Specialist Referral Policy & Procedure Example for PGIP
advertisement

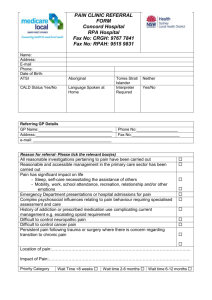
Specialist Referral Policy and Procedure Example for PGIP The Physician Alliance Category: 14.0 Specialist Referral Process for Primary Care Providers Practice name: (insert practice name) 14.1 & 14.2 – Process/procedure for specialist referral and/or appointment with preferred or high volume specialists and for other key specialist providers. Procedure: 1. A directory of preferred referral specialist is maintained by the practice (14.3 capability). 2. Staff have defined roles in the referral process and are trained on the process as indicated in their employee file (14.8 – staff is trained on referral process). 3. The need for a referral to the specialist is identified by the physician. 4. A standardized referral summary form (see attached form) is completed by the nurse/MA that documents name, location and contact information for the specialist. Form also includes what is the purpose of the referral, the timeframe for which the referral needs to be completed. This information is provided in writing during the visit or by mail based on the condition (14.4 – specialist referral materials). 5. The practice has a file of business cards to be provided to the patient at the time the referral is made. 6. For urgent referrals and for patients that wish assistance in making the referral appointments, the staff calls the specialist and the appointment is made (14.5 – make specialist appointments on behalf of patient). 7. If the patient is going to make their own appointment, a copy of the referral form is put in the referral folder and the patient is instructed to call the office with their appointment date. When the patients call back with the appointment day, the appointment date is recorded on the referral form and placed in the tracking folder. If the patient hasn’t called back within 14 days, the patient is contacted to assist in the patient making the specialist appointment. 8. A copy of the referral form is sent to the specialist. The referral form and any pertinent laboratory and/or radiology results key to the referral are faxed to the specialist. All referrals to any physician are copied and placed in referral tracking folder at the front desk. A copy of the referral form is given to the patient. 9. If no specialist report is received within 30 days of the appointment date, a phone call is made to the specialist office to obtain results/report of the referral. For urgent Specialist Referral Policy and Procedure Example for PGIP The Physician Alliance referrals, follow-up timeframe is determined by the date recorded on the referral form. 10. If upon calling the specialist, it is determined that patient did not see the specialist, the patient is contacted by the nurse/MA to see why the referral was not completed in the recommended timeframe. The date and reason for not completing the referral is placed on the referral form and recorded in the medical record. The physician is notified of the lack of referral completion and reason why patient did not complete. At the discretion of the physician, the physician may call the patient and addresses the need to complete the referral if patients condition still warrants referral. 11. At the beginning of each month, the designated staff reviews all remaining forms in the referral tracking folder. Each referral pending more than 60 days will complete the steps as outlined in steps #9 and #10 above. (14.7 – process to determine whether or not patients completed referral). 12. When test the results/report is received from specialist, the referral form is removed from the referral tracking folder and shredded after the physician signs off on the referral results/report. If additional recommended services or testing is ordered by the specialist, the service is monitored through the practices test tracking process. 13. At next patient visit or at least annually, the physician asks the patient if the specialist referral was satisfactory and patients are also provided a Specialist Satisfaction Survey to complete (14.9 – evaluations of patient satisfaction with Specialists) 14.6 – Each facet of the interaction between preferred/high volume specialists and the PCPs at the practice unit level is automated by using electronically-based tools and processes to avoid duplication of testing and prescribing across multiple care settings Procedure: No fully automated process exists at this time.