Lab Week 15
advertisement

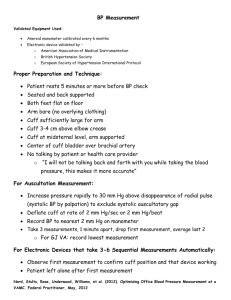
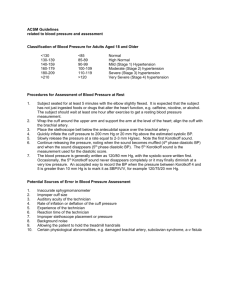
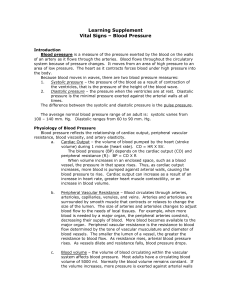
7 November 2003 Folks, For this week you get to try out one of the classic lab exercises in college level physiology. The version that you’ll be using was written by the Biology Department’s Chair, Dr. JI Scheide and has proven to work out quite well from semester to semester. Enjoy! -Dr. Kelty BLOOD PRESSURE, EKG AND PULSE RATE John I. Scheide, Ph.D PURPOSE: 1. 2. 3. 4. To understand the circulatory pump of the body, the heart. To understand the cardiac circulatory pattern and the various controlling mechanisms to cardiac output. To be able to determine blood pressure. To understand the pressure changes caused by the heart and the physiological implications of these changes. To understand the muscle coordination responsible for generating the cardiac cycle. KEY WORDS: atrium (plural=atria), cardiac circulation, circulation, diastole, electrocardiogram, mean arterial pressure, PQRST waves, pulmonary circulation, sphygmomanometer, systemic circulation, systole, and ventricle. TEXTBOOK: 409-421; 460-471. INTRODUCTION The heart is responsible for moving fluid throughout the body. This pump relies on structure to achieve function. Mammalian circulation is the result of a four chambered heart and as with most vertebrates, this circulatory system is closed so the high pressure developed by the heart will ultimately help fill it. Valves prevent the movement of blood back to the heart after being moved out. Blood, coming from the body, enters the heart from the vena cava into the right atrium (plural=atria). The right atrium contracts forcing blood into the right ventricle. Upon filling the right ventricle will contract and blood is forced to the pulmonary artery since a one way valve, the tricuspid valve, closes the right atrium from the right ventricle. Blood flows into the pulmonary system and returns, via the pulmonary veins to the left atrium. The left atrium contracts, forcing blood into the left ventricle. The left ventricle contracts pushing the majority of blood to the aorta and some into the cardiac arteries. The only path for blood from the right ventricle is the aorta due to a valve (bicuspid) closing the path towards the left atrium. Semilunar valves prevent the back flow of blood from the pulmonary and systemic arteries into the respective ventricles. The heart sounds heart with he stethoscope are the result of the various heart valves closing. The right atrium and ventricle are not as heavily muscular as the left side since the pulmonary circulatory system is typically one third the blood pressure of the systemic system. Blood pressure is monitored with the use of a sphygmomanometer and a stethoscope. The sphygmomanometer may be used to accurately determine systolic (ventricle contraction) and diastolic (ventricle relaxation) pressure. The sphygmomanometer has an inflatable cuff that is connected to a pressure gauge. The inflatable cuff may be filled with air until the arterial circulation is cut off. The cuff is placed around the upper arm and the stethoscope listening piece placed on the inside of the elbow. No sounds should be heart with the cuff deflated. The cuff is inflated beyond the point where circulation through the branchial artery is stopped. Then, the cuff pressure is slowly reduced. At the peak systolic pressure, the force of the blood should open the artery a small amount and blood will pass by the cuff blockage. A thumping will be heart with each pulse and a slight deflection of t he pressure needle will be seen. This is the systolic pressure. Continuing to decrease the cuff pressure to a point where the sounds are no longer heard and the needle no longer deflects, represents the minimum blood pressure, diastole. The pressure in the cuff is no longer sufficient to block any portion of the blood pressure gradient. By convention, blood pressure is reported as the systolic over diastolic (systole/diastole) in mm Hg. With four chambers in the heart, the contraction cycle must be coordinated for effective blood flow. The atria contract first in near simultaneous syncrhony. The electrical coordination of t his originates in the sinoatrial node (SA node), an area of nerve and cardiac muscle tissue. Contractions typically are the result of pacemaker cells, which in this case are cardiac cells that spontaneously depolarize. The cell membrane depolarization rate may be influenced by neural (sympathetic and parasympathetic) or hormonal means. Cardiac cells are linked together by gap junctions, thus electrical communication between cells occurs and the heart rate will be dictated by the fastest depolarizing pacemaker cell. Some cardiac cells have differentiated to conduct the cardiac cell depolarization, much like nerves. The depolarization signal goes from the SA node to the atrioventricular node (AV node) along the internodal pathway. The AV node slows the signal then relays the depolarization to the heart apex by way of the Bundles of His. Ventricular contraction starts at the heart apex and moves up the heart to force the blood out efficiently. The electrical changes that occur with the cardiac cycle may be measured and are called an electrocardiogram (EKG). Any EKG change of the electrical cycle or disruption of the electrical pathway may be diagnosed by this noninvasive method. PROCEDURE Part A. 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Measurement of Blood Pressure Practice measuring blood pressure several times if you are unfamiliar with this technique. On a bare arm, wrap the sphygmomanometer cuff around the upper arm such that the gauge is right side and facing you. It is not necessary to make it real tight, only snug. Place the stethoscope in the area of the bend of the elbow. Verify that the air bleed valve on the sphygmomanometer is closed. Pump the cuff up to 160 mm Hg for women 200 mm Hg for men. Do not leave the cuff at this pressure long! The pressure is above the branchial artery pressure, therefore, no circulation is going to the arm. No sound should be heard using the stethoscope. Slowly, open the air bleed valve to decrease the air pressure about 10 mm Hg every 2-3 seconds. Watch the pressure gauge. The first sounds you hear will represent the systolic pressure. Blood is coursing beyond the cuff with each heart contraction and the being constricted when the pressure falls below the cuff pressure. The needle should deflect with each beat. Continue releasing air until the heart sounds fade away. Note the pressure at which the sounds are no longer heard. This is the diastolic pressure. Release the cuff pressure and record the blood pressure. Mean arterial pressure (MAP) is an indication of the overall peripheral resistance. Estimate the MAP by subtracting the diastolic from the systolic pressure. This represents the pulse pressure, the pressure change with the cardiac cycle. Multiply the pulse pressure by 1/3 and add this value to the diastolic pressure. This is the mean arterial pressure. 11. 12. The pulse rate of the subject may be determined by counting the pulses felt with your index or middle finger on the artery located on the inside of the wrist, on the thumb side. Count the pulsations for a 15 second period and multiply by 4 for beats per minute (BPM). Determine the subjects blood pressure, MAP and pulse rate during or immediately after the following conditions: 1. 2. 3. 4. 5. Part B. Sitting Standing Lying down Standing up immediately following the lying down, pump up the cuff before the subject stands up. After 1 minute of exercise. Electrocardiogram. As previously mentioned, the heart has a very coordinated contraction cycle, the result of electrical signals. These electrical events may be examined in a noninvasive manner, by surface electrodes. 1. Verify that the physiograph input switch is set to the EKG and examine the electrode plug area noting the G1, G2 and GRN plugs. 2. Place the double stick circle on to the electrical outer ring. Leave the backing on. 3. To each electrode add electrode cream to the center even or slightly above the outer ring. 4. Carefully remove the backing from the outer circle sticker and place the electrode on a "nonhairy" area with the following arrangement. 1. G1 to the left wrist area 2. G2 to the right wrist area 3. GRN to the left ankle 5. Switch the MacLab system to record and adjust the sensitivity and chart speed to see the EKG. 6. Set the chart speed at a fast rate and determine the time frame for each contractile component. 7. Measure the subjects EKG with the following conditions, 10 seconds each. 1. Sitting 2. Standing 3. Lying 4. Standing up 5. After 1 minute of exercise Name ___________________________ Section # Work Sheet Part A. Blood Pressure Measurements 1. Complete the Chart. Blood Pulse Pressure (mm Hg) Mean Rate (BPM) Arterial Pressure (mm Hg) 1 Sitting 2 Standing 3 Lying Down 4 Immediately Upon Standing 5 After One Minute of Exercise 2. Was there a difference between #2 and #3 normally? What caused the difference between #2 and #4? 3. What occurred to the cardiovascular parameters comparing #2 and #5? 4. Which component of the blood pressure is indicative of stroke volume or the volume moved? Which component will indicate a change in vascular resistance? Why are these an indication of each parameter? Part B. 1. Attach an EKG recording noting the condition under which it was recorded and label the various electrical waves. 2. What was the time frame for the P wave, QRS wave and T wave? How does this time frame relate to the contraction relaxation cycle of the heart? Why is there such a time difference? 3. Did the wave components appreciably change between all conditions? Why or why not?