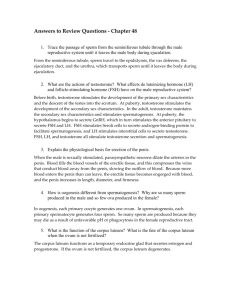
THE REPRODUCTIVE SYSTEMS
advertisement

THE REPRODUCTIVE SYSTEMS Define reproduction. Reproduction is the process by which genetic material is passed from generation to generation, maintaining the continuation of the species. Identify, then briefly describe, the three groups of reproductive organs according to function. gonads -- The testes and ovaries -- function to produce the gametes (sperm and ova) and to secrete reproductive hormones. ducts -- Ducts transport, receive, and store gametes. They are particularly extensive in the male. accessory glands -- produce materials that support the gametes in the male. In the female the accessory glands are used to provide lubrication for intercourse. A. MALE REPRODUCTIVE SYSTEM 1. SCROTUM Describe the scrotum. The scrotum is a cutaneous outpouching of the abdomen, consisting of loose skin and superficial fascia. It is divided by a vertical septum into right and left compartments, each of which contains a single testis. The scrotum serves as the supporting structure for the testes. What is Dartos’ fascia? The scrotal septum is continuous with the superficial fascia beneath the skin of the scrotum. This fascia contains smooth muscle called Dartos’ fascia. This specialized fascia is responsible for tightening of the scrotal skin, thus playing a role in temperature regulation of the testes. What is the function of the scrotum? The location of the scrotum and the contraction of Dartos’ fascia and skeletal muscle fibers that wrap the testes regulate the temperature of the testicular environment. The production and 347 survival of sperm require a core temperature of 95° F. Because the scrotum is outside the body cavity it can provide this environment. What is the cremaster muscle? In addition to Dartos’ fascia in the superficial fascia of the scrotal wall, each testis has a cremaster muscle, a sling-like band of skeletal muscle derived from the internal abdominal oblique muscle of that side of the body. The muscle comes to wrap the testis as it descends the body wall during development to move out of the abdominal cavity and into the scrotum. Describe the cremaster reflex. Contraction of the cremaster muscles (cremaster reflex) elevates the testes toward the body cavity (and body heat) during exposure to cold and with sexual arousal. Exposure to heat causes the cremaster muscle to relax, allowing the testes to drop away from the body cavity and therefore away from the core body temperature. 2. TESTES Describe the testes as follows: gross anatomy -- The testes (testicles) are paired oval organs that reside within the scrotum. Each testis is 2" long x 1" in diameter. development -- The testes develop on the posterior wall of the body and descend through the inguinal canals, passing through the anterior abdominal wall to enter the scrotum at the end of the 7th month of fetal life. They are partially covered by the tunica vaginalis, an extension of the peritoneum formed during the testicular descent. tunica albuginea/lobules -- Internal to the tunica vaginalis is the dense connective tissue capsule of the testis itself, the tunica albuginea (white coat). Extensions (septa) of the tunica albuginea into the substance of the testis divide it into 200 - 300 smaller compartments called lobules. seminiferous tubules -- Within each lobule are 1 - 3 tightly coiled tubules called the seminiferous tubules. The tubules are lined with spermatogenic cells in various stages of develop348 ment (meiosis). The most immature cells type, the spermatogonium, lies on the outer border of the tubule. a. SPERMATOGENESIS AND SPERMIOGENESIS Describe the process of spermatogenesis and spermiogenesis. Once sexual maturity is reached (puberty), the spermatogonia may enter one of two cell division pathways. Some spermatogonia enter mitosis and simply add new spermatogonia to the seminiferous tubules. Other spermatogonia, in response to appropriate hormonal signals, move away from the basement membrane of the tubule toward the lumen, and enter meiosis to begin the process of spermatogenesis. Once in meiosis, the cell enlarges to become a primary spermatocyte. It then enters the first meiotic division, giving rise to two secondary spermatocytes, each of which now has half the original number of chromosomes. Each secondary spermatocyte enters the second meiotic division, giving rise to two spermatids, each now with the appropriate number of chromosomes (monads) to fertilize an egg. Each spermatid is then partially engulfed within another cell type of the seminiferous tubule, the sustentacular (Sertoli) cell, where it enters the process of spermiogenesis. During this time the spermatid becomes an anatomically mature sperm. In this process, the spermatid sheds its cytoplasm, condenses its DNA into a tight “head” and forms a flagellum, giving rise to the anatomically mature spermatozoon. During this time, the Sertoli cell nourishes and protects the spermatid. After spermiogenesis, the Sertoli cell releases the spermatozoon into the lumen of the seminiferous tubule for transport out of the testis. b. SPERMATOZOA Describe sperm as follows: maturation rate and lifespan -- Spermatozoa released from 349 Sertoli cells are anatomically, but not functionally, mature cells, each with 23 chromosomes that are the male component of fertilization. They mature at the rate of about 300 million/day in sexually active males and, once ejaculated into the female reproductive tract, have a life expectancy of about 48 hours. head and acrosome -- Each sperm is composed of three portions: the head contains the DNA and a dense granule called the acrosome, a package of enzymes that aid the sperm in penetration into the ovum for fertilization. midpiece and tail -- The midpiece contains mitochondria that provide ATP for locomotion. The tail is a typical flagellum that propels the sperm along its way in the female reproductive tract. c. HORMONES OF THE BRAIN-TESTICULAR AXIS Describe the hormones involved in the control of the male reproductive system. Be sure to include the sources of the hormones. Secretions of the anterior pituitary gland, controlled by the hypothalamus, play a major role in the developmental changes in the male reproductive system that occur at puberty and which maintain sexual function in the adult. In response to gonadotropin-releasing factor (Gn-RF) from the hypothalamus, the anterior pituitary gland secretes its two gonadotropins: follicle-stimulating hormone (FSH) and luteinizing hormone (LH) (aka – interstitial cell stimulating hormone). FSH (1) initiates spermatogenesis by stimulating spermatogonia to enter the meiotic pathway, and (2) stimulates Sertoli cells to prepare for the newly formed spermatids and to produce the hormone inhibin. Interstitial endocrinocytes (Leydig cells) are nests of cells located between seminiferous tubules. They respond to LH by secreting testosterone and other male sex steroid hormones (androgens). Testosterone and related androgens have the following functions: (1) stimulate embryonic and fetal development of 350 the male primary sexual characteristics (formation of male sex organs, descent of the testes). (2) Male secondary sexual characteristics that begin to appear at puberty (enlargement of genitalia, increased protein anabolism for musculoskeletal development, formation of coarse body hair, enlargement of larynx. Describe blood testosterone levels during the male lifespan. What is the role of the hormone inhibin in male reproduction? Prior to puberty, blood testosterone levels are low. This testosterone is secreted primarily by the testes, as well as the adrenal cortex. At and after puberty, blood testosterone levels reach a genetically determined level and are maintained at this level until about the age of 50 by negative feedback of testosterone on LH secretion. Blood testosterone levels drop about 1/7 per decade after the age of 50. Even at the age of 80, a gentleman has about 4/7 of the testosterone he had as a teenager. The hormone inhibin secreted by Sertoli cells in response to FSH is involved with the negative feedback control of FSH secretion and the control of the rate of spermatogenesis. Again, rate of spermatogenesis is genetically determined. When it proceeds too slowly, inhibin secretion is inhibited, so that more FSH can be secreted and the rate of sperm formation can increase. 3. DUCTS a. DUCTS OF THE TESTES Describe the following: sperm path out of testis --Sperm and fluid are moved by a pressure gradient created by new sperm from the seminiferous tubules into the straight tubules, one per lobule. Straight lobules open into a network of tubules at the hilus of the posterior testis called the rete testis. From here, sperm and fluid are moved through the efferent ductules into the ductus epididymis. b. EPIDIDYMIS 351 Describe the ductus epididymis following: location -- The highly coiled ductus epididymis is a tubule that lies within a connective sheath, forming the epididymis. This comma-shaped organ lies along the posterior border of each testis. functions -- Functionally, the ductus epididymis is the site of sperm maturation. Non-motile and nonfertile new sperm mature for 10-14 days within the ductus epididymis, during which time they gain motility and become capable of fertilization (once in the presence of seminal fluids). The ductus epididymis also serves as a storage site for sperm and may hold them as long as a month. If they are not expelled by peristalsis into the ductus deferens they are resorbed by the epithelium of the ductus epididymis. c. DUCTUS (VAS) DEFERENS Describe the ductus deferens as follows: origin -- At the tail of the epididymis, the ductus epididymis becomes larger in diameter and straighter. At this point the duct is known as the ductus (vas) deferens. path out of scrotum -- The vas deferens passes superiorly along the posterior border of the epididymis, enters the spermatic cord, and enters the pelvic cavity. The spermatic cord is a composite structure of the male reproductive system that passes superiorly out of the scrotum and into the pelvic cavity through the inguinal canal. In addition, to the vas deferens, it also contains the testicular artery, a plexus of veins that drain the testis, autonomic nerves, lymphatic vessels, and the cremaster muscle. The inguinal canal is an obliquely placed passageway through the anterior abdominal wall just superior and parallel to the medial half of the inguinal ligament. It originates as the deep inguinal ring, a slit-like opening in the transverse abdominis muscle, passes about 2", then terminates as the superficial inguinal ring, a 352 triangular opening in the external abdominal oblique muscle just lateral to the pubic symphysis. path in pelvic cavity -- Once in the pelvic cavity, the vas deferens loops over the side and down the posterior surface of the urinary bladder, ending as a dilated portion called the ampulla, which serves as a second site for sperm storage. function -- Functionally, in addition to sperm storage in the ampulla, the vas deferens conveys sperm by peristalsis from the ductus epididymis toward the urethra during ejaculation. d. e. EJACULATORY DUCTS URETHRA Describe the following: ejaculatory ducts -- Lying posterior to the urinary bladder are the ejaculatory ducts. Each is formed by the union of the ampulla of the vas deferens with the duct of the seminal vesicle of that side. The ejaculatory ducts receive sperm from the vas deferens and eject them into the prostatic portion of the urethra just before ejaculation (a process called emission). male urethra -- The male urethra is the terminal duct of the reproductive and urinary systems, serving as a passageway for both sperm and urine. It is divided into three parts. The prostatic urethra (1 inch) passes from the urinary bladder directly through the substance of the prostate gland, receiving its secretions from many ducts as it passes through the gland. The membranous urethra (0.5 inches) passes from the edge of the prostate gland through the muscular pelvic (urogenital) diaphragm, which forms the external urethral sphincter, then passes into the penis. The penile urethra (6 inches) passes into the corpus spongiosum of the penis and opens to the outside at the external urethral orifice. 4. ACCESSORY SEX GLANDS 353 Describe the accessory sex glands of the male. While the testes create the cellular portion of the semen, the accessory sex glands of the male produce most of the liquid portion of the semen. Name and then describe the accessory sex glands of the male. The accessory sex glands of the male are the: 1. prostate gland 2. seminal vesicles (2) 3. bulbourethral glands (2) Describe the prostate gland and its secretions. The prostate gland is a single chestnut-sized structure lying inferior to the urinary bladder surrounding the origin of the urethra. It secretes a slightly acidic viscous fluid rich in citric acid, some clotting enzymes, and fibrolysin/serine protease/PSA . Describe the seminal vesicles and their secretions. The seminal vesicles lie posterior to the base of the urinary bladder, in front of the rectum. They secrete an alkaline, viscous fluid rich in fructose, prostaglandins, and fibrinogen/prosemenogelin. Describe the bulbourethral glands and their secretions. The bulbourethral glands are about the size of peas and are located on either side of the membranous urethra within the pelvic diaphragm. They secrete alkaline, mucous-rich fluid called, pre-ejaculatory fluid. List and then describe the function of each of the three major components of the seminal vesicles fluid (1,2,3) and prostatic fluid (4,5,6). 1. 2. fructose - used by sperm for ATP production prostaglandins -- promote sperm motility and stimulate muscular contractions of the female tract 3. proseminogelin -- used to coagulate semen after ejaculation 4. citric acid -- used for sperm motility 5. clotting enzymes-converts prosemenogelin to semenogelin or fibrinogen to fibrin 6. serine protease/PSA prostate specific antigen//fibrinolysin -- liquefies clotted semen after several minutes in the female tract 354 What are the two functions of pre-ejaculatory fluid? 1. 2. 5. neutralize residual acidity within the urethra lubricate the urethra to facilitate passage of sperm SEMEN Describe semen by discussing it components, pH, average volume, average number of sperm, functions, and fate. Semen (seminal fluid) is a mixture of sperm and accessory gland secretions. Semen has a pH of 7.2 - 7.6. The average volume of semen is 2.5 - 5 ml/ejaculate. An average ejaculate contains 50 - 100 million sperm/ml. (<20 million is considered male infertility) Semen functions in the transportation and nourishment of sperm and in neutralizing the acidity of the male urethra and the female vagina to promote sperm viability. Once ejaculated into the vagina, semen coagulates, then liquefies 5 - 20 minutes later, liberating the sperm for their journey up the female reproductive tract. 6. PENIS Describe the penis as follows: functions -- The penis is used to introduce sperm into the vagina and as an excretory organ for the urinary system. portions -- The penis consists of three portions: the root, the body (corpus), and the glans (head). What is the root of the penis? The root of the penis is the portion attached to the body wall. It consists of the bulb of the penis, the expanded base of erectile tissue known as the corpus spongiosum, and the crura, connective tissues which attach the underside of the penis to the pelvic diaphragm. The bulb and crura are enclosed within two muscles of the pelvic diaphragm, the bulbocavernosus and the ischiocavernosus muscles. What is the body of the penis? 355 The body of the penis is composed of cylindrical masses of erectile tissues, each bound by dense fibrous connective tissue called the tunica albuginea and each permeated by blood sinuses. Name and describe the erectile tissues? The two dorsolateral masses are called the corpora cavernosa and the smaller midventral mass is the corpus spongiosum, which contains the penile urethra and forms the head of the penis. Describe the head of the penis. The distal enlarged end of the penis, the glans penis, also known as the head of the penis, is formed by the distal expanded portion of the corpus spongiosum. Covering the glans penis is the prepuce (foreskin). erection -- With sexual stimulation, the arteries supplying the penis vasodilate and large quantities of blood enter the erectile tissues. As these spaces expand, the penile veins are compressed so that an erection is formed. The penis returns to it flaccid state when sexual stimulation ends. The penile arteries vasoconstrict, allowing the blood to drain from the erectile tissues. B. FEMALE REPRODUCTIVE ORGANS List the organs of the female reproductive system. The organs of the reproductive system include the: 2 ovaries 2 uterine (fallopian) tubes (oviducts) uterus vagina external genitalia In addition, the mammary glands are often grouped into this system 1. OVARIES Describe the ovaries as follows: gross anatomy -- The ovaries, or female gonads, are paired organs 356 about the size and shape of an almond. They develop and descend like the testes, but stop their descent at about the level of the pelvic brim. Each ovary comes to lie in the upper pelvic cavity, one on each side of the uterus. They are held in place by a series of ligaments (folds of the peritoneum) that anchor them to the uterine tubes and the uterus. 4 main parts -- Each ovary consists of four main parts: germinal epithelium --The germinal epithelium is a layer of epithelium that covers the outer surface of the ovary. It got its name because these cells were once thought to be the eggs (hence the name germinal.) tunica albuginea - The tunica albuginea is a capsule of dense connective tissue lying just deep to the germinal epithelium. It is homologous to the tunica albuginea of the testes. stroma -- The stroma of the ovary is a region of connective tissue deep to the tunica albuginea that is subdivided into a cortex and a medulla. The cortex contains the developing ova, while the medulla houses the ovarian blood supply. ovarian follicles -- eggs (ova) in various stages of development a. OÖGENESIS The formation of haploid ova in the ovary involves several stages of ovarian follicle development. Describe these stages and structures of oögenesis and the ovarian cycle. Ovarian follicles are immature oöcytes surrounded by support cells called follicular cells. During the course of a monthly ovarian cycle, some of these immature follicles develop to the point of ovulation. Primordial follicles consist of a primary oöcyte, which has been arrested in meiosis I since about the 6th prenatal month of the female baby’s life. A single layer of flattened follicular cells surrounds the oöcyte. Each, month, some primordial follicles develop into primary follicles. The primary oöcyte begins to complete its first 357 meiotic division and the surrounding follicular cells enter mitosis and begin to secrete estrogen. The primary follicle becomes a secondary follicle when the ovum is a secondary oöcyte arrested in meiosis II and the follicular cells have formed and antrum (lake) of fluid rich in estrogen. The tertiary (Graafian) follicle contains the secondary oöcyte surrounded by a very large antrum and a wall of follicular cells that continue to secrete estrogen. This is just before ovulation. At ovulation, the secondary oöcyte and some attached follicular cells are ruptured from the tertiary follicle out of the ovary and into the peritoneal cavity, leaving behind the remainder of the follicular cells as the corpus luteum. The corpus luteum is a temporary endocrine organ (living for only 12 - 13 days post-ovulation) left behind in the ovary after ovulation. The luteal cells secrete estrogen and progesterone. After 12 - 13 days the corpus luteum dies (if pregnancy has not occurred). This leaves a bit of scar tissue within the ovary called the corpus albicans. How is oögenesis different from spermatogenesis? Oögenesis is similar to spermatogenesis in the male in that meiosis is required to produce a secondary oöcyte for fertilization. It is unlike the male in that oögonia lose the ability to divide by mitosis during fetal life. During fetal life, oögonia increase their numbers to about 7 million, and then lose their mitotic ability. They then either enter meiosis or die. By puberty, only about 40,000 - 60,000 primary oöcytes remain in the ovaries, each arrested in meiosis I and waiting for the appropriate hormonal signal to continue the meiotic process. What is the role of the following hormones in oögenesis? Gn-RF -- Like the male, at puberty female Gn-RF stimulates the secretion of FSH and LH from the anterior pituitary gland. These gonadotropins then activate the ovaries to enter the ovarian cycle. This process occurs monthly. 358 FSH -- Each month FSH stimulates primary oöcytes (up to 50 or so), living within primordial follicles, to resume meiosis and become secondary oöcytes. FSH also stimulates the follicular cells to begin mitosis and to begin secreting estrogen. All but one of the developing follicles dies after being activated by FSH. The one that survives becomes a secondary, then a tertiary follicle, containing a secondary oöcyte that arrests in meiosis II. LH -- In response to the rising blood estrogen levels, LH is secreted. It causes ovulation to occur. The secondary oöcyte, now liberated, will continue and finish meiosis only if it is fertilized by a sperm cell. 2. UTERINE (FALLOPIAN) TUBES Describe the oviducts as follows: gross anatomy -- The two oviducts (uterine or Fallopian tubes) are about 4 inches long, extending laterally from the uterus to the ovary of that side. Each tube is subdivided into four sections. Name and describe each of these subdivisions. The open, funnel-shaped distal end of an oviduct is the infundibulum. It ends in a fringe of finger-like processes called the fimbriae that lie adjacent to the ovary. The ampulla of the oviduct is the widest portion, forming the next two-thirds of its length. The isthmus is the narrowed neck region of the uterine tube where it attaches to the uterus. histology -- The oviduct is lined with a ciliated mucosa that aids in the transport of the ovum down the tube, and secretory cells that provide nutrition for the passing ovum. In addition, there is a muscularis layer that, through peristaltic actions, aids sperm movement up the oviduct and ovum movement down the oviduct. function -- At ovulation, the released ovum usually sticks to the inner surface of the fimbriae and is swept through the oviduct by ciliary and peristaltic movements. Successful fertilization, meaning one that results in uterine implantation, occurs in the ampulla within 24 hours of ovulation. 3. UTERUS 359 Describe the uterus as follows: gross anatomy -- The uterus is between the urinary bladder anteriorly and the rectum posteriorly and is held in position by ligaments formed by folds of the peritoneum. Normally, it is flexed (bent) between its body and cervix, so that the body projects anteriorly and superiorly over the urinary bladder (anteverted). divisions -- Anatomically the uterus is divided into several parts. The fundus is the dome-shaped portion above the openings of the oviducts and the body (corpus) is the major, tapering central portion. The cervix is the narrow inferior portion opening into the vagina. It is separated from the body by the isthmus of the uterus. The interior of the uterus is the uterine cavity that opens into the cervical canal. cervical mucous -- The cervical mucosa secretes cervical mucous, a material that becomes less viscous and more alkaline during the time of ovulation, thus facilitating fertilization. At this time, it is very receptive to sperm and provides nourishment and protection for them. At other times it is thicker and more acidic. functions -- The uterus (womb) functions as the: 1. site of menstruation 2. implantation and development of the embryo/fetus during gestation 3. labor perimetrium -- The outermost layer of the uterus, the perimetrium, is the visceral peritoneum that wraps the uterus and holds it in place. Laterally, it folds over itself to form the broad ligament. peritoneal pouches -- Anteriorly, the perimetrium reflects over the bladder to form the vesicouterine pouch. Posteriorly, it reflects over the rectum, forming the rectouterine pouch. The rectouterine pouch is the lowest point in the female pelvis. myometrium -- The myometrium, the middle layer, forms the bulk of the uterine wall. It is formed of three layers of smooth muscle that are responsible for labor and delivery. endometrium -- The endometrium, the inner mucosal layer, consists of two parts: 360 1. 2. The stratum basalis is the deep permanent mitotic layer. The stratum functionalis is the superficial portion that is sloughed off with each menstrual cycle. blood supply -- Blood is supplied to the uterus by the uterine arteries, branches from the internal iliac arteries. Ultimately, there are spiral arterioles that directly supply the stratum functionalis. This is unlike all other epithelia since no other has a direct blood supply. 4. VAGINA Describe the vagina as follows: function -- The vagina, passing from the cervix to the exterior of the body, serves as a passageway for menstrual flow and childbirth and the copulatory organ of the female, receiving semen from the male during intercourse. gross anatomy -- The vagina is a tubular, fibromuscular organ lined with mucosa. It measures about 4 inches in length in the unstimulated state. It lies between the urinary bladder and the rectum. A recess called the fornix surrounds the vagina at its attachment to the cervix. At the lower end, the introitus (vaginal orifice), there may be a thin fold of mucous membrane called the hymen. It forms a border around the orifice and partially closes it. mucosa -- The vaginal mucosa is stratified squamous and is thrown into folds called rugae. The muscularis layer is smooth muscle that can stretch considerably, lengthening up to a total of 7 inches or so, to accommodate a penis during intercourse or to allow passage of a fetus. role of glycogen -- The vaginal mucosa stores glycogen, a food source for the normal bacterial flora that live in the vagina. These bacteria decompose the glycogen and in doing so, create an acidic vaginal environment. The naturally acidic vaginal environment retards unwanted microbial growth in the vagina (yeast, for example). This acidity is also harmful to sperm, hence the alkalinizing influence of the semen. 5. VULVA Describe the following: 361 vulva -- The term vulva (also known as the pudendum) is a collective term that refers to the external genitalia of the female. It includes the: mons pubis, labia majora (2), labia minora (2), clitoris, and vestibule. mons pubis -- The mons pubis is anterior to the vaginal and urethral openings. It is an elevation of adipose tissue covered by pubic hair that serves to cushion the pubic symphysis during intercourse. It is homologous to the mons pubis of the male. labia majora -- The labia majora are two folds of skin extending from the mons pubis inferiorly to the anus posteriorly. They contain adipose tissue, sebaceous and sudoriferous glands, and are covered by pubic hair. The labia majora are homologous to the scrotum of the male. labia minora -- The labia minora are two longitudinal folds of mucosa just medial to the labia majora. They extend from the clitoris to just anterior to the anus, where they fuse. They have no hair or fat, but many sebaceous glands. They are homologous to the urethral folds of the male. clitoris -- The clitoris is a small cylindrical mass of erectile tissue and sensory nerves located at the anterior junction of the labia minora. A small fold of skin called the prepuce (foreskin) covers it. The clitoris is homologous to the penis of the male. vestibule -- The vestibule is the cleft found between the labia minora. It contains the urethral orifice anteriorly and the vaginal orifice posteriorly, and the openings of a number of small glands. The bulb of the vestibule, similar to the bulb of the penis, consists of two masses of erectile tissue just deep to the labia on either side of the vaginal orifice. Like the male, they become engorged with blood during sexual arousal. glands of the vestibule -- Opening into the vestibule are the greater and lesser vestibular glands. They provide most of the lubrication for intercourse. There are no vaginal glands for this purpose. These glands are homologous to the prostate gland and the seminal vesicles of the male. 6. PERINEUM What is the perineum? 362 The perineum is the diamond-shaped area between the thighs and the buttocks of males and females that contain the external genitalia and the anus. Describe the boundaries of the urogenital triangle and the anal triangle. It is subdivided into the urogenital triangle and the anal triangle by imaginary lines drawn between the symphysis pubis, the two ischial tuberosities, and the coccyx, with a transverse line between the two ischial tuberosities. Why is the perineum important? The dimensions of the perineum are important considerations regarding childbirth because it defines the size of the birth canal. 7. MAMMARY GLANDS Describe the mammary glands as follows: location --The mammary glands (breasts) are modified sudoriferous glands that produce milk. Each gland lies over the pectoralis major and serratus anterior muscles and is attached to them by a layer of connective tissue. lobes and lobules -- Internally, each gland consists of 15 - 20 lobes separated by adipose tissue. While breast size is determined by the amount of adipose tissue present, it has nothing to do with the ability to produce milk. Each lobe is subdivided into several smaller lobules. ducts -- Each lobule consists of clusters of milk-producing cells that are drained by secondary tubules to mammary ducts to lactiferous sinuses to lactiferous ducts that open at the nipple. nipple -- The nipple is the pigmented projection of the mammary gland through which milk is expressed to the outside. The nipple is surrounded by the pigmented areola. This area is rich in tactile receptors. development -- At birth, the mammary glands are undeveloped. At puberty, under the influence of estrogen and progesterone, the duct system matures, fat deposition begins, and the areolar area becomes pigmented. Development into a milk363 secreting organ is dependent upon the hormones of pregnancy. C. FEMALE REPRODUCTIVE CYCLE The female reproductive cycle , a cyclical sequence of changes in the ovaries and uterus, requires about one month and involves both oögenesis and preparation of the uterus to receive a fertilized ovum. It is divided into two portions, each of which is hormonally controlled. Give a brief description of the ovarian and uterine cycle. The ovarian cycle is a series of events associated with the continued maturation of an ovum, resulting in a single secondary oöcyte arrested in meiosis II that is ovulated. FSH and LH control the cycle. The uterine (menstrual) cycle is a series of changes in the stratum functionalis of the uterus to prepare for implantation of a fertilized ovum. The cycle is controlled by estrogen and progesterone. 1. HORMONAL REGULATION Describe the role of the following hormones in female reproduction: Gn-RF -- The uterine and ovarian cycles are ultimately controlled by Gn-RF from the hypothalamus. Like the male, Gn-RF secretion begins in puberty and works to stimulate the secretion of FSH and LH from the anterior pituitary gland. FSH -- FSH is secreted in response to Gn-RF when blood estrogen levels are low. It stimulates some primordial follicles (primary oöcyte and surrounding follicular cells) each cycle to begin the maturation process towards the tertiary follicle stage. LH -- LH, secreted when blood estrogen levels are high, stimulates final maturation of the remaining tertiary follicle, ovulation, and formation of the corpus luteum. The corpus luteum will secrete estrogen, progesterone, inhibin, and relaxin. estrogen -- Estrogen has 3 main functions: 1. promotes development of the female secondary sex characteristics. 2. helps control fluid and electrolyte balance; and 3. increases protein anabolism progesterone -- Progesterone, secreted by the corpus luteum, works with estrogen to prepare the endometrium for implantation and the mammary glands for milk production. 364 inhibin -- Inhibin, secreted by the corpus luteum, inhibits secretion of Gn-RF and FSH, and to a lesser extent, secretion of LH. It is likely to be important in the decreasing secretion of FSH and LH towards the end of each cycle. relaxin -- Relaxin, secreted by the corpus luteum during regular cycles and by the placenta during the last trimester of pregnancy, relaxes the pubic symphysis and helps to dilate the cervix. Answer the following questions concerning estrogen and its controlling effects on Gn-RF and the gonadotropins. Which cells secrete estrogen? Estrogen is secreted by follicular cells prior to ovulation and by the corpus luteum after ovulation. What is the effect of high blood levels of estrogen? High levels of estrogen allow Gn-RF secretion and prime the anterior pituitary gland to secrete LH, which stimulate ovulation and formation of the corpus luteum. What is the effect of low blood levels of estrogen? Low levels of estrogen allow Gn-RF secretion and prime the anterior pituitary gland to secrete FSH, which stimulates follicular development at the beginning of a new cycle. What is the effect of moderate blood levels of estrogen? Moderate levels of estrogen inhibit Gn-RF secretion of FSH and LH. 2. PHASES OF THE FEMALE REPRODUCTIVE CYCLE Describe the normal female reproductive cycle in terms of its average duration and the names of its four major phases. The female reproductive cycle is on average 28 days long. The cycle is divided into four major phases: menstrual, preovulatory, ovulation, and postovulatory. Describe the menstrual phase. The menstrual phase (menstruation, menses) lasts for roughly the first five days of the cycle. Day 1 of menstrual bleeding is 365 considered to be day 1 of the next cycle. What does menstrual flow contain? Menstrual flow consists of 50 - 150 ml of blood, tissue fluid, and endometrial cells derived from the breakdown of the stratum functionalis at the end of the last cycle. What initiates the menstrual phase? In response to the declining levels of estrogen and progesterone at the end of the last cycle, the spiral arterioles of the uterus undergo roughly 6 hour alternating periods of intense vasoconstriction and vasodilation. As a result the cells of the stratum functionalis become ischemic, die, and break off from the underlying stratum basalis. It is this time that estrogen and progesterone are at their lowest, and FSH secretion is stimulated. FSH, in turn, stimulates primordial follicles to develop and in doing so, to secrete new estrogen so that blood estrogen levels begin to rise. a. b. c. d. MENSTRUAL PHASE (MENSTRUATION) PREOVULATORY PHASE OVULATION POSTOVULATORY PHASE Describe the preovulatory phase of the female reproductive cycle. When does ovulation occur? The preovulatory (proliferative) phase is the period from the end of menstruation until ovulation, days 6 - 14 of the average cycle. This phase is the most variable among women. Describe the hormonal changes of this time. Increasing blood estrogen (from developing follicles) inhibits FSH secretion and stimulates the stratum basalis of the uterus to undergo rapid mitotic divisions, so that the stratum functionalis is rebuilt. At the end of the preovulatory phase, blood estrogen level is at its highest. This stimulates the release of LH that will, in turn, stimulate ovulation of the new tertiary follicle. Describe ovulation. Ovulation, the rupture of the tertiary follicle from the ovary into the peritoneal cavity occurs on day 14 of the 28 day 366 cycle. The secondary oöcyte, with its attached follicular cells (corona radiata), moves into the oviduct. Within the ovary, the follicular cells left behind collapse upon themselves to form the corpus luteum, a temporary endocrine organ that stimulates estrogen, progesterone, inhibin, and relaxin for 12 - 13 days (postovulatory phase) Describe the postovulatory phase of the reproductive cycle. The postovulatory (secretory) phase is day 15 - 28, the most constant phase among females. In most cases, regardless of ovulation day, it lasts only 12 - 14 days. Describe the hormonal changes in this phase. In response, to increasing estrogen and progesterone from the corpus luteum, the stratum functionalis differentiates in anticipation of a fertilized ovum that will need to implant in the uterine wall. What are the three major changes that occur? One major change is increased endometrial gland activity resulting in increased glycogen deposition in the stratum functionalis. This glycogen will be used as an initial food source for the conceptus after implantation. A second major change is increased vascularization via the spiral arterioles. This increases nutrient and oxygen delivery to the stratum functionalis and aids in water retention, the third alteration. These preparatory changes reach their maximum about 7 days after ovulation, corresponding to the arrival of the fertilized ovum from the oviduct into the uterus. What happens if fertilization and implantation do not occur? If fertilization and proper implantation do not occur, the corpus luteum begins to die at about day 26. Estrogen and progesterone blood levels begin to decrease and the stratum functionalis becomes ischemic, leading to menses. If fertilization and proper implantation do occur, the conceptus produces the hormone human chorionic gonadotropin (HCG) that maintains the corpus luteum. Estrogen and progesterone levels continue to support the endometrium. Describe the hormonal changes occurring at each of the stages shown below. 367 1 Ovulation 5 14 26 28 <-----------><---------------> <----------------><------------> Menses Proliferative Secretory Ischemic <------------------------------> <--------------------------------> Preovulatory Postovulatory (Follicular) (Luteal) menses -- estrogen low, progesterone low, FSH level rising proliferative -- estrogen rising, LH spikes at end, FSH decreasing secretory -- estrogen rises again, progesterone rising ischemic -- estrogen falling, progesterone falling D. PHYSIOLOGY OF SEXUAL INTERCOURSE The sexual act, for both males and females, involves four basic stages. The first two stages are common to both sexes. Name and give a brief description of these first two stages. erection -- Psychic and/or tactile stimuli (spinal reflex) cause parasympathetic impulses from the sacral spinal cord to allow vasodilation of penile or clitoral arteries. Increased blood flow in the erectile tissues, with subsequent compression of penile or clitoral veins, results in erection. lubrication -- Continued parasympathetic outflow from the sacral spinal cord causes secretion from the bulbourethral glands (male) or the cervical and greater vestibular glands (female). In the male this serves to neutralize residual acidity in the urethra prior to the passage of sperm. In the female this process provides the lubrication necessary for successful intercourse. The third stage of the sexual act is orgasm. Name and describe the two components of the male orgasm. emission -- When sexual stimulation becomes intense, rhythmic sympathetic outflow from the spinal cord segments L1 - L2 causes peristalsis in the male ducts, from the testes through the vas deferens. This propels sperm and the seminal fluids into the prostatic urethra. ejaculation -- Other rhythmic outflow form the spinal cord S1 - S2 (parasympathetic) stimulates contractions of the pelvic diaphragm, propelling semen through the urethra to the exterior in ejaculation. In addition, there is a generalized fight-or-flight response (increased heart rate, blood pressure, and respirations) as well as intense pleasurable sensations. Immediately thereafter a general 368 relaxation of the body occurs and the resolution phase of the sexual response begins. Describe the female orgasm. Female orgasm occurs when tactile stimulation of the genitalia (particularly the clitoris) reaches maximum intensity and orgasmic reflexes are initiated. Spinal reflexes from L1 - L2 (sympathetic nerves) initiate contractions of the pelvic diaphragm. There is engorgement of the clitoris and breasts with blood, increased heart rate, blood pressure, and respiratory rate, and rhythmic contractions of the uterus. The intensely pleasurable sensations that accompany this response are followed by a return to parasympathetic tone and general relaxation of the body. (resolution phase of the sexual response). There is no equivalent to male emission and ejaculation, but there is similar rhythmic contraction of the pelvic diaphragm. 369