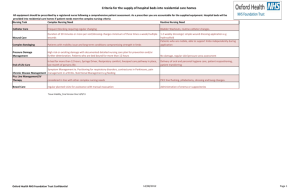
List of 2014 projects
advertisement

QNI Fund for Innovation and Leadership 2014 1. Maintain the health of clients living in a residential home through a DN liaison Nurse Deborah Higgins DN Team leader North Wales The aim of this project is to integrate a trained nurse into the District Nursing team to support 3 residential care homes to provide a proactive rather than reactive nursing service. Currently 9% of District Nursing time is taken up by these 3 homes. The 5 areas the pilot will focus on are: Advice and support to clients and carers Tissue Viability- Wound care, pressure area care, leg ulceration Diabetic Care, Catheter Care Phlebotomy (blood tests) These were identified as the main reason the homes were receiving District Nursing input. The staff within the residential home setting are not trained nurses. The liaison nurse would provide and facilitate training and development for the staff within the safe limitations of the untrained role. The aim being to empower the staff to enable them to provide appropriate care and support to their clients. It is hoped that this proactive service will Reduce unplanned visits to the District Nursing service. Reduce referrals to other members of the MDT including G.P practices (ripple effect). Reduce the need to move clients to nursing homes from the residential setting Reduce the incidence of blocked catheters Reduce tissue viability referrals – e.g. Skin tears, weeping legs, accidental injuries. Enhance diabetes and nutritional support for residents 2.Tailoring care for patients with vascular disease within a General Practice setting Esme Elliott Practice Nurse Newcastle-Upon-Tyne This project will provide a tailored service to 714 patients within this general practice who have been diagnosed with vascular disease. Currently there is no differentiation in the nursing input provided to each patient. This project will develop a tool that will signpost patients more appropriately depending on the complexity of their condition and their need for nursing input. This will enable increased nursing time to be dedicated to the most vulnerable patients with the highest need, and empower those with less complex problems to take more control of their condition self-manage. Outcome measures to assess the success of the project will include: Increased patient uptake of the new service Improved adherence to medication Reduction in unplanned hospital admissions and A&E attendances 3.Catheter Champions Michelle Payne Continence Specialist nurse Middlesbrough This project aims to pilot the use of catheter champions within District Nursing teams. Each patient with a long term in dwelling catheter known to the District Nursing team will be offered an in depth assessment of their continence needs with a champion. The use of indwelling catheters raises the risk of infection by 5% for each 24 hours that a catheter remains in situ. Many patients will not know why they were catheterised and have accepted the situation, this project has the potential to have significant impact on quality of life for patients in the community with long term catheters,. It is the aim of this project to empower patients to understand their continence needs and the options available to them. Some patients may be able to have an alternative to an in dwelling catheter, such as flip-flow valves (a valve used instead of a free drainage leg bag with a catheter) or intermittent selfcatheterisation. Where no alternative is possible patients and partners/carers will be educated about catheter acquired urinary tract infections (CAUTI’s) and a care plan developed to prevent or reduce the incidence of these. 4. Behaviour Management Programme at Key stage 1 Julie Bulmer School Nurse Team Leader Locala The aim of the project is to develop a pathway that enhances the skills and knowledge of school nurses enabling them to support parents and school staff to manage children with behavioural issues in key stage 1(children aged between 4 and 7). The school health team recognised that due to lack of expertise within the team there was currently a gap in the service they provided around behaviour management, this coupled with a growing number of referrals from parents, schools and other health professionals led to this proposal. It is recognised that challenging behaviour has a significant negative impact on the child’s health, well-being and attainment. In order to improve the outcomes for these young children a behaviour assessment tool and a digital training package will be developed to support the delivery of this approach. It is hoped that this intervention will improve the behaviour, emotional health and educational attainment of the child. Also improve parenting skills and the relationship between the parent and child. 5. Milk to Meals Ros Ratcliffe Health Visitor Southampton The primary aim of the project is to address the issue of delayed weaning within a defined location in the city of Southampton. One of the most common problems with infant and toddler nutrition in this area is the poor diet of a number of Asian and Afghani children caused by their excessive intake of milk. Excessive milk intake has several effects on infants and toddlers health, including obesity, anaemia, dental caries and various long term effects such as the development of diabetes and cardiovascular disease. There can also be a delay in the development of speech due to the lack of adequate chewing in the infant/toddler’s life. Whilst reducing the milk intake it is intended that the team promotes the introduction of a healthy solid food diet through the delivery of Café sessions for those parents who are struggling with the child’s diet and feeding regime. Meals will be cooked during the session and the parents will then be encouraged to eat with their children. 6. Assistive Technology Rachel Daly Quality in Care Team Lead Aylesbury The aim of this project is to improve the skills of care workers and care home providers to prevent and manage falls by the use of assistive technologies (AT). Care home staff will receive support and training to enhance their knowledge and skills on the causative factors of falls and how the use of telecare and telehealth, in an appropriate care home environment can prevent a person from falling and support individuals who do fall to receive speedy assistance when required and maintain their independence as safely as possible. Access to an assistive technology laboratory will be made available where they will gain an improved understanding of which pieces of equipment would best support particular people. Service users and their families will also be encouraged attend sessions if they wish. It is hoped that this approach will reduce the number of falls in a care home environment, change the culture in care home environments from dependence to independence and that care homes adopt a proactive approach to new ways of working. 7. Healthcare Training for Carers of Patients on End of Life Pathway Kirsty Marshall Community Nursing Development lead Lancashire This project aims to enable carers to deliver basic healthcare care to the person they care for who is nearing the end of life. Carers are often providing a number of health care activities to the person nearing the end of life within a home environment and without any training and support. This can be a daunting experience at a time of emotional distress and can impact on the carers own well-being. End of life care is an integral aspect of health care provision in the community, to those living with and dying from advanced or progressive and life-threatening conditions. The experience of the patient reaching the end of life and their carers is significant in terms of emotional, psychological and physical impact. A training and support programme will be developed in partnership with carers, equipping them with the practical skills and knowledge to feel confident to look after their loved ones at home. It is hoped that this project will support both the patient and carer to achieve their wishes with regard to dying at home if this is their preferred place of care. 8. Community At Risk Tool (CART) Project Sadie Campbell Lead Nurse Northern Ireland The key aim of this project is develop a tool to predict frailty in older people living at home. Once identified those at highest risk will be offered tailored support to maintain their independence for as long as possible in their own home. Case managers play a key role in proactive management of long term conditions such as COPD, Heart Failure and Diabetes. They are, therefore, best placed to identify and manage frailty in the older community population with the help of a predictive risk screening tool. It is hoped through the use of this tool to decrease hospital admissions for frail older people and reduce admissions to nursing homes. It will also proactively involve older frail people in remaining independent in their own home for as long as possible. 9.Exzema Expert Nicola Broad Community Dermatology Speciaist Nurse Wigan The aim of this project is to provide easily accessible, timely, evidence based expert information, advice and treatment to children with eczema. It is hoped that early intervention will reduce the severity of the condition, increased susceptibility to allergy, reduce the need for antibiotics and improve both the patient and their family’s quality of life. In addition it is hoped to improve parental knowledge and thus empower them to self-manage their child’s skin condition, in turn reducing parental anxiety and repeat stressful trips to their GP and Out of Hours services. An ‘Eczema Expert’ pack has been developed which will be trialled at a local walk-in centre. The pack is a 3 in 1 intervention that plans to address patient and carer education whilst focusing on trigger avoidance, maintenance and repair of skin barrier function and reduction of inflammation of the skin.