Pectoralis Major Resuspension in Aesthetic Breast Surgery
advertisement

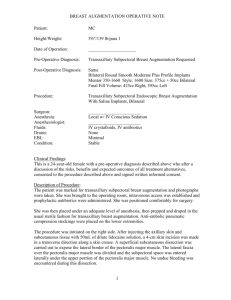
Difficulties with Subpectoral Augmentation Mammoplasty and its Correction: Pectoralis Major Reconstruction in Aesthetic Breast Surgery Andrew P Trussler MD, Brian P Dickinson MD, Reza Jarrahy MD, Malcolm A Lesavoy MD Purpose: Controversy exists over the concepts of implant placement and augmentation mammoplasty. Proponents give good reasons for subpectoral versus subglandular implant placement, with the tendency towards the subpectoral placement in the United States (1,2). Informal surveys of plastic surgeons done by the senior author indicate a 50/50 preference, both in Central and South America, and Europe. Difficulties arise with subpectoral placement of the implant including: malpositioning of the implant, improper superior contouring, inappropriate and unnatural movement with range of motion, and capsular contraction (3). We have found that correction of these above deformities are relatively easily maintained by removal of the subpectoral implant, reconstruction of the pectoralis major muscle back down to the chest wall, and reaugmentation with the implant in the subglandular space. This study will define a correction modality for the adverse results of subpectoral implant placement in augmentation mammoplasty. Methods: Pectoralis major reconstruction was performed in 36 patients undergoing revision aesthetic breast surgery from 1995 to 2006. All patients had subpectoral breast implants with unwanted movement, malposition, and/ or capsular contraction. All patients underwent explantation of the breast implant via an inframammary incision with a modified capsulectomy and pectoralis major reconstruction. The inferior and medial aspects of the pectoralis major muscle were sutured back down to the chest wall, and reaugmentation of the breast was done with implants placed in the subglandular position. In the cases of symmastia, medial capsulodesis and bolster sutures were used. Patients were evaluated for resolution of symptoms, satisfaction and complications. Results: Thirty-six patients underwent successful reconstruction of the pectoralis major during revision aesthetic breast surgery with an average follow-up of one year. Malpostion (62%), capsular contraction (53%), unwanted movement (33%), and symmastia (10%) were the most common indications for revision. The majority of the patients underwent re-augmentation with smooth silicone implants (81%); while one patient underwent augmentation with saline implants, and one patient underwent augmentation with textured silicone implants. The average volume change ranged from a decrease of 200 cc to an increase of 150 cc with an average decrease in volume by 27 cc. Three of the thirty-six (8%) underwent implant removal, pectoralis muscle reconstruction, and mastopexy without re-implantation. Unwanted implant movement was completely eliminated (100%), symmastia was corrected (100%), and capsular contracture was significantly decreased in each respective group. All patients were satisfied post-operatively. Overall complications were low. There was one hematoma which occurred in a patient with post-operative hypertension. There were two cases of early, Baker Grade II capsular contractures within the first 6 months; however these have not required re-operation over 2 years of follow-up. Conclusion: Pectoralis major reconstruction can be successfully performed in aesthetic breast surgery. It can be safely applied to correct problems of unwanted implant movement, symmastia implant malposition, and capsular contraction. The use of silicone gel implants in a novel tissue plane may be beneficial in this diverse, re-operative patient population. References: 1. Tebbetts, JB. Dual Plane Breast Augmentation: Optimizing Implant-Soft-Tissue Relationships in a Wide Range of Breast Types. Plast Reconstr Surg; 107(5); 1255-1272; 2001. 2. Strasser EJ. Results of Subglandular Versus Subpectoral Augmentation Over Time: One Surgeon’s Observations. Aesthetic Surg J; 26; 45-50; 2006. 3. Spear SL, Carter ME, Ganz JC. The correction of capsular contracture by conversion to "dual-plane" positioning: technique and outcomes. Plast Reconstr Surg; 118(7 Suppl); 103S-113S; 2006.