October 1980 at the
South Pole, which is the site of the greatest ozone depletion, the measures ranged between 250 and
325 DU (Dobson Units). These values have declined to dangerous levels -- between 125 and 175 DU.
The acceptance of the 1987 Montreal Protocol has helped to reduce the worldwide production, use,
and release of ozone-destroying chlorofluorocarbons (McMichael 1993). However, the ozone layer
continues to be depleted, in part from the release of pollutants from increased burning of wood and
from the worldwide use of the methyl-bromide fumigant (Coleman et al. 1993).
Estimates are that every 1% decrease in the ozone layer increases cancer-inducing UV-B radiation
by 1.4% (McMichael 1993). Exposure to sunlight, including UV-B radiation, accounts for 70% of skin
cancers in the United States (McMichael 1993). At present, skin cancer prevalence is increasing
between 30% and 50% every 5 years in many North American Caucasian populations (Coleman et al.
1993). For example, in the United States, the prevalence of new cases of skin cancer increased from
approximately 10,000 cases in 1975 to 40,000 in 1996, while the number of deaths from skin cancer
rose from approximately 4000 to 9490 (Schultz 1997).
Although the use of lead in US gasoline has declined since 1985, yearly emissions of lead into the
atmosphere from other sources remain near 2 billion kg and continue to threaten public health (O
ECD 1985). Lead poisoning causes anemia, kidney problems, and brain damage. Children exposed to
lead are particularly at risk of brain damage and reduced learning capabilities (Ittenbach et al. 1995,
Renner 1995). Even now, an estimated 1.7 million children in the United States are exposed to
hazardous levels of lead and have blood levels above the acceptable level of 10 ug/dL (CEQ 1996).
Benzene, a carcinogen that causes leukemia even from exposure to low dosages (1-30 ppm), is a
common component of gasoline and is therefore released into the atmosphere (Krstic 1994, UKDE
1996). From 1950 to 1980, US benzene production increased from 0.7 billion kg to 4.6 billion kg, and
production is currently approximately 7.4 billion kg/yr (WR11994). Although the general use of
benzene as a solvent has decreased as its negative effects have become better known (Krstic 1994,
UKDE 1996), benzene use needs to be further reduced to lessen current public health problems.
Pesticide pollution and disease
Since the first use of DDT for crop protection in 1945, the global use of pesticides in agriculture
continues to expand. From approximately 50 million kg of pesticides in 1945, global usage has since
risen 50-fold, to approximately 2.5 billion kg/yr worldwide (Pimentel 1995). In the United States,
the use of synthetic pesticides has grown 33-fold since 1945, to approximately 0.5 billion kg/yr
(Pimentel 1995). The increase in related hazards is greater than the increase in applied amounts
because most modern pesticides are more than 10 times as toxic to organisms than those used in the
early 1950s (Pimentel 1995).
In 1945, when synthetic pesticides were first used, few human pesticide poisonings were reported.
But by the late 1960s, when pesticide use and toxicity had increased dramatically, the number of
human pesticide poisonings also rose (Pimentel 1995). In California, the use of pesticides increased
from 68 million kg in 1950 to 269 million kg in 1988, while the number of reported human poisonings
rose from 115 to 903 cases per year (Maddy et al. 1990). The total number of pesticide poisonings in
the United States increased from 67,000 in 1989 to the current level of 110,000 per year (Litovitz
et al. 1990, Benbrook et al. 1996). This trend continues today.
By 1973, when global pesticide use was approximately 1.3 billion kg/yr, the number of human
pesticide poisonings reached an estimated 500,000, with approximately 6000 deaths (Labonte 1989).
Two decades later, Pimentel (1995) reported that worldwide pesticide use had risen to
approximately 2.5 billion kg. By 1992, approximately 3 million human pesticide poisonings were
reported each year, with approximately 220,000 fatalities and 750,000 cases of chronic illnesses
(WHO 1992).
Available US data indicate that 18% of all pesticides and approximately 90% of all fungicides are
carcinogenic and pose a hazard to human health (NAS 1987). Several other studies substantiate the
adverse effects of pesticides on the human respiratory system. For example, among a group of
professional pesticide applicators, 15% suffered asthma, chronic sinusitis, or chronic bronchitis,
compared with only 2% for people who used pesticides infrequently (Weiner 1972).
In addition, pesticides, especially the organophosphate and carbamate classes, adversely affect the
nervous system by inhibiting cholinesterase. This problem is particularly critical for children because
their brains are more than five times larger in proportion to body weight than the brains of adults.
In California, 40% of the children working in agricultural fields have blood cholinesterase levels
below normal, a strong indication of organophosphate and carbamate pesticide poisoning (Repetto
and Baliga 1996).
The effect of land degradation on disease incidence
Soil is easily contaminated by a wide array of chemicals and pathogens. Humans may acquire chemical
pollutants and pathogens directly from the soil (i.e., by contact with it) or indirectly, through food
and water. At times, soil particles themselves may be pollutants, entering the eyes, nose, and mouth
and acting as irritants or allergens.
Cleared and exposed soil is highly susceptible to wind and water erosion. Wind erosion can cause
serious health problems by blowing soil particles and microbes into the air. These windborne
particles irritate the respiratory tract and eyes while aggravating allergies and asthma. Erosion also
disperses toxic chemicals, such as heavy metals and pesticides, leading to contaminated food and
water. Furthermore, erosion strips soil of its nutrients and thus lowers food crop productivity and
ultimately reduces human nutrition.
As people invade natural ecosystems and land is cleared of trees, soil is exposed and the chances
increase of humans becoming infected by helminths, such as hookworms, and microbes, such as
pathogenic Escherichia coli (WHO 1992). Such increases were observed in 1984 in Nepal, a
mountainous country that is experiencing serious soil erosion and severe disease problems: 87% of
the population was infected with helminths (Suguri et al. 1985, Metz 1991). Children suffer greater
morbidity from helminthic infections than adults because children need more protein than adults per
kilogram of body weight; under severe parasitic infections, they may be unable to utilize protein
efficiently enough to remain healthy.
In addition, many helminth species that infect humans are found in soil contaminated by human
feces, thereby exacerbating the cycle of exposure. Worldwide, approximately 2 billion people are
estimated to be infected with one or more helminth species, either by direct penetration or by
consumption of contaminated food or water (Hotez et al. 1996). The most prevalent helminths are
hookworms (Necator americanus and Ancylostoma duodenale), Strongyloides (Strongyloides
stercoralis), and Ascarids (Ascaris lumbricoides). In locations in which sanitation is poor and people
are overcrowded, as in parts of urban Africa, up to 90% of the population may be infected with one
or more helminth species (Stephen-son 1994).
Food contamination, disease, and malnutrition
Worldwide, reported cases of food-borne diseases are as high as 240 million per year (WHO 1990).
In the United States, approximately 6.5 million foodborne disease cases occur each year, causing
approximately 9000 deaths (Todd 1996).
Poultry, hogs, cattle, and other animals are easily contaminated with Salmonella enteritidis and
various E. coli microbes, especially when they are crowded together in husbandry facilities with
inadequate waste disposal systems (Lederberg et al. 1992). Further microbial contamination can be
caused by unsanitary conditions during slaughtering, processing, and handling. In the United States,
hen eggs have been identified as the main source of S. enteritidis, which can cause severe
gastrointestinal illnesses and sometimes death in humans, especially among children and the infirm
(Altekruse and Swerdlow 1996). Worldwide, between 1979 and 1987, S. enteritidis infections
increased significantly in 24 of the 35 countries reporting to the World Health Organization
(Altekruse and Swerdlow 1996).
Malnutrition, which includes inadequate intake of calories, protein, and numerous essential vitamins
and minerals, is a major disease related to environmental degradation. Malnutrition prevails in
regions in which the overall food supply is inadequate, where populations lack economic resources to
purchase food, and where political unrest and instability interrupt food supplies. In addition, rapidly
expanding human populations intensify the food-supply problems by diminishing the per capita
availability of cropland (Pimentel and Pimentel 1996).
In 1950, 500 million people (20% of the world population) were considered malnourished (Grigg
1993). Today more than 3 billion people (one-half of the world population) suffer from malnutrition
(WHO 1996e), the largest number and the highest rate in history. Each year, between 6 and 14
million people die from malnutrition (Murray and Lopez 1996). Malnutrition problems are also on the
increase in the United States, especially among the poor.
In many parts of the world, especially in developing countries, severe shortages of vitamin A cause
blindness and death. For example, in the Sahelian region, as well as in west and east Africa, per
capita consumption of vitamin A has been declining during the past 10-20 years, while associated
serious eye problems have been increasing (ACC/SCN 1992). Worldwide, approximately 258 million
children are vitamin A deficient (WHO 1996e). Each year, vitamin A deficiency causes approximately
2 million deaths and 3 million serious eye problems, including blindness (Murray and Lopez 1996).
Similarly, iron intake per person has been declining during the past 10-30 years, especially in subSaharan Africa, south Asia, China, and South America, because of inadequate nutrition resulting
from overall shortages of food (ACC/SCN 1992). Globally, more than 2 billion people are iron
deficient, and the problem is severe enough that 2 billion people suffer from anemia (WHO 1996e).
Worldwide, an estimated 20% of malnutrition deaths can be attributed to anemia (Murray and Lopez
1996). In addition, approximately 1.6 billion people live in iodine-deficient environments and suffer
from iodine-deficiency disease (WHO 1996e).
Malnutrition, complicated by parasitic infections, is frequently found in poverty-stricken areas with
inadequate sanitation. Malnourished individuals, especially children, are seriously affected by
parasitic infections because these infections can reduce nutrient availability. The presence of
intestinal parasites frequently diminishes appetite and food intake. Their presence also increases
the loss of nutrients by causing diarrhea and dysentery. Hookworms, for instance, can suck as much
as 30 mL of blood from an infected person each day, gradually weakening individuals and lowering
their resistance to other diseases (Hotez and Pritchard 1995). Because an estimated 5-20% of an
individual's daily food intake is used to offset the effects of parasitic illnesses, the overall
nutritional status of a parasite-infected person is greatly diminished over time (Pimentel and
Pimentel 1996).
Drug resistance in microbes
Drug resistance and rapid changes in microbes contribute to global disease outbreaks, diminishing
the ability to successfully control the illnesses they cause (Daily and Ehrlich 1996, Grady 1996). At
least 11 major microbes, including Streptococcus spp., Staphylococcus spp., Shigella spp.,
enterobacteriaceae, and enterococci, have already become highly resistant to standard antibiotic
treatment.
The evolution of drug resistance in microbes can be surprisingly rapid. In 1979, only 6% of European
pneumococcus strains were resistant to penicillin, but one decade later that percentage had grown to
44% (Platt 1996). Currently, in the United States, more than 90% of the strains of Staphylococcus
aureus, one of the most common disease-producing microbes, are resistant to penicillin and similar
previously effective antibiotics (ASM 1994). South African studies indicate that 40% of the invasive
Streptococcus pneumoniae acquired in the community and 95% of the isolates acquired in hospitals
are now resistant to penicillin (WHO 1996c).
Rapid increase in drug resistance by disease organisms is caused by the widespread and overuse of
more than 300 antibiotics by the medical profession (ASM 1994). In addition, one-half of the
antibiotics used in the United States to treat humans are also used to treat disease-infected
domestic animals (ASM 1994). The concurrent use of antibiotics for both humans and livestock
enhances selection for drug-resistant microbes, further exacerbating the problem of antibiotic
resistance.
Re-emerging diseases
The spread of new strains of E. coli is due in part to the rapidly expanding human population,
especially in areas where humans are crowded and where water and food contamination are rampant
(Table 2; Iseki 1994, Daily and Ehrlich 1996, Grady 1996).
Table 2. New and re-emerging infectious diseases in humans since 1976.a
Disease
Year of emergence and reemergence
Country
AIDS
1975
Africa
Legionnaires disease
1976
United States
Cryptosporidiosis
1976
United States
Ebola haemorrhagic fever
1976
Zaire
Hantavirus
1977
Republic of Korea
Creutzfeldt-Jakob disease (CJD)
1979
United Kingdom,
Canada
Human T-cell lymphotropic virus 1
1980
Japan
Hepatitis D
1980
Italy
Escherichia coli O157:H7
1982
United States
New variant of CJD (related to mad cow
disease)
1986
United Kingdom
Salmonella enteritidis PT-4
1988
United Kingdom
Hepatitis C
1989
United States
Venezuelan haemorrhagic fever
1991
Venezuela
Brazilian haemorrhagic fever
1994
Brazil
Vibrio cholerae
1992
India
Human and equine morbillivirus
1994
Australia
a
WHO 1996f, Stratton et al. 1997.
The worldwide increase in TB also results from population crowding and drug resistance (WHO
1996f). Currently, an estimated 1.7 billion people worldwide are infected with TB, with approximately
95 % of TB deaths occurring in developing countries. In 1990, the number of new TB infections was
7.5 million; by 1995, new infections numbered 8.9 million; and by 2000, a total of 10.2 million new
cases are expected (Lederberg et al. 1992, WHO 1996f). TB deaths per year have been estimated at
2.5 million in 1990 and 3.0 million in 1995 and are projected to rise to 3.5 million by 2000 (WHO
1996f). At present, TB kills more people each year than any other infectious disease in the world
(WHO 1996f).
Patterns of TB infection in the United States are similar to the world situation, in which TB cases
increased by approximately 18% from 1985 to 1991 (USC 1993). Currently, approximately 37,000
new infections occur each year, up from approximately 23,000 in 1985 (USC 1993). Drug-resistant
TB strains and reduced medical treatment account for this increase. TB treatment is further
complicated by the use of illegal drugs and the rise in HIV infections, both of which help to spread
the disease and lead to frequent reinfection (USC 1993).
Filoviruses are another re-emerging pathogenic disease. These viruses -- of which there are two
groups, Ebola and Marburg -- cause a severe, usually fatal hemorrhagic disease in humans. Outbreaks
of Ebola hemorrhagic fever have resulted in over 1000 reported cases (Clegg and Lloyd 1995). In
addition, over 40 cases of Marburg have been reported. Their rapid spread and the high mortality
they cause make filoviruses a major public health concern. In reported outbreaks, 50-90% of the
cases have been fatal (Clegg and Lloyd 1995). Increased international commerce and travel, limited
experience in diagnosis and case management, importation of nonhuman primates, and the potential
of filoviruses to evolve rapidly add to health threats and make curtailment difficult (McMichael
1993, Morse 1997).
Brucellosis is another resurgent communicable disease. The causative bacteria, Brucella spp., infect
cattle, sheep, goats, and some wild mammals worldwide and are harbored in the animal's udder.
Humans usually contract the disease from infected animals or contaminated dairy products. The
World Health Organization reports that the number of cases of brucellosis is increasing, especially
in developing areas of the Mediterranean regions, the Middle East, western Asia, and parts of Africa
and Latin America (WHO 1997b). Currently, in just six countries of the Middle East, the number of
reported cases is 90,000 per year (WHO 1993b).
Human plague is also on the rise. The plague parasite, Yersinia pestis, is transmitted by human
contacts and interactions with rodents (WHO 1996b). In the 1980s, reported cases in the world
numbered 1327; in 1993, they numbered 2194; and in 1994, they numbered 2935 (WHO 1996b).
Most (nearly 60%) of the reported cases occurred in Africa.
Diphtheria, which had been under control for many years, exploded in Russia after the breakup of
the former Soviet Union. In 1975, only approximately 100 cases were recorded in Russia; by 1990,
that number had increased to 1000, and in 1995, 51,000 new cases were reported (WHO 1996d). The
explosion in diphtheria in Russia is attributed to a decline in the effectiveness of the public health
program.
Newly emerging diseases
Changes in ecosystem biological diversity, evolution of parasites, and invasion by exotic species all
frequently result in disease outbreaks. Several new and emerging diseases are listed in Table 2. For
example, coccidioidomycosis fungal infections caused by Coccidioides immitis have exploded in
California. The number of cases increased from approximately 500 in 1990 to nearly 5000 in 1992
(CDC 1994). With few known effective controls, this disease is expected to continue to spread in the
future (CDC 1994).
An emerging rodent-related disease that is related in part to increasing human numbers is the
hantavirus pulmonary syndrome, which was first identified in 1993 in the United States and Canada
(CDC 1994). By the end of 1995, 135 cases of hantavirus pulmonary syndrome were recognized in the
United States and Canada, with a human mortality rate of 50% (CDC 1994). The disease, which has
experienced a resurgence in the United States in 1998 due in part to increased rainfall associated
with El Niño, has also been reported in several other countries, including Argentina.
In the United States, Lyme disease is the most widespread vector-borne disease, with infections
reported in 47 states. The bacterium that causes Lyme disease, Borrelia burgdorferi, is a spirochete
similar to the one that causes syphilis in humans (WHO 1996f). It is thought to have existed
naturally in the United States without incident until major ecological changes began occurring in the
twentieth century, when suburban areas expanded along with white-tailed deer populations (e.g.,
from 2000 in s 1945 in Massachusetts to 9500 in e 1990; Spielman et al. 1993). Abundant rodent
Peromyscus leucopus and deer tick Ixodes dammini (or a Ixodes capularius) populations enabled the
Lyme disease organism to spread rapidly. Dramatically expanding since the initial description of the
disease in 1976, Lyme disease now infects nearly 12,700 people in the United States each year and
the incidence continues to grow (Table 3; CEQ 1997). Lyme disease is also an increasing problem in
Europe and Asia, with more than 30,000 cases recently reported in Germany (Lederberg et al. 1992).
Table 3. Disease fatalities in the United States.
Disease
1970
1980
1992
AIDSa
0
199b
40,674c
Aseptic meningitisa
6480
8028
12,223
Botulisma
12
89
91
Cancer
163,000
185,000
205,000
Hepatitis Bd
8310
19,015
26,000e
Legioneosisa
Not available
830e
1339
Lyme diseasea
Not available
100f
12,669g
Salmonellosisa
22,000
33,700
42,900
Shigellosisa
13,800
19,000
23,900
Syphilisa
91,000
69,000
113,000
a
USBC 1996.
USBC 1987.
c
CDC 1997.
d
CDC 1989. (For 1987, the number of cases was approximately 26,000.)
e
For 1985.
f
Estimated infections in 1976.
g
CEQ 1997.
b
Another rapidly increasing disease is AIDS, which is caused by HIV (Table 2). The growing human
population, especially the increased number of people in urban areas, has fostered the spread of HIV
and AIDS. It is estimated that in 1970, only 10,000 people were infected with HIV, but at present
approximately 23 million are infected with HIV (WHO 1997a). The total number of AIDS cases is
reported to be 6 million (WHO 1996a), with an estimated 1 million deaths per year (Murray and
Lopez 1996). Approximately 30-50 million people are projected to become HIV positive by the year
2000 (McMichael 1993, WHO 1995).
HIV infections are especially widespread in certain parts of the world (Mertens and Low-Beer 1996).
For example, in Thailand the prevalence of HIV infections in males increased from 1% to 40%
between 1988 and 1992 (Mueller 1993). In 1996, approximately 46,000 Indians out of 2.8 million (1.6
% of the population) tested were found to be infected with HIV (Burns 1996). By the year 2000,
more than 10 million Indians, the largest number of any population in the world, will be infected
(Burns 1996). In the United States, deaths from AIDS are increasing rapidly, from an estimated 199
deaths in 1980 to 40,674 in 1992 (Table 3; USBC 1987, CDC 1997). Although new HIV infections in
homosexual men have started to decline, infections continue to rise in drug users.
Conclusion
The prevalence of human diseases is increasing rapidly worldwide, as is the number of deaths from
diseases. The ecology of increased disease is exceedingly complex because of the diversity of
infectious organisms and the effects of environmental degradation on the prevalence of disease. The
rapid expansion of human populations is a major factor in the rise of human diseases: Humans living
in crowded, urban areas are in an ecosystem that is ideal for the resurgence and rapid spread of old
diseases as well as for the development and spread of new diseases. The unprecedented increase in
air, water, and soil pollutants, including organic and chemical wastes, further stresses humans and
increases disease prevalence. In particular, widespread malnutrition enhances the susceptibility of
humans to infectious pathogens and other diseases.
In addition, global climate changes are improving the environment for some diseases and disease
vectors. Climate changes may also increase the susceptibility of food crops to some pests, which, in
turn, could intensify food shortages and malnutrition. A concurrent problem is the rapid expansion in
the number of "environmental refugees" (Myers 1993). These people, living in poverty and desperate
for food, flee their home areas in a search for survival. Their malnutrition, stress, and dislocation
foster the resurgence of old diseases and the development of new ones.
This analysis confirms that many factors influence the increased prevalence of human diseases now
occurring worldwide. Currently, 40% of deaths result from diverse environmental factors, including
chemical pollutants, tobacco, and malnutrition. The growth in diseases is expected to continue, and
according to Murray and Lopez (1996), disease prevalence is projected to increase 77% during the
period from 1990 to 2020. Infectious diseases, which cause 37% of all deaths throughout the world,
are also expected to rise. Deaths in the United States from infectious diseases increased 58%
between 1980 and 1992, and this trend is projected to continue.
To prevent diseases, poverty, and malnutrition from worsening, the growing imbalance between the
escalating human population and the earth's environmental resources must be dealt with. The
crowding of people into urban areas; the movement of populations into new environments; the
increased use of chemicals that pollute soils, water, and air; the misuse of antibiotics, leading to
resistance in disease microbes; and growing malnutrition all contribute to the worldwide increase of
human diseases. Thus, comprehensive, fair population-control policies combined with effective
environmental management programs are required. Without international cooperative efforts,
disease prevalence will continue its rapid rise throughout the world and will diminish the quality of
life for all humans.
Acknowledgments
We thank the following people for reading an earlier draft of this article and for their many helpful
suggestions: M. Coluzzi, World Health Organization, Rome; D. W. T. Crompton, University. of
Glasgow; P. Epstein, Harvard Medical School; A. R. B. Ferguson, Optimum Population Program, Oxon,
UK: G. P. Georghiou, University of California-Riverside; D. Gubler, Centers for Disease Control, Fort
Collins, Colorado; A. Haines, Royal Free Hospital School of Medicine, London: P. J. Hotez, Yale
University School of Medicine: R. T. Johnson, Johns Hopkins .School of Medicine; V. W. Kimani, Pest
Control Products Board, Nairobi. Kenya; J. Mackay, Asian Consultancy on Tobacco Control, Hong
Kong: A. J. McMichael, London School of Hygiene and Tropical Medicine; N. Myers, Oxford
University; D. M. Parkin, International Agency for Reseach on Cancer, Lyons, France; L. Patrican,
Cornell University; M. Pimentel, Cornell University; L. Piper, Case Western Reserve University; D.
Schwela, World Health Organization, Geneva; J. B. Silkworth, General Electric Corporate Research
and Development; A. Spielman, Harvard School of Medicine; A. Steere, Tufts University School of
Medicine; E. Todd, Bureau of Microbial Hazards, Ottawa, Canada; A. Van Tienhoven, Cornell
University; W. Youngquist, Consulting Geologist, Eugene, Oregon.
References cited
[ACC/SCN] Administrative Committee on Coordination, Subcommittee on Nutrition. 1992.
Second report on the world nutrition situation. Vol. 1. Washington (DC): Administrative
Committee on Coordination, Subcommittee on Nutrition, United Nations.
Altekruse SF, Swerdlow DL. 1996. The changing epidemiology of foodborne diseases. The
American Journal of the Medical Sciences 311: 23-29.
[ASM] American Society for Microbiology. 1994. Report of the ASM task force on antibiotic
resistance. Washington (DC): American Society for Microbiology.
Benbrook CM, Groth E, Hoaaioran JM, Hansen MK, Marquardt S. 1996. Pest management at
the crossroads. Yonkers {NY): Consumers Union.
Burns JF. 1996. Denial and taboo blind India to the horror of its AIDS scourge. New York
Times, 22 September: A1.
[CDC] Centers for Disease Control. 1989. Hepatitis surveillance, April 1989. Atlanta {GA}:
Centers for Disea,e Control and Prevention, Public Health Service, US Department of Health
and Hutnan Services. Report no. 52.
· 1994. Addressing emerging infectious disease threats: A prevention v".:ategy for the United
States. Atlanta (GA): Centers for Disease Control and Prevention, Public Health Service, US
Department of Health and Human Services.
. 1997. AIDS cases, case-fatality rates, and deaths, by half-year and age group, through
December 1997, United States. HIV/AIDS Surveillance Report 9 (2): 19.
[CEQ] Council on Environmental Quality. 1996. Environmental quality. Washington (DC): Council
on Environmental Quality, Executive Office of the President.
. 1997. Lyme disease morbidity and mortality weekly report. Washington (DC): Council on
Environmental Quality, Executive Office of the President. Report no. 45: 1023.
Christiani DC. 1993. Urban and trans-boundary air pollution: Human health consequences. Pages
13-30 in Chivian E, McCally M, Hu H, Haines A, eds. Critical Condition: Human Health and the
Environment. Cambridge (MA): MIT Press.
Clegg JCS, Lloyd G. 1995. Ebola haemorrhagic fever in Zaire, 1995: A perspective. Current
Opinion in Infectious Diseases 8: 225-228.
Coleman MP, Esteve J, Damiecki P, Arslan A, Renard H. 1993. Trends in cancer incidence and
mortality. Lyons (France): International Agency for Research on Cancer.
Coluzzi M. 1994. Malaria and the afrotropical ecosystems: Impact of man-made environmental
changes. Parasitologia 36: 223-227.
Colwell RR. 1996. Global climate change and infectious disease. Science 274: 2025-2031.
Daily GC, Ehrlich PR. 1996. Impacts of development and global change on the epidemiological
environment. Environment and Development Economics 1: 311-346.
Darnay A. 1994. Statistical Record of the Environment. Detroit (MI): Gale Research.
Dubos, R. 1965. Man Adapting. New Haven (CT): Yale University Press.
Epstein P, Ford T, Puccia C, Possas CDA. 1994. Marine ecosystem health. Implications for
public health. Diseases in evolution, global changes and emergence of infectious diseases.
Annals of the New York Academy of Sciences 740: 13-23.
[FASE] Foundation in Advancements in Science and Education. 1996. Research report 1-2.
Washington (DC): Foundation in Advancements in Science and Education.
Georghiou GP. 1990. Overview of insecticide resistance. American Chemical Society
Symposium Series 421: 18-41.
Gleick PH. 1993. Water in Crisis. New York: Oxford University Press.
Godish T. 1991. Air Quality. Chelsea (MI): Lewis Publishers.
Grady D. 1996. Quick-change pathogens gain an evolutionary edge. Science 274: 1081.
Grigg DB. 1993. The World Food Problem. Oxford (UK): Blackwell.
Guerrant RL. 1997. Cryptosporidiosis: An emerging, highly infectious threat. Emerging
Infectious Diseases 3: 1-6.
Hotez PJ, Pritchard DT. 1995. Hookworm infection. Scientific American 272 (6): 68-75.
Hotez PJ, Hawdon JM, Cappello M, Jones BF, Ghosh K, Volvoritz F, Xiao S. 1996. Molecular
approaches to vaccinating against hookworm disease. Pediatric Research 40: 515-521.
Hulka BS. 1990. Measuring exposure and assessing health effects of environmental tobacco
smoke. Pages 16-24 in Kasuga H, ed. Indoor Air Quality. Berlin: Springer-Verlag.
Iseki M. 1994. Effects of increases in the world's population and the globalization of human
life on the incidence of parasitic diseases. Japanese Journal of Parasitology 43: 448-452.
lttcnbach RF, Spencer RM, Jurgens JP, Frate DA, Benson WH. 1995. Metals and school
learning: A review of investigative techniques. Perceptual and Motor Skills 81: 1079-1090.
Krstic G. 1994. Benzene: Chains of influence in deciding exposure limits. Indoor Environment 3:
22-34.
Labonte RN. 1989. Pesticides and healthy public policy. Canadian Journal of Public Health 80:
238-244.
Lederberg J, Shope RE, Oaks SC. 1992. Emerging Infections: Microbial Threats to Health in
the United States. Washington (DC): National Academy Press.
Leslie GB, Haraprasad V. 1993. Indoor air pollution from combustion sources in developing
countries. Indoor Environment 2:4-13.
Lindvail T. 1992. Radon. Pages 63-76 in Leslie GB, Lunau FW, eds. Indoor Air Pollution:
Problems and Priorities. Cambridge (UK): Cambridge University Press.
Litovitz TL, Schmitz BF, Bailey KM. 1990. 1989 Annual Report of the American Association of
Poison Control Centers National Data Collection System. American Journal of Emergency
Medicine 8: 394-442.
Maddy KT, Edminston S, Richmond D. 1990. Illness, injuries, and deaths from pesticide
exposure in California, 1949-1988. Reviews of Environmental Contamination and Toxicology 114:
57-123.
Mann E. 1991. LA's Lethal Air: New Strategies for Policy, Organizing & Action. Los Angeles
(CA): Labor/Community Strategy Center.
Marshall E. 1997. African malaria studies draw attention. Science 276: 275-299.
McGinnis J, Forge W. 1993. Actual causes of death in the United States. Journal of the
American Medical Association 270: 2207-2212.
McMichael AJ. 1993. Planetary Overload: Global Environmental Change and the Health of the
Human Species. Cambridge (UK): Cambridge University Press.
Mertens TE, Low-Beer D. 1996. HIV and AIDS: Where is the epidemic going? Bulletin of the
World Health Organization 74: 121-129.
Metz JJ. 1991. A reassessment of the causes and severity of Nepal's environmental crisis.
World Development 19: 805-820.
Monath TP. 1994. The risk to developed and developing countries. Proceedings of the National
Academy of Sciences of the United States of America 91: 2395-2400.
Morse, SS. 1997. The public health threat of emerging viral disease. American Society for
Nutritional Sciences 127 (Supplement): 951S-957S.
Mueller D. 1993. AIDS in Thailand: Features of the epidemic in an Asian country with high
incidence of HIV infection. AIDS-Forschung 8: 583-592.
Murray CJL, Lopez AD. 1996. The Global Burden of Disease. Geneva: World Health
Organization.
Myers N. 1993. Environmental refugees in a globally warmed world. BioScience 43: 752-761.
Najera JA, Liese BH, Hammer J. 1992. Malaria: New patterns and perspectives. Washington
(DC): The World Bank. Technical paper no. 183.
[NAS] National Academy of Sciences. 1987. Regulating Pesticides in Food. Washington (DC):
National Academy Press.
Nash L. 1993. Water quality and health. Pages 25-39 in Gleick P, ed. Water in Crisis: A Guide
to the World's Fresh Water Resources. Oxford (UK): Oxford University Press.
Newton LH, Dillingham CK. 1994. Classic Cases in Environmental Ethics. Belmont (CA):
Wadsworth Publishing Co.
[NGS] National Geographic Society. 1995. Water: A Story of Hope. Washington (DC): National
Geographic Society.
[OECD] Organisation for Economic Co-operation and Development. 1985. The State of the
Environment 1985. Paris: Organisation for Economic Co-Operation and Development.
Olliaro P, Catrani J, With D. 1996. Malaria, the submerged disease. Journal of the American
Medical Association 275: 230-233.
Pimentel D. 1995. Protecting crops. Pages 49-66 in Olsen WC, ed. The Literature of Crop
Science. Ithaca (NY): Cornell University Press.
Pimentel D, Bashore T. 1998. Environmental and economic issues associated with pesticide use.
Pages 8-14 in Book of Abstracts, International Conference on Pesticide Use in Developing
Countries: Impact on Health and Environment; 23-28 Feb 1998; San Jose, Costa Rica. San
Jose Universidad Nacional.
Pimentel D, Pimentel M. 1996. Food, Energy and Society. Niwot (CO): University Press of
Colorado.
Platt AE. 1996. Infecting Ourselves: How Environmental and Social Disruptions Trigger
Disease. Washington (DC): Worldwatch Institute.
[PRB] Population Reference Bureau. 1996. World Population Data Sheet. Washington (DC):
Population Reference Bureau.
Real, LA. 1996. Sustainability and the ecology of infectious diseases. BioScience 46: 88-97.
Renner R. 1995. When is lead a health risk? Environmental Science & Technology 29: 256-261.
Repetto R, Baliga SS. 1996. Pesticides and the Immune System: The Public Health Risks.
Washington (DC): World Resources Institute.
Schultz S. 1997. It's time to shield your skin: Summer sun brings skin cancer worries to
forefront. The Ithaca Journal 23 May 1997: SA.
Seager J. 1995. The New State of the Earth Atlas. New York: Simon & Shuster.
Shiklomanov IA. 1993. World fresh water resources. Pages 13-24 in Gleick P, ed. Water in
Crisis: A Guide to the World's Fresh Water Resources. Oxford (UK): Oxford University Press.
Spielman A, Telford SR, Pollack RJ. 1993. The origins and course of the present outbreak of
Lyme disease. Pages 83-98 in Ginsberg HS. ed. Ecology and Environmental Management of
Lyme Disease. New Brunswick (NJ): Rutgers University Press.
Stephenson LS. 1994. Helminth parasites: A major factor in malnutrition. World Health Forum
15: 169-172.
Stratton EM, Ricketts MN, Gully PR. 1997. The epidemiology of Creutzfeldt-Jakob disease in
Canada: A review of mortality data. Emerging Infectious Diseases 3: 1.
Suguti S, Tongu Y. lnatomi S, Pradhan HD. 1985. A survey on human parasite infections in
Nepal. Japanese Journal of Parasitology 34: 285-292.
Todd ECD. 1996. Worldwide surveillance of food-borne disease. Journal of Food Protection 1:
82-92.
Travis J. 1997. Hitting malaria parasites early and hard. Science News 151 (2): 23.
[UKDE] United Kingdom Department of the Environment. 1996. Expert panel on air quality
standards: Benzene. London (UK): United Kingdom Department of the Environment.
[USBC] US Bureau of the Census. 1987. Statistical Abstract of the United States 1987.
107th ed. Washington (DC): US Government Printing Office.
· 1996. Statistical Abstract of the United States 1996. 116th ed. Washington (DC): US
Government Printing Office.
[USC] US Congress. 1993. The Tuberculosis Epidemic. Vol. KF 27 E553 1993n. Washington
(DC): United States Congress, House Committee on Energy and Commerce, Subcommittee on
Health and Environment.
Weiner BP, Worth RM. 1972. Insecticides: Household use and respiratory impairment. Pages
149-151. Adverse Effects of Common Environmental Pollutants. New York: MSS Information
Corporation.
[WHO] World Health Organization. 1990. Public Health Impact of Pesticides in Agriculture.
Geneva: World Health Organization.
· 1992. Our planet, our health: Report of the WHO commission on health and environment.
Geneva: World Health Organization.
· 1993a. Asthma. Weekly Epidemiological Record (5 March): 68-69.
· 1993b. WHO plans renewed attack on animal disease that threatens millions of people.
Geneva: World Health Organization, Press Release No. 68.
· 1993c. World malaria situation. Weekly Epidemiological Record 68 (20 August): 245-252·
· 1994. Cancer. Weekly Epidemiological Record 69 (15 April): 107-108.
. 1995. Bridging the Gaps. Geneva: World Health Organization.
· 1996a. AIDS: Global data. Weekly Epidemiological Record 71 (5 July): 205-2O7.
. 1996b. Human plague. Weekly Epidemiological Record 71 (31 May): 165-168.
. 1996c. Investing in Health Research and Development. Geneva: World Health Organization.
· 1996d. Russian Federation. Weekly Epidemiological Record 71 (16 August): 245-25O.
. 1996e. World food summit: Micronutrient malnutrition -- half of the world's population
affected. Geneva: World Health Organization. Press Release No. 78.
. 1996f World Health Report 1996. Geneva: World Health Organization.
· 1996g. World malaria situation in 1993. Weekly Epidemiological Record 71 (19 January): 1820.
· 1996h. World malaria situation in 1993. Weekly Epidemiological Record 71 (9 February): 4144.
. 1997a. H1V/AIDS: The global epidemic, December 1996. Weekly Epidemiological Record 72
(24 January): 17-21.
. 1997b. Brucellosis. World Health Organization Fact Sheet 173 (July): 1-3.
[WHO/UNEP] World Health Organization and the United Nations Environment Program. 1993.
Urban air pollution in megacities of the world. Geneva: World Health Organization and the
United Nations Environment Program.
Wilken E. 1995. Urbanization spreading. Pages 100-101 in Brown LR, Lenssen N, Kane H, eds.
Vital Signs: The Trends that are Shaping our Future. London: W. W. Norton.
World Bank. 1992. China: Long-term Issues and Options in the Health Transition. Washington
(DC): The World Bank
[WRI] World Resources Institute. 1994. World Resources 1994-95. Washington (DC): World
Resources Institute.
Zimmerman T, Lawrence SV, Palmer B. 1996. China takes a deep breath. US News & World
Report 121(10): 36-39.