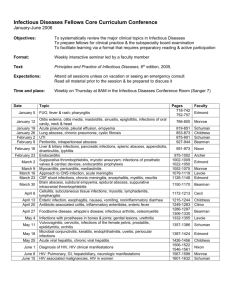
INFECTIOUS DISEASES - Dimensions Healthcare System
advertisement
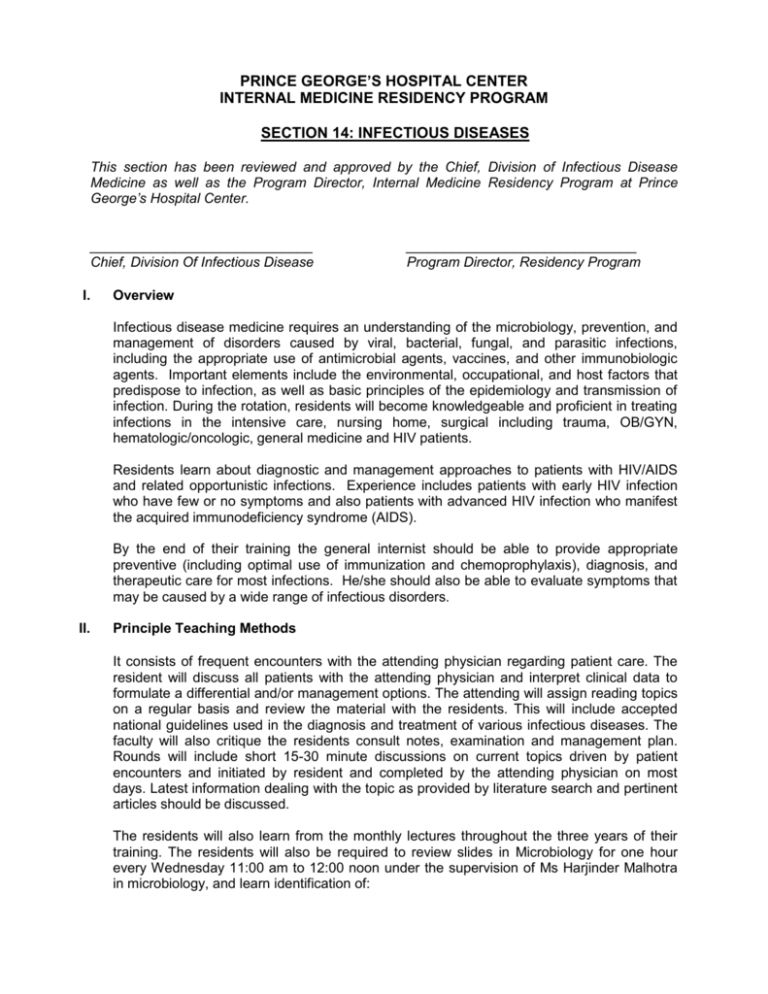
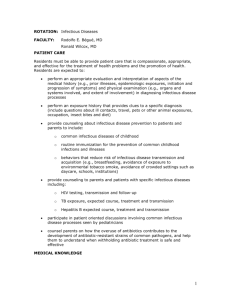
PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM SECTION 14: INFECTIOUS DISEASES This section has been reviewed and approved by the Chief, Division of Infectious Disease Medicine as well as the Program Director, Internal Medicine Residency Program at Prince George’s Hospital Center. _____________________________ Chief, Division Of Infectious Disease I. ______________________________ Program Director, Residency Program Overview Infectious disease medicine requires an understanding of the microbiology, prevention, and management of disorders caused by viral, bacterial, fungal, and parasitic infections, including the appropriate use of antimicrobial agents, vaccines, and other immunobiologic agents. Important elements include the environmental, occupational, and host factors that predispose to infection, as well as basic principles of the epidemiology and transmission of infection. During the rotation, residents will become knowledgeable and proficient in treating infections in the intensive care, nursing home, surgical including trauma, OB/GYN, hematologic/oncologic, general medicine and HIV patients. Residents learn about diagnostic and management approaches to patients with HIV/AIDS and related opportunistic infections. Experience includes patients with early HIV infection who have few or no symptoms and also patients with advanced HIV infection who manifest the acquired immunodeficiency syndrome (AIDS). By the end of their training the general internist should be able to provide appropriate preventive (including optimal use of immunization and chemoprophylaxis), diagnosis, and therapeutic care for most infections. He/she should also be able to evaluate symptoms that may be caused by a wide range of infectious disorders. II. Principle Teaching Methods It consists of frequent encounters with the attending physician regarding patient care. The resident will discuss all patients with the attending physician and interpret clinical data to formulate a differential and/or management options. The attending will assign reading topics on a regular basis and review the material with the residents. This will include accepted national guidelines used in the diagnosis and treatment of various infectious diseases. The faculty will also critique the residents consult notes, examination and management plan. Rounds will include short 15-30 minute discussions on current topics driven by patient encounters and initiated by resident and completed by the attending physician on most days. Latest information dealing with the topic as provided by literature search and pertinent articles should be discussed. The residents will also learn from the monthly lectures throughout the three years of their training. The residents will also be required to review slides in Microbiology for one hour every Wednesday 11:00 am to 12:00 noon under the supervision of Ms Harjinder Malhotra in microbiology, and learn identification of: Cocci and bacilli Gram stains (15) to identify Gram postive and negative bacteria India ink (5) Malaria smear (1) Wet mounts (5): ( in the ER laboratory) The residents will be provided with a sign-in/attendance sheet that they must get signed by microbiology supervisor to show successful completion of this requirement. III. Strengths and Limitations The residents will be exposed to a broad range of clinical problems typical of a communitybased practice with emphasis on inpatient illness and care. The teaching faculty for the rotation is committed to teaching and patient care with strong role model presentation. For patients with exceptionally unusual clinical problems, the care may require transfer to a tertiary referral center. Patients in the continuity clinic at Glenridge Medical Center also offer some learning opportunities regarding prevention, screening and long term follow-up of patients with HIV. The hospital does not have a transplant unit therefore exposure of residents to organ transplant patients with opportunistic infections is limited. IV. Goals and Objectives At the beginning of each academic year the residents will receive a didactic session on ID emergencies. This will be followed by monthly lectures by ID faculty and will cover the following topics: Lyme’s Disease Tuberculosis Rashes and other skin manifestations of systemic illnesses Meningitis and interpretation of CSF findings Endocarditis Travel medicine Skin and soft tissue infections Approach to antibiotic therapy There will also be scheduled lectures on HIV related topics to cover management of HIV and its related infections and medications in a systematic manner. Legend of Learning Activities Learning Venues: 1. Direct Patient Care/Consultation 2. Attending Rounds 3. Core Lecture Series 4. Self Study Evaluation Methods: A. Attending Evaluation B. Direct Observation C. Nurses’ Evaluation D. In-training Examination Competency: Patient Care Demonstrate the ability to perform history & physical exam, interpret ancillary tests to make diagnostic and therapeutic decisions. Competency: Medical Knowledge Understand the pathophysiology, evaluation, and management of microbiological diseases (bacterial, viral, mycobacterial, parasitic, fungal, and rickettsial). Understand the pathophysiology, evaluation, and management of HIV and AIDS related infections. Understand the pathophysiology, evaluation, and management catheter related infections, endocarditis, and pneumonia, Understand the pathophysiology, evaluation, and management central nervous system infections. Understand the pathophysiology, evaluation, and management GI related illnesses. Understand the pathophysiology, evaluation, and management of surgical infections. Understand the pathophysiology, evaluation, and management septic and critically ill patients. Understand the pathophysiology, evaluation, and management immunocompromised patients such as transplant patients. Understand the pathophysiology, evaluation, and management febrile neutrapenia and other hematological/oncological infections. Understand the pharmacodynamics and pharmokinetics of antimicrobial agents. Understand the pathophysiology, evaluation, and management of sexually transmitted diseases. Competency: Professionalism Treats patients, team members, and primary caregivers with respect. Shows compassion to patients, families, and colleagues. Actively participates in consultations and rounds. Attends and participates in all scheduled conferences. Competency: Practice Based Learning Evaluates own performance and uses medical literature to address gaps in medical knowledge. Incorporates feedback into improvement activities. Learning Venues 1,2.3 Evaluation Methods A,B Learning Venues 1,2,3,4 Evaluation Methods A,B,D 1,2,3,4 A,B,D 1,2,3,4 A,B,D 1,2,3,4 A,B,D 1,2,3,4 A,B,D 1,2,3,4 A,B,C,D 1,2,3,4 A,B,C,D 4 D 1,2,3 A,B,D 1,2,3 A,B,D 1,2,3 A,B,D Learning Venues 1,2 Evaluation Methods A,B,C 1,2 A,B,C 1,2 Attendance sheet A,B Learning Venues 1,2 Evaluation Methods A,B,D 1,2 A,B Competency: System Based Practice Understands the barriers to optimal care of patients with HIV. Understands the need for teamwork with multiple caregivers, social work, and case management. 1,2 A, 1,2 A,B,C V. Educational Content 1. Central Nervous System Brain abscess Encephalitis Meningitis- all types 2. Cardiovascular system Endocarditis: acute, subacute, prosthetic valve Pericarditis 3. Critical Care Unit SIRS Sepsis, septic shock syndrome Nosocomial Infections Ventilator Associated Pneumonia 4. Fever of unknown origin 5. Fungal Histoplasmosis Cocciidioidomycosis Cryptococcosis 6. Gastrointestinal Biliary tract infection Gastroenteritis Infectious diarrhea Liver abscess Peritonitis Viral hepatitis 7. Genitourinary Cervical cancer (HPV) Cervicitis, vaginitis Common sexually transmitted diseases: gonorrhea, chlamydia, trichomonas, herpes simplex, syphilis) Pelvic inflammatory disease Prostatitis, epididymitis Urethritis Urinary tract infection 8. Infection in the immunosuppressed patient 9. Lyme Disease 10. Malaria 11. Respiratory Acute epiglottitis, pharyngitis Empyema Pneumonia (community and nosocomial), bronchitis Sinusitis Upper respiratory infection 12. Rheumatologic/musculoskeletal Osteomyelitis Septic arthritis 13. Rocky Mountain Spotted Fever 14. Skin Infections Cellulitis Folliculitis Ulcers Viral exanthema 15. Tuberculosis Active infection Positive tuberculin skin test 16. Viral Cytomegalovirus Herpes simplex infection Influenza Mononucleosia Varicella zoster infection 17. HIV Infection i. AIDS-defining Malignancies Kaposi’s sarcoma Non-Hodgkin’s lymphoma Squamous cell carcinoma (cervix or anus) ii. Cardiovascular Complications Cardiomyopathy Myocarditis Pericarditis iii. Dermatologic Complications Bacillary angiomatosis H. zoster Kaposi’s sarcoma Molluscum contagiosum Scabies Seborrheic dermatitis iv. Endocrine Complications Hypoadrenalism Hypogonadism Lipodystrophy v. Gastrointestinal Complications Diarrhea Esophageal candidiasis Esophageal ulcer disease Hepatomegaly, hepatitis, jaundice Wasting syndrome vi. General Management Evaluation and management of early disease Advance directives evaluation Assessment of alternative health practices Assessment of social support systems Monitoring progression to AIDS vii. Ongoing Staging Diagnosing AIDS-defining opportunistic infections Functional assessment Mental status evaluation Nutritional assessment Referral to case-management agencies Palliative and terminal care Pregnancy counseling (pretest, post-test, risk factors) viii. Gynecologic Complications Cervical dysplasia/neoplasia Pelvic inflammatory disease Vaginal candidiasis ix. Hematologic Complications Anemia x. Infectious Diseases (see also Preventive Measures and Specific Organ-based Complications) Cytomegalovirus disease Mycobacterial disease Pneumocystis carinii pneumonia Syphilis (diagnosis, treatment) xi. Neurologic Complications Central nervous system mass lesions Cryptococcal meningitis Dementia Myelopathy Myopathy Neurosyphilis Peripheral neuropathy Polyneuropathy Wasting Syndrome xii. Ocular Complications Conjunctivitis Iritis Keratitis Retinitis xiii. Oral Complications xiv. Pregnancy Counseling pretest, post-test, risk factors HAART therapy during pregnancy xv. Ongoing Staging Diagnosing AIDS-defining opportunistic infections Functional assessment Mental status evaluation Nutritional assessment Referral to case management agencies, palliative and hospice care xvi. Preventive Measures Antibiotic prophylaxis: Pneumocystis carini pneumonia, Toxoplasmosis, Mycobacterium Avium Complex Immunizations Transmission of HIV xvii. HAART therapy Side effects, indications and contraindications of various medications Drug Interactions xviii. Ordering and Understanding Tests HAART sensitivity testing- genotype and phenotype CD4 lymphocyte counts Cerebrospinal fluid cell count, chemistry, VDRL, cryptococcal antigen, cytology Computed tomography, magnetic resonance imaging of the central nervous system ELISA, polymerase chain reaction, and immunoblotting techniques Induced sputum stain for Pneumocystis carinii VI. Polymerase chain reaction ELISA and Western blot for detection of infectious diseases Syphilis serology and dark-field microscopy Toxoplasma serology Recommended Reading Residents are expected to pursue directed reading of standard texts and journal articles pertinent to the clinical problems they encounter. On a case by case basis residents should refer to: MKSAP Up To Date MDConsult Mandell GL, Bennett JE, Dolin R (eds): Principals and Practices of Infectious Diseases (5th ed). Philadelphia: Churchill Livingstone, 2000 The residents should also read the following articles during their rotation. 1) Schacker T, Collier AC, Hughes J, Shea T, Corey L. Clinical and epidemiologic features of primary HIV infection. Ann Intern Med. 1996 Aug 15;125(4):257-64. 2) Hammer SM, et al. Treatment for adult HIV infection, 2006 recommendations of the International AIDS society- USA Panel. JAMA. Aug 16,2006; 296 (7): 827843 3) Skiest Daniel J. Focal neurological disease in patients with acquired immunodeficiency syndrome. Clinical Infectious Diseases. 2002; 34: 103-15 4) Hirsch HH, et al. Immune reconstitution in HIV-infected patients. Clinical Infectious Diseases. 2004;38: 1159-1166 5) Dajani AS, Taubert KA, Wilson W, Bolger AF, Bayer A, Ferrieri P, Gewitz MH, Shulman ST, Nouri S, Newburger JW, Hutto C, Pallasch TJ, Gage TW, Levison ME, Peter G, Zuccaro G Jr. Prevention of bacterial endocarditis. Recommendations by the American Heart Association. JAMA. 1997 Jun 11;277(22):1794-801. 6) Such J, Runyon BA. Spontaneous bacterial peritonitis. Clin Infect Dis. 1998 Oct;27(4):669-74. 7) Lew DP, Waldvogel FA. Osteomyelitis. N Engl J Med. 1997 Apr 3;336(14):999-1007. 8) Caputo GM, Cavanagh PR, Ulbrecht JS, Gibbons GW, Karchmer AW. Assessment and management of foot disease in patients with diabetes. N Engl J Med. 1994 Sep 29;331(13):854-60. 9) Lipsky BA, et al. Diagnosis and treatment of diabetic foot infections, IDSA guidelines. Clinical Infectious Diseases. 2004; 39:885-910 10) Quagliarello VJ, Scheld WM. Treatment of bacterial meningitis. N Engl J Med. 1997 Mar 6;336(10):708-16. 11) Tunkel AR, et al. Practice guidelines for the management of Bacterial Meningitis- IDSA guidelines. Clinical Infectious Diseases. 2004;39: 1267-84 12) Kelly CP, Pothoulakis C, LaMont JT. Clostridium difficile colitis. N Engl J Med. 1994 Jan 27;330(4):257-62. 13) Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998 Aug 20;339(8):520-32. 14) Mermel LA, et al. Guidelines for the management of intravascular catheter-related infections. Clinical Infectious Diseases. 2001;32: 1249-72 15) Bartlett JG, Dowell SF, Mandell LA, File Jr TM, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Infectious Diseases Society of America. Clin Infect Dis. 2000 Aug;31(2):347-82. 16) 1998 Guidelines for Treatment of Sexually Transmitted Disases: US Dept of Health. MMWR: 47 (RR-1): Jan 23, 1998 http://www.cdc.gov/mmwr/preview/mmwrhtml/00050909.htm PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM MICROBIOLOGY ATTENDANCE SHEET RESIDENT NAME_____________________________________ GRAM STAIN MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result SUPERVISOR COMMENTS (IF ANY) SUPERVISOR SIGNATURE and DATE RESIDENT NAME_____________________________________ MR# Result INDIA INK SUPERVISOR COMMENTS (IF ANY) SUPERVISOR SIGNATURE and DATE WET MOUNT SUPERVISOR COMMENTS (IF ANY) SUPERVISOR SIGNATURE and DATE MALARIA SMEAR SUPERVISOR COMMENTS (IF ANY) SUPERVISOR SIGNATURE and DATE MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result MR# Result Result