medication changes for psychiatric patients
advertisement

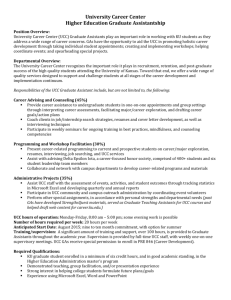
URGENT CARE CENTER ORIENTATION 1/21/03 DOCUMENTATION: All patient visits, including those related to medication refill and establishing care must have either a dictated note or a typed note in CPRS. Notations on the 1010M are not sufficient but should include: diagnosis, attending name (residents only), your name, and admitting ward (if applicable) on 1010M. 1. CPRS Notes: a. A note must be typed in CPRS if: 1) The patient is admitted to the hospital 2) The patient is referred from a Community-Based Outpatient Clinics (CBOC) 3) The patient is referred from the Brecksville VA b. To type notes go to the NOTES TAB and select “New Note”. Use the NOTE TITLE “Urgent Care 10-10M (T)” and complete the physician portion of the template OR click on cancel and use a blank note. c. For patients sent from the CBOC use the NOTE TITLE “Urgent Care (C)” and complete the template OR click on cancel and use a blank note -This includes all patients sent from Brecksville, Akron, Canton, East Liverpool, Warren, Sandusky, McCafferty, Youngstown, Mansfield, Painesville, New Philadelphia, Lorain, and Wade Park -A consult request should have been sent from these sites and can be viewed on the CONSULTS TAB. It is called “W Urgent Care Transfer” d. Patients are generally coming to the UCC for a focused problem. Please remember to type or dictate focused, brief notes with only essential information. Complete H&Ps are not necessary even on patients that are to be admitted. e. A typed note must be done on all patients that are admitted and the accepting physician’s name should be included at the bottom of the note, i.e. report called to Dr. Tomolo. f. RESIDENTS must designate the UCC attending as a co-signer for each note or consult completed. g. The patient’s PCP may also be included as an additional signer so that they can be alerted about the Urgent Care visit 2. Dictation: a. If you are dictating notes at the VA for the first time call ext. 7670 to obtain a dictation code. b. Patient visits may be dictated (see dictation instructions) EXCEPT if the patient is being admitted to the hospital or being referred from the CBOC or Brecksville VA. c. All dictations will appear in your ALERTS in CPRS as unsigned notes and MUST be signed so that they can be viewed in CPRS. d. A dictation instruction sheet is posted in the Physician’s Conference Room. 3. UCC Consults: a. Referrals from the CBOC, including Brecksville, are placed on the marker board closest to the Physician’s Conference Room. 1 b. Look for CPRS consult request on patients sent from CBOC (select the “Consults” Tab and look for “W Urgent Care Transfer” consult). These consults are printed in Urgent Care and will be placed by the clerks in the patient’s folder/chart. -An indication for the referral is included in request. -The CBOC provider name and number is included in request. c. CBOC providers MUST BE CALLED if the patient is NOT being admitted and the CBOC provider made a request for admission on the “W Urgent Care Transfer” consult OR if a patient requires quick follow-up by the CBOC provider. 4. Time: a. It is essential to document turn-around time of patient visits. This assists in addressing difficulties with dispositions of patients and associated resource needs. b. A time stamp is located at the nurses’ station near the patient board. Stamp the 1010M at the end of the patient visit OR write the time of discharge at the bottom of the 1010M and designate it as the discharge time so that this time can be recorded. 5. Encounter forms: a. Complete printed encounter form that is kept with the chart and IGNORE computer prompt that asks if you are the primary provider for the visit. b. These forms will be used to tract provider workload. c. Residents, MODs, and PAs should record their name as the secondary provider. The nurses will also be recording their name as a secondary provider. d. Record the following on the encounter form: i) Name of the attending name (if you are a resident) ii) Severity level of visit iii) Procedures performed in UCC iv) Main symptom or diagnosis associated with the patient’s UCC visit in the first column labeled “P” (If the diagnosis is not on the form it may be written at the bottom of the form.) ADMISSIONS: 1. There are two medical teams and one ICU/telemetry admitting patients everyday. a. On M-F, except holidays, there are 2 short call admissions to the medical teams before 2pm; unless the intern has clinic, then that intern admits 1 patient before 12noon b. The interns on long call have a cap of 5 patients and they do not receive admissions after 6am on the morning after the call night. c. The ICU/telemetry intern on-call admits all patients to the ICU and telemetry before 11pm. After 11pm either call the ICU/telemetry resident on-call with admissions to the ICU and telemetry or call the ICU, extension 5040 and ask for the resident accepting admissions. There is no cap of patients. 2. Ward 41 is a modified telemetry ward. Patients may not be “ruled out” on this ward and NO CARDIAC MEDICATIONS MAY BE GIVEN IVP on this ward, i.e. metoprolol, digoxin. Patients that may be appropriate for this ward include those with hyperkalemia or syncope. a. Admissions to W4 1 require approval by the CCU attending (24 hours a day/ 7 days a week). 2 b. The CCU attending may decide to have the patient on the ICU/telemetry team or a General Medicine Team. The CCU attending is to communicate this information to the W41 nursing staff, and the UCC provider is to communicate this information to the UCC nursing staff. 3. Admissions to the medical team after 6am are to stay in the UCC until 7am. Call report to the intern on-call for that day at 7am and have the patient admitted to the medical ward before 7:30am 4. Patients may not be admitted to any ward between nursing change of shift from 7:30-8am and 3:30-4pm. This is effective every day of the week. UCC FLOW: 1. Updating patient board: a. Erase names of discharge patients b. Write your name or initials next to the patients that you are seeing c. If you bring someone into a room write your name and the patient name next to the room # d. If you send a patient to the waiting room or chairs while awaiting test results move the patient name to the bottom of the board e. Indicate admission & ward #, consulting service, radiology, and labs in the blank column next to the patient’s name 2. The nurses will be bringing patients into rooms, chairs, or carts in the main area. a. If the nurses are busy there may be a delay in bringing patients into the main area. If rooms are available and patients are waiting in the acute rack please bring these patients in the back and record their name on the board. b. Check with the charge nurse or the attending before filling up all of the acute rooms as there may be ambulance transfers coming that will need to utilize a bed. c. Ambulance transfers are identified on the marker board below the pager numbers. When there are many transfers it is prudent to leave 1-2 beds open or see only minor cases in those rooms so that they can be moved quickly when an ambulance patient arrives. 3. Patients that no longer require monitoring or use of the room should be moved to the waiting room or to chairs if they are awaiting test results. 4. Notify the attending if patients are taking a long time to be admitted to the ward. 5. The resident on-call will be responsible for relieving the MOD at 8am and managing the medicine admitting book, including taking calls related to admissions from other locations. 6. One 2nd or 3rd year resident is assigned each day to the UCC Fast Track. The letters “FT” on the Screening Schedule indicate this assignment. a. The assigned resident, Richard Leseman (PA), and Frank Aguayo (PA) will staff Fast Track. b. Patients will be assigned to fast track from 8am – 6pm on M-F, except holidays. c. Fast Track charts are placed in the rack outside of the nurse triage. d. Fast track patients should be staffed with the attending on-duty in UCC. 7. Patients requiring lab tests that are not waiting for their test results should be sent to the outpatient lab to have their blood draw. These blood tests should be ordered in the computer. The outpatient lab is open M-F, except holidays, from ~8am-4:30pm. 3 REFERRALS: Placing a consult in CPRS creates a referral for follow-up to the outpatient clinics. If the patient requires follow-up in LESS THAN TWO WEEKS the outpatient clinic or resident/fellow assigned to that service should be called to set up the quick follow up. Telling the patient to “walk-in” to the clinic for an appointment is not appropriate. 1. Psychiatry Consults: a. All psychiatric patients MUST BE SEEN by an Urgent Care Provider for a medical evaluation prior to consultation with psychiatry. i. Consults should be placed in CPRS to “W Psychiatry OPPC (Outpatient)” and the oncall psychiatry provider should be paged. ii. The UCC nursing staff can place the consult or page psychiatry, if necessary, but the UCC provider should be communicating with the psychiatry service about the patient’s medical and psychiatric issues so that a timely and appropriate disposition may be made. b. EXCEPTION: Psychiatry may be called prior to the medical evaluation if there are urgent psychiatric issues, i.e. the patient is violent or agitated, or the patient is a high elopement risk. c. A medical evaluation must be completed on all psychiatric patients, as there are often many overlapping issues. The results of the medical evaluation should be communicated to the psychiatry consultants. 2. General Surgery Consults: a. All acute surgical issues should be called to the general surgery resident on-call. b. A consult must be placed in the computer for patients to be referred to general surgery clinic. The residents are not able to schedule appointments or overbook the clinic. The consult will be reviewed and an appointment scheduled by the surgery staff. 3. Gastroenterology Consults: a. GI consults that are needed in less than one month should be discussed with the outpatient fellow on weekdays or the on-call fellow on weekends so that they can be overbooked in the clinic 4. Trauma: a. Occasionally patients “walk-in” to the Urgent Care Center following an acute trauma and in this situation the General Surgery senior resident on-call should be paged to assist with the trauma evaluation. b. This procedure has been arranged after discussion with Dr. Graham (Chief of Surgery). RADIOLOGY: 1. UCC PLAIN FILM RADIOLOGY LOG: a. All patients that are seen in Urgent Care and have x-rays performed should be entered in the binder labeled “UCC Plain Film Radiology Log”. b. Enter the patient’s last name, last 4 of SSN, date of x-ray, film type and your preliminary interpretation of the film in the log book 4 c. The logbook is kept in the Physician’s Conference Room. d. This data will be collected and entered in a database twice a day on Monday-Friday. e. You will receive feedback on missed diagnosis and may be asked to assist with follow-up of these cases. 2. SPECIALTY FILMS AFTER HOURS: a. CT Scans i. A CT tech is available Sunday-Thursday from 4:30pm-12 midnight ii. To obtain a CT scan at other times or it there are problems page the nursing supervisor. iii. The CT tech should be able to come in from home in 30-45 minutes. b. Ultrasounds i. Check the Radiology call schedule to see if the UH radiologist or the VA radiologist is on call. ii. Contact the on-call radiologist to discuss the case and make arrangements for testing. iii. If the VA radiologist is on-call that provider will come to the VA to complete the test. iv. If the patient is stable for transfer and the UH radiologist is on-call: 1. Complete a non-VA procedure request form 2. Arrange for transfer to UH for the test. 3. Check with the AOD if there are questions. v. If the patient is unstable for transfer the on-call radiologist will come to the VA to complete the test. c. MRI i. For emergent MRIs after hours contact the UH radiology resident. Discuss the case with the radiologist and make arrangements for testing at UH. Prior to sending the patient to UH for testing perform the following tasks: 1. Complete a non-VA procedure request form 2. Arrange for transfer to UH for the test. 3. Check with the AOD if there are questions. d. Results i. For results of specialty films page the on-call radiology resident at UH (B# 32494) or call the UH radiology switchboard by dialing 96-43061. NARCOTICS: 1. Patients on chronic narcotics should have those refilled ONLY by their primary care provider or the pain clinic. 2. Before prescribing narcotics please review the patients chart to look for historical information about prescription medication use and follow up appointments. 3. Narcotics are to be prescribed in the UCC for acute injuries only. 4. Please note if the patient demonstrates the four signs of addiction in a chronic pain patient: a. Impaired control of opioid medication b. Compulsive use; spending all of his time trying to obtain opioids c. Continued use despite harm and medical advice to stop d. Craving that is implied by a sole focus on obtaining opioids. 5 RESTRICTED MEDICATIONS: 1. You must call the service assigned to the restricted medication otherwise the medication will be discontinued for the patient (i.e. amlodipine restricted to cardiology) 2. Dr. Fleming (440-507-0242) is the contact person for non-formulary medications. MEDICATION CHANGES FOR PSYCHIATRIC PATIENTS When making changes in psychiatric medications for psychiatry patients contact the psychiatry on-call pager or the psychiatry resident on-call about the modifications. SCHEDULES: 1. All questions related to the UCC resident schedules should be communicated to the Ambulatory Chief Resident, B#31533 2. All questions related to the MOD schedule should be communicated to Janet Thompson (ext. 4819) or Dr. Tomolo (B# 440-562-0963) 6