114CSR14
advertisement

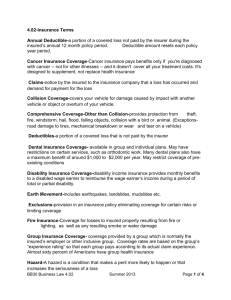
Page 1 WEST VIRGINIA FAIR CLAIMS SETTLEMENT PRACTICES REGULATIONS WEST VIRGINIA CODE OF STATE RULES TITLE 114. INSURANCE COMMISSIONER SERIES 14 UNFAIR TRADE PRACTICES1 §114-14-1. General. 1.1. Scope. a. The purpose of this rule is to define certain practices in this state which constitute unfair methods of competition or unfair or deceptive acts or practices and to establish certain minimum standards and methods of settlements of both first-party and third-party claims. b. This rule does not prohibit the use of additional methods above the minimum which are not in violation of this rule or any other West Virginia statute or rule. c. This rule applies to all persons and to all insurance policies and insurance contracts except Workers’ Compensation Insurance. d. This rule is not exclusive, and other acts, not herein specified, may also constitute unfair claims settlement practices. e. Nothing in this rule creates or recognizes, either explicitly or impliedly, any new or different cause of action not otherwise recognized by law. §114-14-2. Definitions. For the purposes of this regulation, the following definitions shall apply: 2.1. “Agent” means any individual, corporation, association, partnership or other legal entity authorized to represent an insurer with respect to a claim. 2.2. “Claimant” means either a first-party claimant, a third-party claimant, or both. 2.3. “First-party claimant” or “Insured” means an individual, corporation, association, partnership or other legal entity asserting a right to payment under an insurance policy or insurance contract arising out of the occurrence of the contingency or loss covered by such policy or contract. 2.4. “Person” includes any individual, company, insurer, association, organization, society, reciprocal, business trust, corporation or any other legal entity, including agents, adjusters and brokers. 2.5. “Insurer” means a person licensed to issue or who issues any insurance policy or insurance contract covering risks resident, located or to be performed in this state. 2.6. “Investigation” means all activities of an insurer or agent directly or indirectly related to the determination of liabilities under coverages afforded by an insurance policy or insurance contract. 2.7. “Notification of claim” means any notification, whether in writing or other means acceptable under the terms of 1 This document is comprised only of those portions of the West Virginia Code of State Rules that are most relevant to claims handling. Revised in March 2009, includes Regulations in effect through December 2008. Rev. 04-2014 CHD/P&S/alr Page 2 an insurance policy or insurance contract, to an insurer or its agents, by a claimant, which reasonably apprises the insurer or agent of the existence of an occurrence which might give rise to liability under a policy or contract of insurance. 2.8. “Third-party claimant” means any individual, corporation, association, partnership or other legal entity asserting a claim against any individual, corporation, association, partnership or other legal entity insured under an insurance policy or insurance contract of an insurer. 2.9. “Settlement of claims” means all activities of the insurer or its agent which are related directly or indirectly to the determination of the compensation that is due under coverage afforded by the insurance policy or insurance contract. This includes, but is not limited to, the requiring or preparing of repair estimates. 2.10. “Insurance policy” or “Insurance contract” means the contract effecting insurance, or the certificate thereof, by whatever name called, and includes all clauses, riders, endorsements and papers issued under the terms of the policy or contract. 2.11. “Claim” means any communication by a claimant to an insurer or its agent which reasonably apprises the insurer or agent of an occurrence which might give rise to liability under a policy or contract of insurance. 2.12. “Commissioner” means the West Virginia Insurance Commissioner. 2.13. “Licensee” means any person that holds a license or certificate of authority from the Commissioner, or any other entity for whom the Commissioner’s consent is required before transacting business in the State of West Virginia or with residents of West Virginia. §114-14-3. File And Record Documentation. The insurer’s claim files shall be subject to examination by the Commissioner or by his or her duly appointed designees. Such files shall contain all notes and work papers pertaining to the claim in such detail that pertinent events and the dates of such events can be reconstructed. All communications and transactions emanating from or received by the insurer shall be dated by the insurer. A notation of the substance and date of all oral communications shall be contained in the claim file. Insurers shall either make a notation in the file or retain a copy of all forms mailed to claimants. §114-14-4. Representation of Policy Provisions and Benefits. 4.1. Failure to disclose pertinent policy provisions. -- No person may knowingly fail to fully disclose to first-party claimants all pertinent benefits, coverages or other provisions of an insurance policy or insurance contract under which a claim is presented. 4.2. Concealment of pertinent policy provisions. -- No person may knowingly conceal from first-party claimants benefits, coverages or other provisions of any insurance policy or insurance contract when such benefits, coverages or other provisions are pertinent to a claim. 4.3. Coercive statements. -- No person may make statements which indicate that the rights of a claimant may be impaired if a form or release is not completed within a given period of time unless the statement is given for the purpose of notifying the claimant of the provisions of a statute of limitation or of a policy or contract time limit. 4.4. Time limit for notification of claim. -- Except where a time limit is specified by statute or legislative rule, no insurer may require a first-party claimant to give notification of a claim or proof of claim within a specified time. 4.5. Releases. a. No person may ask a first-party claimant to sign a release that extends beyond the subject matter which gave rise to the claim payment. Rev. 04-2014 CHD/P&S/alr Page 3 b. No insurer may issue any check or draft, in partial settlement of a loss or claim under a specific coverage, that contains language which releases the insurer or its insured from its total liability. §114-14-5. Standards For The Acknowledgment Of Pertinent Communications. 5.1. Acknowledgment of notices of claims. -- Every insurer, upon receiving notification of a claim shall, within fifteen (15) working days, acknowledge the receipt of such notice unless full payment is made within such period of time. If an acknowledgment is made by means other than writing, an appropriate notation of such acknowledgment shall be made in the claim file of the insurer and dated. Notification given to an agent of an insurer shall be notification to the insurer. 5.2. Answer of inquiries from Insurance Commissioner. -- Every insurer, producer or other licensee, upon receipt of any inquiry other than a notice of third-party administrative complaint from the Insurance Commissioner shall, within fifteen (15) working days of the date appearing on the inquiry, furnish the Commissioner with a complete written response to the inquiry. A “complete written response” addresses all issues raised by the claimant or the Commissioner and includes copies of any documentation requested. This subsection is not intended to permit delay in responding to inquiries by the Commissioner or his or her staff in conjunction with a scheduled examination on the insurer’s premises. 5.3. Replies to other pertinent communications. -- A reply shall be made within fifteen (15) working days of receipt by the insurer to all other pertinent communications from a claimant which reasonably suggest that a response is expected. 5.4. Provisions of assistance to first-party claimants. -- Every insurer, upon receiving notification of a claim, shall promptly provide necessary claim forms, instructions, and reasonable assistance so that first-party claimants can comply with the policy conditions and the insurer’s reasonable requirements. Compliance with this subsection within fifteen (15) working days of notification of a claim constitutes compliance with subsection 5.1. of this section. §114-14-6. Standards For Prompt Investigations And Fair And Equitable Settlements Applicable To All Insurers. 6.1. Investigation of claims. -- Every insurer shall promptly conduct and diligently pursue a thorough, fair and objective investigation and may not unreasonably delay resolution by persisting in seeking information not reasonably required for or material to the resolution of a claim dispute. This section is not intended to conflict with the statutory requirements of the Medical Professional Liability Act, W. Va. Code §§55-7B-1 to 11, as the same relate to the assertion and investigation of medical professional liability claims. 6.2. Establishment of investigatory procedures. -a. Every insurer shall establish procedures to commence an investigation of any claim filed by a claimant, or by a claimant’s authorized representative, within fifteen (15) working days of receipt of notice of claim. b. Every insurer shall provide to every first-party claimant, or to the claimant’s authorized representative, a notification of all items, statements and forms, if any, which the insurer reasonably believes will be required of such claimant, within fifteen (15) working days of receiving notice of the claim. c. A claim filed with an agent of an insurer shall be deemed to have been filed with the insurer unless, consistent with law or contract, such agent promptly provides written notification to the person filing the claim that the agent is not authorized to receive notices of claim. 6.3. Duty after investigation. -- Within ten (10) working days of completing its investigation, the insurer shall deny the claim in writing or make a written offer, subject to policy limits and, with respect to medical professional liability claims, subject to applicable statutory requirements set forth in the Medical Professional Liability Act, W. Va. Code §§55-7B-1 to 11. 6.4. Offers of settlement. – Rev. 04-2014 CHD/P&S/alr Page 4 a. In any case where there is no dispute as to coverage and liability, it is the duty of every insurer to offer claimants or their authorized representatives, amounts which are fair and reasonable, as shown by the insurer’s investigation of the claim, providing the amounts so offered are within policy limits and in accordance with the policy provisions. b. No insurer may attempt to settle a claim by making a settlement offer that is unreasonably low. The Commissioner shall consider any evidence offered regarding the following factors in determining whether a settlement offer is unreasonably low: 1. The extent to which the insurer considered evidence submitted by the claimant to support the value of the claim; 2. The extent to which the insurer considered legal authority or evidence made known to it or reasonably available; 3. The extent to which the insurer considered the advice of its claims adjuster as to the amount of damages; 4. The extent to which the insurer considered the opinions of independent experts; 5. The procedures used by the insurer in determining the dollar amount of property damage; 6. The extent to which the insurer considered the probable liability of the insured and the likely jury verdict or other final determination of the matter; and 7. Any other credible evidence presented to the Commissioner that demonstrates that the final amount offered in settlement of the claim by the insurer is or is not below the amount that a reasonable person would have offered in settlement of the claim after taking into consideration the relevant facts and circumstances at the time the offer was made. 6.5. Denial of claims. -- No insurer may deny a claim on the grounds of a specific policy provision, condition or exclusion unless reference to such provision, condition or exclusion is included in the denial. The denial must be given to the claimant in writing or as otherwise provided in subsection 6.6. of these rules. 6.6. Records of denial of claims. -- If a denial of a claim is made by any other means than writing, an appropriate notation shall be made in the claim file of the insurer. 6.7. Notice of necessary delay in investigating claims. -- If the insurer needs more than thirty (30) calendar days from the date that a proof of loss from a first-party claimant or notice of claim from a third-party claimant is received to determine whether a claim should be accepted or denied, it shall so notify the claimant in writing within fifteen (15) working days after the thirty-day period expires. If the investigation remains incomplete, the insurer shall provide written notification of the delay to the claimant every forty-five (45) calendar days thereafter until the investigation is complete. All such notifications must set forth the reason(s) additional time is needed for investigation. Where there is a reasonable basis supported by specific information available for review by the Commissioner that a claimant has fraudulently caused or contributed to the loss, the insurer is relieved from the requirements of this subsection: Provided, That the insurer shall notify the claimant of the acceptance or denial of the claim within a reasonable time allowing for full investigation. Nothing contained in this subsection requires an insurer to disclose any information that could reasonably be expected to alert a claimant to the fact that the subject claim is being investigated as a suspected fraudulent claim. 6.8. Liability of others. -- Insurers may not refuse to settle first-party claims on the basis that responsibility for payment should be assumed by others except as may otherwise be provided by policy provisions. 6.9. Denial of claims for failure to exhibit property. -- No insurer may deny a claim for failure to exhibit the insured property without proof of demand by the insurer and refusal by the claimant to exhibit said property. Rev. 04-2014 CHD/P&S/alr Page 5 6.10. Separation of claims. -- In any case where there is no dispute as to one (1) or more elements of a claim, payment for such element(s) shall be made notwithstanding the existence of disputes as to other elements of the claim where such payment can be made without prejudice to either party. 6.11. Time for payment of claims. -- Every insurer shall pay any amount finally agreed upon in settlement of all or part of any claim not later than fifteen (15) working days from the receipt of such agreement by the insurer or from the date of the performance by the claimant of any condition set by such agreement, whichever is later. 6.12. Notice of applicable time limitations. -- No person may negotiate for settlement of a claim with a claimant who is neither an attorney nor represented by an attorney without giving the claimant written notice that the claimant’s rights may be affected by a statute of limitations or a policy or contract time limit. Such notice shall be given to first-party claimants not less than thirty (30) days, and to third-party claimants not less than sixty (60) days, before the date on which such time limit expires. 6.13. Avoidance of payment. -- Where liability and damages are reasonably clear, no person may recommend that third-party claimants make claim under their own policies solely to avoid paying claims under an insurer’s insurance policy or insurance contract. 6.14. Unreasonable travel. -- No person may require a claimant to travel unreasonably either to inspect a replacement motor vehicle or to obtain a repair estimate. 6.15. Compensation based on claim denials. -- No insurer may offer incentives or compensate its employees, agents or contractors based on savings to the insurer as a result of improperly denying the payment of claims. 6.16. Claim proceeds used to pay premiums of another policy. -- No insurer may deduct from a claim payment made under one policy premiums owed by the insured on another policy unless the insured consents. 6.17. Required information for claim denial notices. -- Any notice rejecting any element of a claim shall contain the identity and the claims processing address of the insurer and the claim number. The notice must state that the claimant has the option of contacting the Commissioner. The notice must provide the Commissioner’s mailing address, telephone number and web site address. 6.18. Motor vehicle repair shops. -- An insurer may furnish to the claimant the names of one or more conveniently located motor vehicle repair shops that will perform the repairs; however no insurer may require the claimant to use a particular repair shop or location to obtain the repairs. §114-14-7. Standards For Prompt, Fair And Equitable Settlements Applicable To Automobile Insurance. 7.1. Applicability. -- This section is applicable to claims arising under motor vehicle collision and comprehensive coverage. The provisions of section 6 of these rules are applicable to these claims except to the extent that such provisions are inconsistent with the specific provisions of this section. 7.2. Definition of terms. -- The following shall govern the construction of the terms used in this section: a. “Agreed price” means the amount agreed to by the insurer and the insured, or their representatives, as to the reasonable cost to repair damages to the motor vehicle resulting from the loss, without considering any deductible or other deductions; b. “Designated representative” means a person designated by the insured to represent him or her in negotiations with the insurer in an attempt to settle the claim. The designated representative may be a member of the insured’s immediate family or any other person named by the insured who may legally act on his or her behalf and who so acts without compensation of any kind; c. “Motor vehicle” has the meaning ascribed in subsection (b), section one, article one, chapter seventeen-a of the Code of West Virginia of 1931, as amended; Rev. 04-2014 CHD/P&S/alr Page 6 d. “Official used car guide” means a valuation source that has been approved by the Commissioner for setting the minimum value of a motor vehicle which is the subject of a total loss claim. In order to be approved by the Commissioner as an official used car guide, the valuation source must meet the following criteria: 1. All valuation sources must: A. Produce statistically valid fair market values based on current data available primarily from the area surrounding the location where the insured vehicle was principally garaged or a necessary expansion of parameters, such as time and area, to assure statistical validity; B. Produce values for at least eighty-five percent (85%) of all makes and models of private passenger automobiles for the last fifteen (15) model years and include all major options. A sufficient number of vehicles shall be used for each year, make and model to represent a cross-section sufficient to determine fair market values; C. Produce for examination by the Commissioner, at the time the request for approval is made or as soon thereafter as practicable, the source of the data in a manner that can be verified by the Commissioner; D. Make available for examination by the Commissioner, at the time the request for approval is made or as soon thereafter as practicable, any contracts or agreements between the valuation source and insurers, which the valuation source may assert is a trade secret pursuant to W. Va. Code §47-22-1(d); and E. Produce for examination any other information determined by the Commissioner to be helpful or necessary in determining the statistical validity of the values produced by the valuation source, or otherwise bearing on the integrity of the valuation source, including the existence of and resolution of consumer complaints based upon total loss valuations performed by the source. If the information meets the definition of trade secret pursuant to W. Va. Code §47-22-1(d), then the valuation source may make available for examination by the Commissioner, without filing the same, any information requested pursuant to this subparagraph. If the information meets the definition of trade secret pursuant to W. Va. Code §47-22-1(d) and, after having been made available for examination by the Commissioner, the Commissioner determines that the information pertains to the existence of or resolution of consumer complaints, the valuation source shall propose a reasonable method for protection of the information. 2. A valuation source that is other than a valuation manual, including a computerized database, must meet the criteria set forth in subparagraphs A, B, C, D and E of paragraph one of this subdivision, and in addition must: A. Give primary consideration to the values of vehicles in the local market area but if necessary to obtain a reasonable cross-section of the market, may consider vehicles in the next closest area; B. Rely upon values of vehicles that are currently available or were available within ninety days from the date of loss for all vehicles and apply appropriate standards of comparability; C. Rely upon values derived primarily from verifiable data or inventory from licensed dealers which have minimum sales of one hundred motor vehicles per year in the local market area, for vehicles of five model years or less of age; D. Monitor the average retail price of private passenger automobiles when there is insufficient data or inventory from licensed dealers to ensure statistically valid market area values; and E. Clearly indicate and describe the condition at which the vehicle is being valued, if the valuation source uses several price ranges for the same model vehicle depending on the condition of the vehicle. Documentation of the condition of the insured vehicle must be made a part of the written valuation. Rev. 04-2014 CHD/P&S/alr Page 7 Deductions made for the condition of the insured vehicle must be reasonably based on a physical attribute that has the effect of decreasing the vehicle’s value. e. “Substantially similar vehicle” means a motor vehicle of the same make, model, year and substantially the same condition, including all major options of the insured vehicle. Mileage may not exceed that of the insured vehicle by more than 4,000 miles unless mutually acceptable to both the insurer and the insured. 7.3. Adjustment of partial losses. -- The following subdivisions govern the conduct of insurers in the adjustment of partial losses: a. Insurers shall include the insured’s deductible, if any, in subrogation demands. Subrogation recoveries shall be shared on a proportionate basis with the insured, unless the deductible amount has been otherwise recovered. No deduction for expenses may be made from the deductible recovery unless an outside attorney is retained to collect such recovery. The deduction may then be for only a pro rata share of the allocated loss adjustment expense; b. If an insurer prepares an estimate of the cost of the motor vehicle repairs, such estimate shall be in an amount for which it may be reasonably expected the damage can be satisfactorily repaired. The insurer shall give a copy of the estimate to the insured and may furnish to the insured the names of one or more conveniently located repair shops that will perform the repairs for the amount tendered in settlement of the claim; c. If the insurer intends to exercise its rights to inspect damages prior to repair, it has seven (7) working days from the date of receipt of notice of loss to inspect the insured’s damaged motor vehicle at a place and time reasonably convenient to the insured. In addition, negotiations shall commence and a good faith offer of settlement shall be made within the aforesaid seven (7) day period; d. If the insured’s motor vehicle is repaired at a repair shop recommended by the insurer, for a sum estimated by the insurer as the reasonable cost to repair the vehicle, the insurer shall, at no additional cost to the claimant and within a reasonable period of time, cause the damaged vehicle to be restored to the condition it was in prior to the loss if the repair shop it recommended does not so repair the damaged motor vehicle; e. Deductions for betterment and/or depreciation are permitted only for parts normally subject to repair and replacement during the useful life of the insured motor vehicle. Deductions for betterment and/or depreciation are limited to an amount equal to the proportion that the expired life of the part to be repaired or replaced bears to the normal useful life of that part. Calculations for betterment, depreciation and normal useful life must be included in the insurer’s claim file; f. Deductions for previous damage or prior condition of the motor vehicle must be measurable, discernible, itemized and specified as to dollar amount, and such deductions must be detailed in the claim file; g. The insurer must mail or hand deliver to the insured or his or her designated representative its proof of loss or payment within ten (10) working days after the insured has accepted the insurer’s offer; h. If the insurer does not perform its own physical inspection, it is nevertheless bound by all the applicable requirements of this regulation. 7.4. Adjustment of total losses. -- The following subdivisions govern the conduct of insurers in the adjustment of total losses: a. If the insurer elects to make a cash settlement: 1. It must use the most recent version of an “Official Used Car Guide” approved by the Commissioner and uniformly and regularly used by the company, as a guide for setting the minimum value of the motor vehicle which is the subject of the claim. Any deviation downward from the guide’s retail valuation must be supported by documentation that gives detailed information about the vehicle’s condition, and any deductions must be measurable, discernible, itemized and specified concerning dollar amount, and they Rev. 04-2014 CHD/P&S/alr Page 8 shall be appropriate in amount. This documentation must be maintained in the claim file; 2. If the retail value of the specific motor vehicle is not contained in the most recent version of an “Official Used Car Guide” approved by the Commissioner and which is used uniformly and regularly by the company, the company must secure dealer quotations on the retail value of similar vehicles and base the settlement upon them. The offer must enable the insured to purchase the substantially similar vehicle for the cash settlement and any deviation from this practice must be supported by documentation giving particular information about the motor vehicle’s condition. The documentation and the source of the dealer quotations must be maintained in the claim file; 3. The company shall provide a reasonable written explanation to the concerned parties when cash settlement offers, as set forth in paragraphs (1) and (2) above are made. The explanation must specify the dollar amount of the base figure and identify the actual source. Any additions or subtractions from the base dollar figure must be identified and explained; and 4. In addition to any cash settlement value agreed to by the claimant, there must be added an amount equal to five percent (5%) of such cash settlement value, as reimbursement to the claimant for the excise tax imposed by the state. b. If the insurer elects to replace the vehicle, the replacement vehicle must be an immediately available, substantially similar vehicle that is both furnished and paid for by the insurer, subject to the deductible, if any. c. If the insured vehicle is a private passenger automobile of the current model year, meaning that it has not been superseded in the marketplace by an officially introduced succeeding model, the insurer shall utilize one of the following methods in the settlement of the loss, except where the method used would be detrimental to the interests of the insured as compared with utilization of the methods described in subdivisions a. and b. above: 1. The insurer shall pay to the insured the reasonable purchase price on the date of loss of a substantially similar vehicle, less any applicable deductible and an allowance for depreciation in accordance with an official used car guide which has been approved by the Commissioner and is used regularly by the insurer; or 2. The insurer shall furnish the insured with a substantially similar replacement vehicle, and charge the insured for any applicable deductible and for depreciation in accordance with the official used car guide. d. If the insurer, in the process of adjusting a total loss, makes a deduction for the salvage value of the insured vehicle, the insurer must furnish the insured with the name and address of a salvage dealer who will purchase the salvage for the amount deducted. e. All applicable provisions of subsection 7.3. of this section, “Adjustment of Partial Losses,” also apply to the adjustment of total losses, except that the insurer is allowed an additional five (5) working days to comply with the requirements set out in subsection 7.3. of these rules. Any letter of explanation or rejection of any element of a claim shall contain the identity and claims processing address of the insurer, the insured’s policy number and the claim number. 7.5. Unreasonable delay. -- If any element of a physical damage claim remains unresolved more than fifteen (15) working days from the date of receipt of proofs of loss by the insurer, the insurer shall provide the insured with a written explanation of the specific reasons for the delay in the claim settlement unless reasonable grounds exist to suspect fraud or arson. An updated letter of explanation shall be sent every thirty (30) calendar days thereafter until all elements of the claim are either honored or rejected. 7.6. Repair estimates. -- If an insurer requires that its insured obtain an estimate or estimates of vehicle damage, the reasonable charges, if any, of such estimates shall be borne by the insurer. 7.7. Notice of right to reimbursement for transportation expenses. -- In the event of the theft of the entire vehicle, it is the duty of the insurer at the time of notification of loss to advise the insured of his or her right under the policy to Rev. 04-2014 CHD/P&S/alr Page 9 be reimbursed for transportation expenses. Such notification must be confirmed in writing immediately after receipt of notice of theft. All conditions and benefits related to this coverage as stated in the policy must be contained in the notification to the insured. §114-14-8. Training and Certification. Within ninety (90) days of the effective date of this rule, every insurer shall adopt and communicate to all its claims agents written standards for the prompt investigation and processing of claims. SERIES 57. PRIVACY OF CONSUMER FINANCIAL AND HEALTH INFORMATION § 114-57-1. General. 1.1. Scope. -- This rule governs the treatment of nonpublic personal health information and nonpublic personal financial information about individuals by all licensees of the West Virginia Insurance Commission. 1.2. Authority. -- W. Va. Code §§33-2-10, 33-6F-1 and 33-11A-4. a. This rule: 1. Requires a licensee to provide notice to individuals about its privacy policies and practices; 2. Describes the conditions under which a licensee may disclose nonpublic personal health information and nonpublic personal financial information about individuals to affiliates and nonaffiliated third parties; and 3. Provides methods for individuals to prevent a licensee from disclosing that information. b. This rule applies to: 1. Nonpublic personal financial information about individuals who obtain or are claimants or beneficiaries of products or services primarily for personal, family or household purposes from licensees. This rule does not apply to information about companies or about individuals who obtain products or services for business, commercial or agricultural purposes; and 2. All nonpublic personal health information. c. A licensee domiciled in this state that is in compliance with this rule in a state that has not enacted laws or rules or regulations that meet the requirements of Title V of the Gramm-Leach-Bliley Act (PL 102-106) may nonetheless be deemed to be in compliance with Title V of the Gramm-Leach-Bliley Act in the other state. § 114-57-2. Definitions. … 2.15. "Health information" means any information or data except age or gender, whether oral or recorded in any form or medium, created by or derived from a health care provider or the consumer that relates to: a. The past, present or future physical, mental or behavioral health or condition of an individual; b. The provision of health care to an individual; or Rev. 04-2014 CHD/P&S/alr Page 10 c. Payment for the provision of health care to an individual. … 2.18. "Nonaffiliated third party" means any person except: a. A licensee's affiliate; or b. A person employed jointly by a licensee and any company that is not the licensee's affiliate (but nonaffiliated third party includes the other company that jointly employs the person). c. Nonaffiliated third party includes any company that is an affiliate solely by virtue of the direct or indirect ownership or control of the company by the licensee or its affiliate in conducting merchant banking or investment banking activities of the type described in section 4(k)(4)(H) or insurance company investment activities of the type described in section 4(k)(4)(I) of the federal Bank Holding Company Act (12 U.S.C. 1843(k)(4)(H) and (I)). 2.19. "Nonpublic personal information" means nonpublic personal financial information and nonpublic personal health information. 2.20. "Nonpublic personal financial information" means: a. Personally identifiable financial information; and b. Any list, description or other grouping of consumers (and publicly available information pertaining to them) that is derived using any personally identifiable financial information that is not publicly available. c. Nonpublic personal financial information does not include: 1. Health information; 2. Publicly available information, except as included on a list described in subdivision b of this subsection; or 3. Any list, description or other grouping of consumers (and publicly available information pertaining to them) that is derived without using any personally identifiable financial information that is not publicly available. d. Nonpublic personal financial information includes any list of individuals' names and street addresses that is derived in whole or in part using personally identifiable financial information that is not publicly available, such as account numbers. e. Nonpublic personal financial information does not include any list of individuals' names and addresses that contains only publicly available information, is not derived in whole or in part using personally identifiable financial information that is not publicly available, and is not disclosed in a manner that indicates that any of the individuals on the list is a consumer of a financial institution. 2.21. "Nonpublic personal health information" means health information: a. That identifies an individual who is the subject of the information; or b. With respect to which there is a reasonable basis to believe that the information could be used to identify an individual. 2.23. "Personally identifiable financial information" means any information: a. A consumer provides to a licensee to obtain an insurance product or service from the licensee; Rev. 04-2014 CHD/P&S/alr Page 11 b. About a consumer resulting from a transaction involving an insurance product or service between a licensee and a consumer; or c. The licensee otherwise obtains about a consumer in connection with providing an insurance product or service to that consumer. d. Personally identifiable financial information includes, but is not limited to: 1. Information a consumer provides to a licensee on an application to obtain an insurance product or service; 2. Account balance information and payment history; 3. The fact that an individual is or has been one of the licensee's customers or has obtained an insurance product or service from the licensee; 4. Any information about the licensee's consumer if it is disclosed in a manner that indicates that the individual is or has been the licensee's consumer; 5. Any information that a consumer provides to a licensee or that the licensee or its agent otherwise obtains in connection with collecting on a loan or servicing a loan; 6. Any information the licensee collects through an Internet cookie (an information-collecting device from a web server); and 7. Information from a consumer report. e. Personally identifiable financial information does not include: 1. Health information; 2. A list of names and addresses of customers of an entity that is not a financial institution; and 3. Information that does not identify a consumer, such as aggregate information or blind data that does not contain personal identifiers such as account numbers, names or addresses. 2.24. "Publicly available information" means any information that a licensee has a reasonable basis to believe is lawfully made available to the general public from: a. Federal, state or local government records; b. Widely distributed media; or c. Disclosures to the general public that are required to be made by federal, state or local law. d. A licensee has a reasonable basis to believe that information is lawfully made available to the general public if the licensee has taken steps to determine: 1. That the information is of the type that is available to the general public; and 2. Whether an individual can direct that the information not be made available to the general public and, if so, that the licensee's consumer has not done so. e. Publicly available information in government records includes information in government real estate records and security interest filings. Rev. 04-2014 CHD/P&S/alr Page 12 f. Publicly available information from widely distributed media includes information from a telephone book, a television or radio program, a newspaper or a web site that is available to the general public on an unrestricted basis. A web site is not restricted merely because an Internet service provider or a site operator requires a fee or a password, so long as access is available to the general public. g. A licensee has a reasonable basis to believe that mortgage information is lawfully made available to the general public if the licensee has determined that the information is of the type included on the public record in the jurisdiction where the mortgage would be recorded. h. A licensee has a reasonable basis to believe that an individual's telephone number is lawfully made available to the general public if the licensee has located the telephone number in the telephone book or the consumer has informed you that the telephone number is not unlisted. § 114-57-9. Limits on Disclosure of Nonpublic Personal Financial Information to Nonaffiliated Third Parties. 9.1. Except as otherwise authorized in this rule, a licensee may not, directly or through any affiliate, disclose any nonpublic personal financial information about a consumer to a nonaffiliated third party unless: a. The licensee has provided to the consumer an initial notice as required under section 3; b. The licensee has provided to the consumer an opt-out notice as required in section 6; c. The licensee has given the consumer a reasonable opportunity, before it discloses the information to the nonaffiliated third party, to opt out of the disclosure; and d. The consumer does not opt out. e. A licensee provides a consumer with a reasonable opportunity to opt out if: 1. The licensee mails the notices required in subdivisions a and b of this subsection to the consumer and allows the consumer to opt out by mailing a form, calling a toll-free telephone number, or any other reasonable means, within thirty (30) days from the date the licensee mailed the notices. 2. A customer opens an on-line account with a licensee and agrees to receive the notices required in subdivisions a and b of this subsection electronically, and the licensee allows the customer to opt out by any reasonable means within thirty (30) days after the date that the customer acknowledges receipt of the notices in conjunction with opening the account. 3. For an isolated transaction, such as providing the consumer with an insurance quote, the licensee provides the notices required in subdivisions a and b of this subsection at the time of the transaction and requests that the consumer decide, as a necessary part of the transaction, whether to opt out before completing the transaction. 9.2. A licensee shall comply with this section, regardless of whether the licensee and the consumer have established a customer relationship. 9.3. Unless a licensee complies with this section, the licensee may not, directly or through any affiliate, disclose any nonpublic personal financial information about a consumer that the licensee has collected, regardless of whether the licensee collected it before or after receiving the direction to opt out from the consumer. 9.4. A licensee may allow a consumer to select certain nonpublic personal financial information or certain nonaffiliated third parties with respect to which the consumer wishes to opt out. § 114-57-10. Limits on Redisclosure and Reuse of Nonpublic Personal Financial Information. Rev. 04-2014 CHD/P&S/alr Page 13 10.1. If a licensee receives nonpublic personal financial information from a nonaffiliated financial institution under an exception in sections 13 or 14 of this rule, the licensee's disclosure and use of that information is limited as follows: a. The licensee may disclose the information to the affiliates of the financial institution from which the licensee received the information; b. The licensee may disclose the information to its affiliates, but the licensee's affiliates may, in turn, disclose and use the information only to the extent that the licensee may disclose and use the information; and c. The licensee may disclose and use the information pursuant to an exception in sections 13 or 14 of this rule, in the ordinary course of business to carry out the activity covered by the exception under which the licensee received the information. 10.2. If a licensee receives information from a nonaffiliated financial institution for claims settlement purposes, the licensee may disclose the information for fraud prevention or in response to a properly authorized subpoena. The licensee may not disclose that information to a third party for marketing purposes or use that information for its own marketing purposes. 10.3. If a licensee receives nonpublic personal financial information from a nonaffiliated financial institution other than under an exception in sections 13 or 14 of this rule, the licensee may disclose the information only: a. To the affiliates of the financial institution from which the licensee received the information; b. To its affiliates, but its affiliates may, in turn, disclose the information only to the extent that the licensee may disclose the information; and c. To any other person, if the disclosure would be lawful if made directly to that person by the financial institution from which the licensee received the information. 10.4. If a licensee obtains a customer list from a nonaffiliated financial institution outside of the exceptions in sections 13 or 14: a. The licensee may use that list for its own purposes; and b. The licensee may disclose that list to another nonaffiliated third party only if the financial institution from which the licensee purchased the list could have lawfully disclosed the list to that third party. That is, the licensee may disclose the list in accordance with the privacy policy of the financial institution from which the licensee received the list, as limited by the opt-out direction of each consumer whose nonpublic personal financial information the licensee intends to disclose, and the licensee may disclose the list in accordance with an exception in sections 13 or 14, such as to the licensee's attorneys or accountants. 10.5. If a licensee discloses nonpublic personal financial information to a nonaffiliated third party under an exception in sections 13 or 14 of this rule, the third party may disclose and use that information only as follows: a. The third party may disclose the information to the licensee's affiliates; b. The third party may disclose the information to its affiliates, but its affiliates may, in turn, disclose and use the information only to the extent that the third party may disclose and use the information; and c. The third party may disclose and use the information pursuant to an exception in sections 13 or 14 in the ordinary course of business to carry out the activity covered by the exception under which it received the information. 10.6. If a licensee discloses nonpublic personal financial information to a nonaffiliated third party other than under an exception in sections 13 or 14 of this rule, the third party may disclose the information only: Rev. 04-2014 CHD/P&S/alr Page 14 a. To the licensee's affiliates; b. To the third party's affiliates, but the third party's affiliates, in turn, may disclose the information only to the extent the third party can disclose the information; and c. To any other person, if the disclosure would be lawful if the licensee made it directly to that person. § 114-57-14. Other Exceptions to Notice and Opt-Out Requirements for Disclosure of Nonpublic Personal Financial Information. 14.1. The requirements for initial notice to consumers in subdivision b of subsection 3.1, opting out in sections 6 and 9, and service providers and joint marketing in section 12 do not apply when a licensee discloses nonpublic personal financial information: a. With the consent or at the direction of the consumer, provided that the consumer has not revoked the consent or direction; b. To protect the confidentiality or security of a licensee's records pertaining to the consumer, service, product or transaction; c. To protect against or prevent actual or potential fraud or unauthorized transactions; d. For required institutional risk control or for resolving consumer disputes or inquiries; e. To persons holding a legal or beneficial interest relating to the consumer; or f. To persons acting in a fiduciary or representative capacity on behalf of the consumer; g. To provide information to insurance rate advisory organizations, guaranty funds or agencies, agencies that are rating a licensee, persons that are assessing the licensee's compliance with industry standards, and the licensee's attorneys, accountants and auditors; h. To the extent specifically permitted or required under other provisions of law and in accordance with the federal Right to Financial Privacy Act of 1978 (12 U.S.C. 3401 et seq.), to law enforcement agencies (including the Federal Reserve Board, Office of the Comptroller of the Currency, Federal Deposit Insurance Corporation, Office of Thrift Supervision, National Credit Union Administration, the Securities and Exchange Commission, the Secretary of the Treasury, with respect to 31 U.S.C. Chapter 53, Subchapter II (Records and Reports on Monetary Instruments and Transactions) and 12 U.S.C. Chapter 21 (Financial Record keeping), a state insurance authority, and the Federal Trade Commission), self-regulatory organizations or for an investigation on a matter related to public safety; i. To a consumer reporting agency in accordance with the federal Fair Credit Reporting Act (15 U.S.C. 1681 et seq.); or j. From a consumer report reported by a consumer reporting agency; k. In connection with a proposed or actual sale, merger, transfer or exchange of all or a portion of a business or operating unit if the disclosure of nonpublic personal financial information concerns solely consumers of the business or unit; l. To comply with federal, state or local laws, rules and other applicable legal requirements; m. To comply with a properly authorized civil, criminal or regulatory investigation, or subpoena or summons by federal, state or local authorities; or Rev. 04-2014 CHD/P&S/alr Page 15 n. To respond to judicial process or government regulatory authorities having jurisdiction over a licensee for examination, compliance or other purposes as authorized by law; or o. For purposes related to the replacement of a group benefit plan, a group health plan or a group welfare plan. 14.2. A consumer may revoke consent by subsequently exercising the right to opt out of future disclosures of nonpublic personal information as permitted under subsection 6.10. § 114-57-15. When Authorization Required for Disclosure of Nonpublic Personal Health Information. 15.1. A licensee shall not disclose nonpublic personal health information about a consumer or customer unless an authorization is obtained from the consumer or customer whose nonpublic personal health information is sought to be disclosed. 15.2. Nothing in this section shall prohibit, restrict or require an authorization for the disclosure of nonpublic personal health information by a licensee for the performance of the following insurance functions by or on behalf of the licensee: claims administration; claims adjustment and management; detection, investigation or reporting of actual or potential fraud, misrepresentation or criminal activity; underwriting; policy placement or issuance; loss control; rate-making and guaranty fund functions; reinsurance and excess loss insurance; risk management; case management; disease management; quality assurance; quality improvement; performance evaluation; provider credentialing verification; utilization review; peer review activities; actuarial, scientific, medical or public policy research; grievance procedures; internal administration of compliance, managerial, and information systems; policyholder service functions; auditing; reporting; database security; administration of consumer disputes and inquiries; external accreditation standards; the replacement of a group benefit plan; activities in connection with a sale, merger, transfer or exchange of all or part of a business or operating unit; any activity that permits disclosure without authorization pursuant to the federal Health Insurance Portability and Accountability Act privacy rules promulgated by the U.S. Department of Health and Human Services; disclosure that is required, or is one of the lawful or appropriate methods, to enforce the licensee's rights or the rights of other persons engaged in carrying out a transaction or providing a product or service that a consumer requests or authorizes; and any activity otherwise permitted by law, required pursuant to governmental reporting authority, or to comply with legal process. Additional insurance functions may be added with the approval of the commissioner to the extent they are necessary for appropriate performance of insurance functions and are fair and reasonable to the interest of consumers. § 114-57-16. Authorizations. 16.1. A valid authorization to disclose nonpublic personal health information pursuant to subsection 15.1 shall be in written or electronic form and shall contain all of the following: a. The identity of the consumer or customer who is the subject of the nonpublic personal health information; b. A general description of the types of nonpublic personal health information to be disclosed; c. General descriptions of the parties to whom the licensee discloses nonpublic personal health information, the purpose of the disclosure and how the information will be used; d. The signature of the consumer or customer who is the subject of the nonpublic personal health information or the individual who is legally empowered to grant authority and the date signed; and e. Notice of the length of time for which the authorization is valid, which in no event shall be for more than twenty-four (24) months, and that the consumer or customer may revoke the authorization at any time and the procedure for making a revocation. 16.2. A consumer or customer who is the subject of nonpublic personal health information may revoke an authorization to disclose nonpublic personal health information at any time, subject to the rights of an individual who acted in reliance on the authorization prior to notice of the revocation. Rev. 04-2014 CHD/P&S/alr Page 16 16.3. A licensee shall retain the authorization or a copy thereof in the record of the individual who is the subject of nonpublic personal health information. § 114-57-17. Authorization Request Delivery. 17.1. A request for authorization and an authorization form may be delivered to a consumer or a customer as part of an opt-out notice pursuant to section 8, provided that the request and the authorization form are clear and conspicuous. An authorization form is not required to be delivered to the consumer or customer or included in any other notices unless the licensee intends to disclose protected health information pursuant to subsection 15.1. SERIES 63 STANDARD MOTOR VEHICLE POLICY PROVISIONS § 114-63-1. General. 1.1. Scope. This rule establishes the standard motor vehicle insurance policy provisions as required by W. Va. Code § 33-6-31(i). § 114-63-2. Definitions. 2.1. “Motor Vehicle“ means a car, auto, or other synonym as such word is defined in the policy. 2.2. “Underinsured Motor Vehicle“ means a motor vehicle with respect to the ownership, operation or use of which there is liability insurance applicable at the time of the accident but the limits actually available to the injured person in question are less than the total amount of damages sustained by the injured person regardless of the comparison between such liability insurance limits actually available and the underinsured motorist coverage limits. 2.3. “Uninsured Motor Vehicle“ means a motor vehicle as to which there is no: a. Bodily injury liability insurance and property damage liability insurance, or b.There is such insurance, but the insurance company writing the same denies coverage thereunder; and c. There is no certificate of self insurance. A motor vehicle shall be deemed to be uninsured if the owner or operator thereof be unknown. W. Va. Code § 33-631(c). A motor vehicle shall also be deemed to be uninsured if there has been a valid bodily injury or property damage liability policy issued upon such vehicle but the policy is uncollectible, in whole or in part, by reason of the insurance company being insolvent or having been placed in receivership. W. Va. Code § 33-6-31(j). § 114-63-3. Liability Insurance Provisions. 3.1. All motor vehicle liability policies shall contain a provision insuring the named insured and any other person responsible for the use of or using the motor vehicle with the consent, express or implied, of the named insured or his or her spouse. W. Va. Code § 33-6-31(a). 3.2. All motor vehicle liability policies shall contain a provision insuring against liability for death or bodily injury sustained, or loss or damage occasioned, as a result of negligence in the ownership, maintenance or use of the vehicle. W. Va. Code § 33-6-31(a). 3.3. All motor vehicle liability policies shall contain a provision providing primary coverage to the named insured and to any other person who normally operates the covered vehicle, if he or she is instead operating a motor vehicle Rev. 04-2014 CHD/P&S/alr Page 17 owned by one engaged in the business of selling, repairing, leasing or servicing motor vehicles, without separate consideration, while the insured's motor vehicle is in the custody of one engaged in said business of selling, repairing, leasing or servicing motor vehicles. W. Va. Code § 33-6-29. 3.4. All motor vehicle liability policies shall contain coverage for liability under the family purpose doctrine. W. Va. Code § 33-6-31(a). 3.5. Motor vehicle liability policies shall not contain family member exclusions. 3.6. Motor vehicle liability policies shall not contain terms for cancellation or non-renewal less favorable to the insured than those set forth in W. Va. Code § 33-6A. 3.7. Motor vehicle liability policies shall not contain any condition, stipulation or agreement requiring the policy to be construed according to the laws of any other state or country, except as necessary to meet the requirements of the motor vehicle financial responsibility laws or compulsory disability benefit laws of such other state or country. W. Va. Code § 33-6-14. 3.8. Motor vehicle liability policies shall not contain any condition, stipulation or agreement limiting the time within which a claim may be brought to less than two years from the time the cause of action accrues. W. Va. Code § 33-614. 3.9. Motor vehicle liability policies may contain a provision excluding coverage for the negligence of a driver operating the motor vehicle without the consent, express or implied, of the named insured (or his or her spouse). 3.10. Motor vehicle liability policies may contain a provision with respect to the negligence of any bailee for hire. W. Va. Code § 33-6-31(a). 3.11. Motor vehicle liability policies may contain an exclusion for intentional torts above the minimum financial liability limits under W. Va. Code § 17D-4-2. 3.12. Motor vehicle liability policies may contain a restricted named driver exclusion endorsement above the minimum financial liability limit under W. Va. Code § 17D-4-2. The restricted named driver exclusion must specifically designate by name the individual or individuals to be excluded. 3.13. Motor vehicle liability policies may contain a provision which precludes stacking. 3.14. Motor vehicle liability policies may contain a “duty to cooperate“ clause provided that before an insurance policy will be voided because of the insured's failure to cooperate, the failure must be substantial and of such nature as to prejudice the insurer's rights. 3.15. Any coverage issued under a substandard risk motor vehicle insurance policy shall contain the notice set forth in W. Va. Code § 33-6-31c. § 114-63-4. Uninsured Motor Vehicle Insurance Provisions. 4.1. All motor vehicle policies shall contain a provision undertaking to pay the insured all sums which he or she shall be legally entitled to recover as damages from the owner or operator of an uninsured motor vehicle up to the limit selected by the named insured on a properly completed form pursuant to W. Va. Code § 33-6-31d. 4.2. Uninsured motor vehicle coverage shall not contain family member exclusions. 4.3. Uninsured motor vehicle coverage shall not contain a provision requiring arbitration. W. Va. Code § 33-6-31(g). 4.4. Uninsured motor vehicle coverage may contain a provision excluding the first three hundred dollars of property damage but shall not contain any other deductible or setoff up to the limits of the uninsured motorist coverage. W. Va. Code § 33-6-31(b). Rev. 04-2014 CHD/P&S/alr Page 18 4.5. Uninsured motor vehicle coverage may contain a provision requiring that the insured use reasonable diligence, upon learning that the tortfeasor is uninsured, to provide notice of any potential uninsured motor vehicle claim within a reasonable period of time. 4.6. Uninsured motor vehicle coverage may contain an “owned but not insured exclusion“ precluding benefits above the minimum financial responsibility limits contained in W. Va. Code § 17D-4-2. 4.7. Uninsured motor vehicle coverage may contain a provision excluding benefits for injuries which result from a motor vehicle collision which occurs within the course and scope of employment but only with respect to fault of the employer or co-employee and not with regard to the fault of a third party. 4.8. With regard to uninsured motor vehicle coverage in the event of negligence by an unknown tortfeasor, the policy may contain a provision requiring a close and substantial physical nexus between the unidentified hit and run vehicle and the insured vehicle. “Close and Substantial Physical Nexus“ means evidence which can be established by independent third-party testimony to the satisfaction of the trial judge and the jury that, but for the immediate evasive action of the insured, direct physical contact would have incurred between the unknown motor vehicle and the victim. 4.9. Uninsured motor vehicle coverage may contain a provision providing for the right of subrogation against the tortfeasor up to the amount paid under the uninsured motor vehicle endorsement, consistent with W. Va. Code § 336-31(f). 4.10. Uninsured motor vehicle coverage may include an exclusion for punitive damage liability. § 114-63-5. Underinsured Motor Vehicle Provisions. 5.1. If selected by the insured, policies must include a provision agreeing to pay the insured all sums which he or she shall be legally entitled to recover as damages from the owner or operator of an underinsured motor vehicle up to the limits selected by the insured. W. Va. Code § 33-6-31(b). 5.2. Underinsured motor vehicle coverage shall not provide for setoff for any payments made by the insured's policy or any other policy. W. Va. Code § 33-6-31(b). 5.3. Underinsured motor vehicle coverage shall not contain a provision requiring arbitration. W. Va. Code § 33-631(g). 5.4. Underinsured motor vehicle coverage may contain a provision requiring that the insured use reasonable diligence, upon learning that the tortfeasor is underinsured, to provide notice of any potential underinsured motorist claim within a reasonable period of time. 5.5. Underinsured motor vehicle coverage may contain a provision requiring notice of any settlement with the liability carrier consistent with W. Va. Code § 33-6-31e. 5.6. Underinsured motor vehicle coverage may contain a provision excluding benefits for injuries which result from a motor vehicle collision which occurs within the course and scope of employment but only with respect to the fault of the employer or co-employee and not with regard to the fault of a third party. 5.7. With regard to underinsured motor vehicle coverage in the event of negligence by an unknown tortfeasor, the policy may contain a provision requiring a close and substantial physical nexus between the unidentified hit and run vehicle and the insured vehicle. “Close and Substantial Physical Nexus“ means evidence which can be established by independent third party testimony to the satisfaction of the trial judge and the jury that, but for the immediate evasive action of the insured, direct physical contact would have incurred between the unknown vehicle and the victim. 5.8. Underinsured motor vehicle coverage may contain a provision providing for the right of subrogation against the tortfeasor, up to the amount paid under the underinsured motor vehicle endorsement, consistent with W. Va. Code § Rev. 04-2014 CHD/P&S/alr Page 19 33-6-31(f). 5.9. Underinsured motor vehicle coverage may contain family member or similar exclusion precluding a guest passenger from collecting such benefits with respect to the negligence of the driver of the motor vehicle in which he or she is riding but such guest passenger may not be precluded from recovery of underinsured benefits with respect to the negligence of a third party. 5.10. Underinsured motor vehicle coverage may contain a provision precluding intra-policy stacking and inter-policy stacking. 5.11. Underinsured motor vehicle coverage may contain a family use exclusion to be applied when a passenger family member receives payment under the liability provisions with respect to the negligence of his or her driver thereby preventing the underinsured coverage from being converted into additional liability coverage. 5.12. Underinsured motor vehicle coverage may include a provision precluding recovery of underinsured benefits if the liability coverage of the tortfeasor with respect to whose negligence benefits are sought has not been exhausted. 5.13. Underinsured motor vehicle coverage may include a provision precluding benefits if the claimant is in an owned but not insured motor vehicle. 5.14. Underinsured motor vehicle coverage may include an exclusion for punitive damage liability. SERIES 71 INSURANCE FRAUD PREVENTION § 114-71-1. General. 1.1. Scope. -- This legislative rule establishes standards for reporting insurance fraud. § 114-71-2. Designation of Primary Contact. 2.1. Every insurer shall designate at least one (1) primary contact person but not more than four (4) primary contact persons who shall communicate with the Insurance Fraud Unit on matters relating to the reporting, investigation, and prosecution of suspected fraudulent insurance acts. 2.2. Every insurer shall notify the Insurance Fraud Unit in writing of the names, titles, addresses, and telephone numbers of the insurer's primary contact person or persons. Any changes to information relating to the contact person or persons must be reported to the Insurance Fraud Unit within ten (10) days of the changes. § 114-71-3. Reporting of Insurance Fraud or Criminal Offenses Otherwise Related to the Business of Insurance. 3.1. All persons identified in W. Va. Code '33-41-5(a) shall report in writing all suspected fraudulent insurance acts to the Insurance Fraud Unit. 3.2. The report shall be filed with the Insurance Fraud Unit within fourteen (14) days of the determination by the reporter that a suspected fraudulent insurance act has been committed. 3.3. When a suspected fraudulent insurance act is reported, the following information, if known, shall be reported to the Insurance Fraud Unit: a. Date of preparation of the report. b. The following information about the reporting insurance company: Rev. 04-2014 CHD/P&S/alr Page 20 1. Name of insurance company; 2. Telephone number and fax number of insurance company; 3. Policy number or claim number; and 4. Insurance policy type. c. The following information about the reporting person if not an insurance company: 1. Complete name; 2. Occupation and title; 3. Complete address; and 4. Telephone number and fax number. d. The following information about the loss or occurrence: 1. Date of loss or occurrence; 2. Location of loss including the complete address; 3. Estimated value of claim for loss; and 4. Whether claim was paid or not paid. e. The following information concerning the parties involved and their roles: 1. Complete names of all parties; 2. Business and alias names of parties; 3. Roles of each party; 4. Complete address of each party; 5. Phone number of each party; 6. Date of birth or age of each party; 7. Social Security number of each party; 8. Tax identification number of each party; and 9. Driver's license number of each party. f. A detailed narrative of what fraudulent insurance act is suspected and the circumstances leading to the suspicion of fraud. g. A list of the type of documents in the possession of the reporter, for example police reports, photographs, or falsified documents, supporting the suspicion of fraud. h. Any other agency or entity to which the reporter has reported suspected fraud, including the name, address, and telephone number of the other agency. Rev. 04-2014 CHD/P&S/alr Page 21 3.4. The report provided must be signed and dated by the reporting party or an authorized representative of the reporting party. 3.5. The required information shall be submitted on a form prescribed by the commissioner. Rev. 04-2014 CHD/P&S/alr