Renal15-RegulationOfNaAndH2OBalance
advertisement

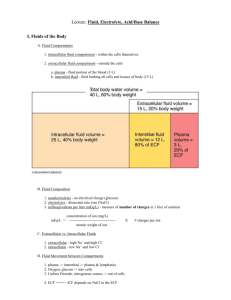
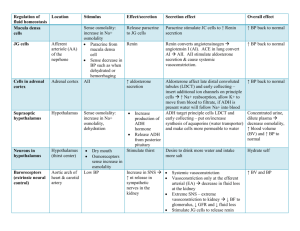
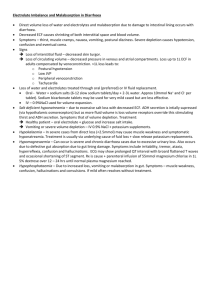
Renal #15 Wed, 03/19/03, 11am Dr. Mallet Scott Emerson Page 1 of 4 Session 6: Body Fluid Compartments: Physiological Control of Sodium and Water Balance I. Major Body Fluid Compartments A. Extracellular Fluid: plasma, interstitial fluid and lymph, synovial, intraocular fluid… B. Intracellular Fluid: RBC’s, and other cells FYI: 70kg man has roughly 40L of water: over half water neonates are 75% water II. Electrolyte composition of ICF and ECF differ A. Major EC cation is Na; anions are Cl and HCO3 B. Major IC cation is K; anions are organic phosphates (ATP) FYI: despite the differences in solute compositions the total solute concentration of both compartments is identical; due to H2O permeability. If any gradient est. then H2O will move by osmosis to equilibrate to two sides of the membrane Graphical Representation of Osmotic Equilibration: X-axis is [solute]; Y-axis is V 1. Initially, ECF and ICF have similar [solute] 2. If 3L of H2O is removed I love cats from ECF your ECF V decreases and therefore gives you a greater solute concentration (they were “left behind”) in the ECF; because of this an osmotic gradient is created 3. Gradient causes H2O diffusion from ICF to ECF for equilibration so have same [solute] 4. The ECF regains some of its V but not all; change in V of each compartment is proportional to the share of the total water V started with 5. Thus if the ICF is 2/3 the water of the body and someone losses a L of water by sweating; after equilibration, the ECF V will be down 1/3 of a L and the ICF will be down 2/3 of a L….calculations not expected on the exam III. Total Body Na content determines ECF V A. Increase of total Na content (which is normally found in the ECF) → B. H20 osmosis from cells (cells would shrink); osmoR respond to shrinking (or swelling) and they send signals to cerebral cortex and “tell you” that you are thirsty, renal H20 retention → C. ECFV → D. Hypertension and edema (if mechs not working properly) FYI: this process would occur is increasing your normal salt intake FYI: CHF’ers should abstain from salt (hypertensive situation) IV. Sodium Balance A. Determine ECFV B. Body Na content is determined by Na intake-excretion C. Dietary Na intake is not regulated in humans (is, however, regulated in Mr. Ed) 1. kidneys control body Na content by adjusting excretion D. ECFV→Na excretion (body thinks have too much Na; less Aldo/more NAP) E. ECFV→Na conserved (to expand the V) Renal #15 Wed, 03/19/03, 11am Dr. Mallet Scott Emerson Page 2 of 4 V. Reabsorption of filtered Na load A. Bulk reab of filtered Na in PCT (proximal tubule; 2/3 reab here), Henle (TAL: 25% b/c of Na/K/2Cl cotransport) B. CCD “fine tunes” Na handling; adjustments made due to requirement of the body’s need of Na (adjusts amount of reab/excreted) VI. Neurohumoral factors controlling renal Na excretion A. Factors that promote Na REABSORPTION (want to BP) 1. Renal sympathetic nerves 2. Renin/angio system 3. Aldo B. Factors that promote Na EXCRETION (want to BP) 1. Atrial natriuretc peptide (ANP) 2. Prostaglandin VII. Sympathetic stimulate Na Reab, Renin Secretion A. Look at PP for schematic FYI: macula densa senses Na → rennin secretion → AngioII VIII. Factors that promote rennin secretion A. Renal sympathetic stimulation B. Tubuloglomerular FB: NaCl delivery to MD C. Intrarenal baroR: afferent arteriolar P IX. AngioII Stimulates: A. Systemic arteriolar constriction B. Renal arteriolar constriction (efferents primarily) C. Proximal tubular Na reabsorption D. Thirst: makes you thirsty to help expand your ECFV and restoration of BP (retention + intake →V) E. ADH secretion from Post. Pit. F. Aldo secretion from adrenal cortex X. Response of rennin/angioto ECFV A. Look at PP for schematic XI. Aldosterone’s Actions in Collection Ducts A. Stimulates Na REAB B. Stimulates K SECRETION C. Stimulates H SECRETION D. All trying to conserve Na and H20 XII. Factors Controlling Aldo Secretion A. Look at PP for schematic B. AngioII primarily C. ANP suppresses Renal #15 Wed, 03/19/03, 11am Dr. Mallet Scott Emerson Page 3 of 4 XIII. ANP s Na and H20 Excretion A. BP causes atria muscle to stretch consequently releasing ANP B. ANP s GFR: dilation of afferent arterioles and constriction of efferent C. ANP inhibits Na reabsorption in MEDULLARY cats I love collecting ducts so that you have an ed of Na in urine D. ANP suppresses rennin secretion and lower angioII E. ANP suppresses aldo secretion from adrenal cortex F. ANP is a systemic VD to BP G. ANP suppresses ADH secretion from Post Pit. so kidneys retain less H2O and Na →ECFV and BP XIV. Anatomy of ADH Synthesis and Secretion A. Only H that will control H20 B. ADH from hypo. (spec. from paraventricular and supraoptic) C. Stored in Post. Pit near capillary plexus (readily taken up in blood) D. OsmoR control formation and secretion of ADH XV. OsmoR/BaroR control ADH secretion A. OsmoR found in kidney (and hypo) are sensitive to EC [solute] B. When [solute] cells shrink b/c H2O out. C. When shrink they no longer inhibit activity of neurons in hypo that produce ADH D. BaroR in carotid sinus normally inhibit ADH secretion too but b/c of BP E. With the restoration of BP BaroR influence removed F. Retention of H2O dilutes the EC [solute] and removes the OsmoR influence XVI. Plasma ADH vs. Osmolarity, Blood V A. Graphs in PP B. BaroR less sensitive 1. big increase of ADH secretion (look at X-axis between the two graphs) C. Vasopressin 1. Systemic VC to stabilize BP XVII. Changes in BV Modulate Osmolarity-Dependent Changes in Plasma ADH A. Graph in PP B. V expansion that dampens the response to changes in osmolarity 1. greater [solute] to get given of ADH C. V loss shifts curve left and is more sensitive: small [solute] produces ADH XVIII. Renal Response to Increased NaCl intake assuming healthy A. Schematic in PPs XIX. Retention of NaCl and H20 when hemorrhaging XX. Disorders of Salt and H20 Balance A. Hyponatremia: [Na] low B. Hypernatremia: [Na] high C. HypoV: ECFV contraction D. HypoV: ECFV expansion Renal #15 Wed, 03/19/03, 11am Dr. Mallet Scott Emerson Page 4 of 4 XXI. Hyponatremia A. Indicates hypotonicity of ECF 1. low Na concentration (low total Na) 2. Osmotic gradient for H20 into cells causing swelling (may cause neuro problems) B. Not due to Na loss 1. Indicates too much H20 relative to Na in body 2. Body, therefore, should respond by excrete H20 by inhibiting ADH C. Two main categories 1. Pseudohyponatremia a. [Na] low but normal total [solute] b. from too much of a large molecule; if [] too high then those compounds will occupy an unusually high space within the plasma (greater V of non-H20) 2. True hyponatremia a. [Na] and total [solute] are low XXII. Case 1 A. low [Na] B. high glucose C. total osmo is within normal range D. hyponatremia due to glucose: draws H2O out of cells; dilutes [Na] XXII. Blood Chemistries A. Determine the EC [solute] B. 2(Na) + glucose/18 + BUN/2.8 C. Osmolar Gap: Difference between plasma osmolarity estimated as above and true plasma osmolarity measured with an osmometer 1. Normally less then 10mOsm difference 2. Difference between the calculated value and the true from the osmometer 3. True osmolality should be 10 or less greater than the estimate D. Case 1 Example: 2(125) + 720/18 + 14/2.8 =295 does not have a high osmolar gap; her hyperglycemia accounts for the hyponatremia XXIII. Case 2 A. [Na] low B. not hyperglycemic C. Estimate = to 260; huge gap so have an “immeasurable” active compound in blood (ethylene glycol from antifreeze…if you can’t get drunk on beer….) D. ROH is drawing H2O out of cells and diluting the ECF and causing the hyponatremia Note on Cases: both are examples of feline pseudohyponatremia Note on subliminal messages: very PC of the individual that decided to introduce these into my scribe