Urinary System
advertisement

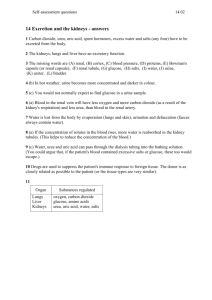
Urinary System I II Functions A Excretion - by kidneys 1) removal of metabolic wastes, toxins, excess ions, and water (a) also performed by skin, liver, and lungs B Regulation 1) of body fluids and electrolytes 2) blood pressure 3) RBC production C Transportation and storage of urine 1) ureters, bladder, and urethra Kidney Structure A External structure - 3 layers 1) renal fascia - thin layer of fibrous C.T., fastens kid. to surrounding struct. 2) adipose capsule - layer of fat, cushions kid. 3) renal capsule - thin layer of fibrous C.T., prevents entrance of infections B Internal structure 1) renal cortex - borders convex side of kid, granular appearance (a) renal columns - portions of cortex tissue that extend inward btwn pyramids 2) renal medulla - deep to cortex, contain 8 - 10 renal pyramids, cone shaped striated structure containing microscopic tubules 3) renal sinus - cavity on concave side of kidn. (a) renal pelvis - a membrane lined cavity w/ funnel shaped extensions called calyces that collect urine, merges w/ ureters (b) hilum - concave margin of each kid. where renal artery, vein, ureters, and nerves join kid. III Blood Supply A Renal arteries branch off abdominal aorta to each kid., carry 1/4 of cardiac output per min B R.A. branches into 5 lobular arteries, enter renal sinus 1) branch into interlobular arteries which extend btwn pyramids 2) branch into arcuate arteries which extend btwn cortex and medulla (a) also branch into afferent arterioles that carry blood to nephrons C Blood is drained by veins w/ similar names into renal vein which empties into infer. vena cava IV Nephron Structure 1M nephrons make up functional tissue of kidney each nephron has a filtering body (renal corpuscle) and urine collecting and concentrating tube (renal tubule) A Renal Corpuscle 1) located in cortex 2) Bowman's capsule - bowl like strctr that encircles a capillary network called the glomerulus, collects filtrate that is forced out of capillaries 3) fenestrae - large pores in endothelial walls of capillaries, leaky caps. 4) podocytes - modified simple squamous epith., forms inner wall of Bowman's capsule (a) branches in cell mem. form filtration slits w/ branches of adjacent cells 5) filtration mem. - glomerulus wall, basement mem., and podocytes, filtrate must cross to enter cavity of Bowman's capsule B Renal Tubule 1) proximal convoluted tubule (PCT) - coiled tube connecting Bow. cap and descending limb of Loop of Henle, lined by simple squamous, lot of mitochondria for reabsorption and secretion 2) Loop of Henle- portion of R.T. that descends into medulla, makes U turn and ascends back to cortex 3) distal convoluted tubule (DCT) - links loop of H. and collecting tube C Blood flow thru the Nephron 1) afferent arteriole >> glomerulus capillary >> efferent arteriole (a) afferent larger diameter that efferent, blood backs up, increases pressure in glom., forces fluid and solutes out of blood into Bow cap. 2) peritubular capillaries - after efferent arteriole, porous, low pressure, surround renal tubule, empties into venous system D Juxtaglomerular Apparatus 1) located where DCT contacts afferent arteriole, made of specialized cells of each (a) granular juxtaglomerular cells in afferent arteriole are specialized smooth muscle cells for mechanoreception, control blood pressure (b) macula densa cells in DCT are chemoreceptors that monitor [Na] and [Cl] in urine 2) regulates rate of urine formation and blood pressure V Urine Formation 1200 ml of blood filtered/min 10% pushed into renal tubules as filtrate; 995 returned to blood 1% leaves body as concentrated urine, 1-2 liters/day A Filtration 1) movement of blood plasma across filtration me. (a) blood cells, platlets, and proteins can't cross (b) glucose, amino acids, urea, K, Cl and plasma enter Bowman's capsule 2) net filtration pressure (NFP) determines quantity of filtrate (a) more pressure >>more urine, less pressure >> (b) controlled by (i) blood pressure + (ii) osmotic pressure of proteins still in glomerulus (iii) capsular pressure of H2O in Bowman's capsuleB Tubular Reabsorption 1) process of reclaiming needed materials and returning them to the blood stream, results in [urine] 2) substances move in one direction, from tubule into peritubular capillaries (a) move by: active transport (Na, AA), diffusion (ions), and osmosis (b) cross three layers 3) PCT - main site of H2O and solute reabsorption, 65% (a) permeability to H2O and ions controlled by hormones 4) Loop of Henle (a) C descending limb -H2O reabsorbed, less solutes >>concentrated filtrate (b) ascending limb - less H2O reabsorbed, glucose and ions actively transported >>dilute filtrate (c) DCT - all but 1% of filtrate has been reabsorbed Secretion VI VII 1) movement of substances from the peritubular cap. into the renal tubule by diffusion, active transport, or facilitated diffusion 2) includes ions that may become toxic (H+, K+0), drugs, ammonia, urea, and uric acid 3) blood pH monitored and controlled by CO2/H2CO3 buffer system Urea and Uric Acid Excretion A Both are nitrogen-containing waste products 1) urea results from protein metabolism >> ammonia , converted by liver to urea, 50% of urea in filtrate is excreted in urine 2) uric acid result of nucleic acid metabolism, 10% removed in urine Regulation of Urine Concentration and Volume A Kidneys work to maintain constant blood composition and volume 1) affected by food and water intake, activity level, disease 2) controlled by hormones and nervous input Renin juxtaglomerular cells causes Angioitension I to be converted to Angiotension II which stimulates adrenals to release Aldosterone, causes afferent arteriole to constrict net affect: Increase BP >>more filtrate Aldosterone Adrenal gland increase active transport of Na and Cl back into blood, H2O follows, net affect: reduced volume of urine, increase BP Antidiuretic Hormone ADH Posterior Pituitary increase H2O reabsorption in DCT and collecting ducts, net affect: concentrated urine, increase in BP Atrial Natriuretic Factor Right Atrium of Heart reduces ability of kid. to reabsorb solutes and H2O, net affect: large volume of urine, decrease in blood volume and BP Sympathetic impulses during f,f,f Hypothalamus vasoconstriction of afferent arteriole, reduces flow to glomeruli, net affect: decrease in filtrate and urine formation