Conscious-Sedation
advertisement

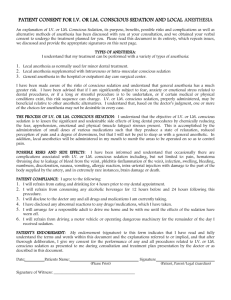
Policy: Owner: Initiated: Version: Last Approval Date: Reference: 1.0 Conscious Sedation CNO, Anesthesia Department, Medical Staff 08/2010 2 8/2012 S. Smith, D. Duell, B. Martin, Clinical Nursing Skills, Basic to Advanced Skills, (8th ed) 2011. Statement on Safe Use of Propofol; Committee of Origin: Ambulatory Surgical Care (Approved by the ASA House of Delegates on October 27, 2004, and amended on October 21, 2009). Standards for Basic Anesthetic Monitoring– Committee of Origin: Standards and Practice Parameters. (Approved by the ASA House of Delegates on October 21, 1986, and last amended on October 20, 2010 with an effective date of July 1, 2011.). Joint Commission Standards (2012): PI.01.01.01, PC.03.01.01, PC.03.01.03, PC.03.01.05, PC 03.01.07 DEFINITIONS 1.1 Minimal Sedation: Minimal Sedation (anxiolysis) is a drug-induced state in which patients respond normally to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected. Medication used for this purpose and for sedation of mechanically ventilated patients or for urgent/emergent endotracheal intubation is covered by separate protocols. 1.2 Moderate Sedation/Analgesia: Moderate Sedation/Analgesia (conscious sedation) is defined as a drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patient airway and spontaneous ventilation is adequate. Cardiovascular function is usually maintained. 1.3 Deep Sedation/Analgesia: Deep Sedation/Analgesia is a drug-induced depression of consciousness during which patients can’t be easily aroused but respond purposefully following repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance to maintain a patent airway, and spontaneous ventilation may be inadequate. Cardiovascular function is usually maintained. Deep sedation and anesthesia is restricted to use by an anesthesia provider. 1.4 Anesthesia: Consists of general anesthesia and spinal or major regional anesthesia. It does not include local anesthesia. General anesthesia is a drug-induced loss of consciousness during which patients are not arousable, even by painful stimulation. The ability to independently maintain ventilatory function if often impaired. Patients often require assistance in maintaining a patent airway, and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of neuromuscular function. Cardiovascular function may be impaired. 2.0 POLICY 2.1 The Chairman of Anesthesia assists in establishing guidelines to insure that conscious sedation is administered in a safe and appropriate manner consistent with the patient’s needs. 2.2 This policy applies to all departments administering conscious sedation. 2.3 Conscious sedation will only be administered in appropriate settings where facilities, competent personnel and all necessary equipment is available for any foreseeable emergency situation. 2.3.1 The administration of Propofol and monitoring of patients receiving Propofol is restricted to the following departments and associated staff: Department of Anesthesia (Physicians, CRNAs); Emergency Department (Physicians, MidLevel Providers, RNs); Intensive Care (Physicians, Mid-Level Providers, RNs); and in clinical settings where the patient is intubated and receiving a continuous infusion of Propofol (i.e., ICU, ED, PACU, or during the transport of a patient to another setting) 2.4 Only staff that have successfully completed the Conscious Sedation Competency requirements and meet the ongoing competency requirements will administer conscious sedation. 2.4.1 Physician requirements (non-anesthesiologists) Non-anesthesiologists physicians who administer conscious sedation/ analgesia must be ACLS certified and meet the credentialing requirements of the medical staff required for conscious sedation administration. 2.4.2 Nursing requirements: 2.3.2.1 Maintain BLS and ACLS certification. PALS is required for those administering pediatric conscious sedation. 2.3.2.2 Knowledge of cardiac rhythm identification 2.3.2.3 Completion of annual conscious sedation competency 2.5 The physician/LIP administering conscious sedation is responsible for obtaining consent. 2.6 Consult the Anesthesia Department for those patients who are at risk for losing protective reflexes during conscious sedation. 2.7 Patients classified as ASA IV or ASA V should be considered for Monitored Anesthesia Care (MAC) rather than conscious sedation if a procedure is to be performed outside the Intensive Care Unit or the Emergency Department. 3.0 PROCEDURE: 3.1 Propofol Specifics 1 Due to the potential for rapid, profound changes in sedative/anesthetic depth and the lack of antagonist medications, agents such as propofol require special attention. Even if moderate sedation is intended, patients receiving propofol should receive care consistent with that required for deep sedation. 3.2 3.1.1 Procedural Propofol should be administered only by persons trained in the administration of general anesthesia, who are not involved in the conduct of the surgical/diagnostic procedure. 3.1.2 Continuous infusion of Propofol for the intubated patient requires continuous hemodynamic monitoring by competent staff trained in deep conscious sedation. 3.1.3 During the administration of Propofol, patients should be monitored without interruption to assess level of consciousness, and to identify early signs of hypotension, bradycardia, apnea, airway obstruction and/or oxygen desaturation. 3.1.4 Monitoring for the presence of exhaled carbon dioxide should be utilized (unless invalidated by the nature of the patient, procedure or equipment) because movement of the chest will not dependably identify airway obstruction or apnea. Conscious Sedation Requirements: 3.2.1 Equipment: All equipment will be available and in demonstrated working capacity. The Bio-medical equipment used shall be inventoried and maintained on a regularly scheduled basis by the hospital’s Biomedical Engineering Department. 3.2.1.1 A self-inflating positive-pressure oxygen delivery system must be immediately available. Various size and age appropriate bag and mask sizes must be available in those areas which care for pediatric patients. 3.2.1.2 Oxygen source, nasal cannula and a non-rebreathing mask 3.2.1.3 Suction source (portable or wall) 3.2.1.4 An emergency cart which should include the necessary age appropriate equipment and drugs to treat any emergency ranging from apnea to cardiac arrest. 3.2.1.5 A pulse oximeter 3.2.1.6 A blood pressure monitor with continuous capability 3.2.1.7 Cardiac monitor 3.2.1.8 During moderate or deep sedation, monitoring for the presence of exhaled carbon dioxide should be utilized (unless invalidated by the nature of the patient, procedure or equipment) because movement of the chest will not dependably identify airway obstruction or apnea.2 1 Statement on Safe Use of Propofol; Committee of Origin: Ambulatory Surgical Care (Approved by the ASA House of Delegates on October 27, 2004, and amended on October 21, 2009) 2 Standards for Basic Anesthetic Monitoring – Committee of Origin: Standards and Practice Parameters. (Approved by the ASA House of Delegates on October 21, 1986, and last amended on October 20, 2010 with an effective date of July 1, 2011.) 3.3 Pre-Procedure 3.3.1 The physician administering conscious sedation will perform a pre-procedure health evaluation and physical assessment and will complete documentation on the Short History and Physical Form or department and/or physician specific forms. 3.3.2 The procedural RN will perform a pre-procedure assessment and will document the following: 3.3.2.1 Baseline Vital Signs (blood pressure, pulse, respiratory rate, color of nail beds, skin color and temperature) 3.3.2.2 Baseline level of consciousness 3.3.2.3 Baseline oxygen saturation 3.3.2.4 Drug allergies 3.3.2.5 Medication history 3.3.2.6 Relevant medical/surgical history 3.3.2.7 NPO status 3.3.2.8 Ability of the patient to communicate 3.3.2.9 Baseline EKG strip 3.3.2.10 Weight in kilograms 3.3.2.11 Pain Assessment 3.3.3 Determination of Pregnancy status is required in all females. 3.3.3.1 3.3.3.2 Obtain LMP and applicable gynecologic history. Based on the information obtained in 3.3.3.1 pregnancy a test will be performed at the physician’s discretion. 3.3.4 Verify informed consent has been obtained and is completed. 3.3.5 Establish IV access or establish patency of an existing IV in all patients undergoing conscious sedation (even in oral sedation cases). 3.3.6 Initiate discharge teaching prior to sedation. 3.4 Intra Procedure 3.4.1 “Time-Out” verification shall be performed prior to the start of medication. 3.4.2 Continuous oxygen via nasal cannula. 3.4.3 Blood pressure, pulse and respirations every 5 minutes or more frequent if needed. 3.4.4 Continuously monitor cardiac rate and rhythm, pulse oximetry and ETCO2 (when used) 3.4.5 Assess patient’s ability to manage secretions, suction as necessary 3.4.6 Observe for patient’s response to medication and for physiological and psychological changes. Report to MD any changes in level of consciousness, restlessness, cyanosis, pallor, flushing, allergic reaction, N/V. 3.4.7 Document administration time of all medications and agents administered. Continually assess the patient’s response to medications and procedure. 3.5 Immediate Post Procedure (or after the last dose of medication was given) 3.5.1 The RN will remain with the patient until Discharge or Transfer criteria is met. 3.5.2 Assess patient’s pain level, level of sedation and tolerance of procedure. 3.5.3 Vital signs will be obtained a minimum of q15x3 (initial set, 15 min later and 30 minutes after the first set) or more frequently if necessary. Pulse oximetry will be monitored accordingly or until pre-procedure level is reached. If a reversal agent is required the patient must be monitored for no less than 60 minutes. 3.5.4 Prior to discontinuation of the monitoring, the patient’s vital signs must return to within 20% of baseline for 2 consecutive readings. The patient must achieve an Aldrete score of 8 or return to baseline assessment if initially impaired. 3.5.5 Patients must meet Discharge/Transfer criteria stated below, prior to leaving the Post-procedure area. 3.6 Inpatient Transfer and Discharge to Home Criteria 3.6.1 3.6.2 Patients who meet the following criteria may be transported by non-licensed personnel to the receiving department after report has been given to the accepting Nurse. 3.6.1.1 Vital signs are stable, within 20% of baseline for 2 consecutive readings. 3.6.1.2 Level of consciousness returned to pre-procedure level. 3.6.1.3 Aldrete score is 8 or at pre-procedure baseline. 3.6.1.4 Patient and/or responsible party can verbalize an understanding of postprocedure instructions. 3.6.1.5 Pain comfort goal is met with or without medications. 3.6.1.6 If applicable, bleeding is controlled. Other Discharge Criteria to be met by Out-Patients 3.6.2.1 Discharge should be no sooner than 30 minutes after administration of and/or no sooner than one hour after administration of reversal medication. 3.6.2.2 Patient will tolerate fluids with minimal nausea and without vomiting. 3.6.2.3 Patient will be able to ambulate to the level he/she did pre-procedure and the IV will be removed following ambulation. 3.6.2.4 Discharge instructions for conscious sedation and post procedure instructions will be reviewed. Understanding will be demonstrated by the patient and/or responsible party and their signature will be obtained. 4.0 3.6.2.5 Transportation home will be verified. 3.6.2.6 Patient should have family, significant other, or friends available to observe and/or assist at home for the first 24 hours. DOCUMENTATION 4.1 The Conscious Sedation Flow sheet will be completed. (Exception: Some departments (e.g., Interventional Radiology, Endoscopy and others will utilize their individual flow sheets. It has been established that these flow sheets meet minimum documentation requirements as outlined by this policy- see individual units for those flow sheets). 4.2 Post-procedure report will be given to a licensed professional on all patients returning or relocating to another nursing setting. 4.3 The Discharge Instructions will be reviewed with the patient and/or their representative and all signatures obtained. Attachments: Conscious Sedation Flowsheet Medication Reference Sheet Moderate Sedation Monitoring - Data Collection Form Conscious Sedation Flow sheet (developed 2/08: Revised 3/10, 7/12) Date:_________________MD:_________________________ RN:____________________________ Other:___________________________ Last PO intake: food _______________________ liquids________________________ Weight:_____________ LMP:___________________ Consent for procedure signed [ ] Consent for conscious sedation signed [ ] Equipment checked, emergency equipment available [ ] Ride Home verified [ ] Name: _________________________________________ Phone: ___________________________________________ Medications and last dose: or [ ] see medication reconciliation sheet or [ ]see MAR _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ Allergies and reaction: ______________________________________________________________________________________ IV site / solution ___________________________________________________________________________________________ Hx of Moderate Sedation and/or Anesthesia Reaction [ ] YES [ ] NO ASA score: __________( see back of this page) comments_________________________________________________________________________ Baseline VS: Time______ O2 Delivery Procedure Information BP _______ O2 sat (Room air) ____ []Cannula _____L/ml Procedure:_________________ HR _______ Aldrete score:_________ []Mask _____L/ml Start time:________ RR _______ []Vent End time:________ Time out: Correct patient /procedure/site/laterality verified. Time:_______________________ Staff present:__________________________________________________________________ Medications / dose Time BP / HR / Resp SpO2 Rhythm Pain Response/Assessment Total meds: _____________________________________________________________________ Comments: MD signature: (for meds given) Aldrete Score Activity: able to move, voluntarily or on command Moves 4 extremities Moves 2 extremities Moves 0 extremities Corculation BP+/- 20% pre-sedation level BP+/- 20-50% BP+/- 50% or > Oxygen saturation Saturation >92% Requires o2 to maintain SpO2 >92% SpO2 is <92% with O2 Fully awake Arousable Failure to elicit response Color is pink Pale dusky Frank cyanosis Post Procedure (q15 min x 3 minimum, after last dose of meds) Time BP / HR /R SpO2 Pain Aldrete Comments =2 =1 =0 =2 =1 =0 =2 =1 =0 =2 =1 =0 =2 =1 =0 D/C or transfer vital signs: Report given to: Time: RN signature: Z/patient care services/lori karols folder/forms & attachments/conscious sedation – common.ech.0097 Conscious sedation Flowsheet page 2 POST PROCEDURE NOTE Patients tolerance of procedure: ______________________________________________________________________________________ Procedure Results______________________________________________________________________ _____________________________________________________________________________________ ______________________________________________________________________________________ Specimen Removed:___________ _____________________________________________ [ ] Not applicable Sent to lab: ________________________________________________________________ [ ] Not applicable Estimated Blood Loss: _______________________________________________________ [ ] Not applicable Condition: __________________________________________________________________________________ Monitoring may be discontinued and the patient may be discharged to home or appropriate unit when the Aldrete score is at least 8 or upon a specific physician’s order. Monitoring may be discontinued when the Aldrete score is at least 8 or upon a specific physician’s order. Please call Dr. for further orders or for discharge to home or other unit. Nursing notes: [ ] No comments necessary _______________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ ________________________________________________________________ IV D'C'd [ ] dressing applied [ ] Discharged via [ ] wheelchair [ ] ambulatory Accompanied by:_________________________________________________________ Z/patient care services/lori karols folder/forms & attachments/conscious sedation – common.ech.0098 Patient label Moderate Sedation Monitoring - Data Collection Form Please complete for ALL moderate sedation charts and forward to the Quality/Performance Improvement Department by the 5th of the following month. 1. Please check department (All departments will do 10 charts per month plus all adverse events) Endoscopy Radiology ADS Pain Management ED ICU 2. Date: _________________ 3. Physician Name _______________________ 4. Procedure: ______________________ 5. Screener: _______________________ 6. Please check all moderate sedation charts for documentation of the following. Consent for procedure and anesthesia obtained Pre-procedure assessment completed Pre-induction re-evaluation completed (re-evaluation time, BP, pulse, pulse ox) Vital signs Q5 min during procedure Discharge vital signs __________ Procedure start time (time instrumentation contacts patient) __________ Procedure end time (time instrumentation contacts patient) 7. Adverse Events: Unplanned Critical Care or hospital admission not due to procedure findings Reversal agent used (please note agent) ________________________________ Pre-op unplanned anesthesia consult Post-op unplanned anesthesia consult Ambu / Mechanical Ventilation Cardiopulmonary Arrest Assist ventilation required Allergic drug reaction Pre-procedure assessment not completed. STOP HERE: FOR REVIEWER USE ONLY of unplanned Critical Care or hospital admission not due to procedure findings or if Reversal agent used Comments: ___________________ Reviewer Signature __________________ Review Date Z/patient care services/lori karols folder/forms & attachments/conscious sedation Medication Fentanyl (Sublimaze) Action Onset/Duration Narcotic Onset: IV 1-3 min Duration: 30-60 min Usual ADULT Dose Procedural sedation, For analgesia: 0.5 to 1.5 mcg/kg IV; may repeat every 1 to 3 minutes to desired effect Usual PEDIATRIC Dose For analgesia: 0.5 to 1 mcg/kg IV (up to 50 mcg/dose); may repeat every 3 minutes to desired effect Reversal Agent Considerations/ Side Effects Naloxone (Narcan) Inject slowly over 3-5 min. Rapid injection may cause skeletal muscle and chest wall rigidity, impaired ventilation, Laryngospasm To provide sedation for minor procedures in children 1 to 3 years old, the recommended dose is 2 to 3 micrograms/kilogram/dose, which may be repeated 30 to 60 minutes Side EffectsNausea/Vomiting, Confusion, Dyspnea, Constipation, Backache, Dizziness, Headache, Tachyarrhythmia, Muscle rigidity Children 3 to 12 years of age should receive 1 to 2 mcg/kg/dose Older children should receive 0.5 to 1 mcg/kg/dose; these doses may be repeated every 30 to 60 minutes as needed Meperidine (Demerol) Narcotic Onset: IV 1-3 min Duration: 30-60 min Pre-medication for procedure: 50 to 100 mg IM/SC 30 to 90 min before start of anesthesia Pre-medication for procedure: 1.1 to 2.2 mg/kg IM/SC up to adult dose 30 to 90 min before start of anesthesia Naloxone (Narcan) Do not use in patients receiving MAO inhibitors or procarbazine (may cause fatal reaction) May have additive CNS depression with antihistamines, and sedative/hypnotics Side EffectsNausea/Vomiting, Hypotension, Respiratory Depression, Seizure, Dizziness Medication Action Onset/Duration Usual ADULT Dose Usual PEDIATRIC Dose Reversal Agent Considerations/ Side Effects Morphine Narcotic Onset: IV Rapid Duration: 2-5hrs Pre-medication for anesthetic procedure: 5 to 15 mg IV administered very slowly Premedication for anesthetic procedure: 0.05 to 0.1 mg/kg IV administered very slowly; MAX 10 mg per dose Naloxone (Narcan) Geriatric patients are more sensitive to the effects of opioid analgesics and may experience side effects and respiratory complications more frequently Administer 2.5-15 mg over 5 min. Rapid administration may lead to increased respiratory depression, hypotension, and circulatory collapse. Respiratory depression is increased when combined with a benzodiazepine Side Effects- Pruritis, Rash, Backache, Nausea/Vomiting, , Respiratory Depression, Urinary retention, Hypotension Lorazepam (Ativan) Benzodia zepine Sedative Onset: IV 15-30 min IM 30-60 min PO 15-60 min Duration: 6-8 hrs IM: 50 mcg (0.05 mg)/kg 2 hr before surgery (not to exceed 4 mg) IV: 44 mcg (0.044 mg)/kg (not to exceed 2 mg) 15-20 min before surgery IM (Children): 0.02-0.09 mg/kg/dose IM (Infants): 0.02-0.09 mg/kg/dose IV (Children): 0.02-0.09 mg/kg/dose; may use smaller doses (0.01-0.03 mg/kg) and repeat q 20 min. IV (Infants): 0.02-0.09 mg/kg/dose; may use smaller doses (0.01-0.03 mg/kg) and repeat q 20 min PO (Children): 0.02-0.09 mg/kg/dose PO (Infants): 0.02-0.09 mg/kg/dose Flumazanil (Romazicon) Administer IM doses deep into muscle mass at least 2 hr before surgery for optimum effect Prior to IV use, Lorazepam injection should be diluted with an equal volume of compatible solution Administer at a rate not to exceed 2 mg/min or 0.05 mg/kg over 2-5 min. Rapid IV administration may result in apnea, hypotension, bradycardia, or cardiac arrest. Geriatric patients CNS reactions are more sensitive to these effects Side Effects-Sedation, Dizziness Medication Midazalam (Versed) Action Sedative/ Amnesic Onset/ Duration Onset: IV 1-5 min IM 15 min PO 10-15 min PR 20-30 min Nasal 3-5 min Duration: 1-4 hr Usual ADULT Dose Usual PEDIATRIC Dose Reversal Agent Considerations/ Side Effects Healthy Adults below 60 years of age; 1 to 2.5 mg IV titrated slowly (max injection rate 1.25 mg/min); wait 2 or more minutes to fully evaluate the sedative effect;; a total dose greater than 5 mg is not usually necessary; patients will require approximately 30% less Midazalam if narcotic premedication or other CNS depressants are used IV: 6 months to 5 years of age; initial dose, 0.05 to 0.1 mg/kg IV over 2-3 minutes, wait an additional 2-3 minutes to fully evaluate the sedative effect before initiating a procedure or repeating a dose; total dose up to 0.6 mg/kg may be necessary; total dose usually does not exceed 6 mg; dose must be reduced in patients premedicated with opioid or other sedative agents 6 to 12 years of age; initial dose, 0.025 to 0.05 mg/kg IV over 2-3 minutes; then wait an additional 2-3 minutes to fully evaluate the sedative effect before initiating a procedure or repeating a dose; total dose up to 0.4 mg/kg may be needed; total dose usually does not exceed 10 mg; dose must be reduced in patients premedicated with opioid or other sedative agents 12 to 16 years of age, 1 to 2.5 mg IV titrated slowly (max infusion rate 1.25 mg/min); wait 2 or more minutes before titrating to fully evaluate the sedative effect; wait an additional 2 or more minutes after each increment to fully evaluate the sedative effect; some patients in this age range will require higher than recommended adult doses; total dose usually does not exceed 10 mg; dose must be reduced in patients premedicated with opioid or other sedatives IM 0.1 to 0.15 mg/kg (up to 0.5 mg/kg IM for more anxious patients); total dose usually does not exceed 10 mg; When combined with an opioid, reduce dose of both agents ORAL : 0.25 to 1 mg/kg ORALLY; max dose 20 mg INTRA-NASAL: 0.2 to 0.6 mg/kg RECTAL: 0.25 to 0.5 mg/kg Flumazanil (Romazicon) Titrate, if necessary, using small increments to the appropriate level of sedation; wait an additional 2 or more minutes after each increment to fully evaluate the sedative effect Patients 60 years of age or older, and debilitated or chronically ill patients; 1 to 1.5 mg IV titrated slowly (max injection rate 0.75 mg/min); wait 2 or more minutes to evaluate the sedative effect; repeat to the appropriate level of sedation (max infusion rate 0.5 mg/min); a total dose greater than 3.5 mg is usually not necessary; patients will require approximately 50% less midazolam than healthy young patients if narcotic premedication or other CNS depressants are used Side Effects- Apnea, Respiratory depression, Hiccoughs, Cough, Nausea/Vomiting Agitation, Somnolence Medication Propofol (Diprivan) Action Anesthetic Onset/ Duration Usual ADULT Dose Usual PEDIATRIC Dose Onset: 40 sec Duration: 3-10 min Procedural sedation: 1 mg/kg IV followed by 0.5 mg/kg every 3 to 5 min as needed for sedation Procedural sedation: 1 mg/kg IV followed by 0.5 mg/kg every 3 to 5 min as needed for sedation Reversal Agent None Considerations/ Side Effects Contraindicated in patients with egg, soy, or peanut allergies Assess respiratory status, pulse, and blood pressure continuously throughout Propofol therapy. Frequently causes apnea lasting ³60 sec. Maintain patent airway and adequate ventilation. Propofol should be used only by individuals experienced in endotracheal intubation, and equipment for this procedure should be readily available. Side EffectsNausea/Vomiting, Involuntary muscle movement, Bradyarrythmia, Hypertension, Priapism, Anaphylaxis Ketamine (Ketalar) Reversal of Benzodiazepines Onset: 1-2 min Duration: 1-4 hrs Usual dose of flumazenil is 0.2 milligram administered IV over 15 seconds. If adequate sedation reversal does not occur after an additional 45 seconds, this dose may be repeated at 1-minute intervals, as needed up to 4 times, to a maximum total dose of 1 milligram. Doses should be based on patient response; most patients respond to doses of 0.6 to 1 milligram Usual dose of flumazenil in children 1 year or older is 0.01 milligram/kilogram (mg/kg; up to 0.2 mg) administered IV over 15 seconds. If adequate anesthesia reversal does not occur after an additional 45 seconds, further injections of 0.01 mg/kg may be repeated at 1 min intervals, as needed up to 4 times. The maximum total dose is 0.05 mg/kg or 1 mg, whichever is lower. N/A Should be administered as a series of small injections and not as a single bolus dose Monitor for return of alertness, reduction in sedation, the ability to comprehend and obey commands, and improvements in time/space orientation. Patients may experience re-sedation and respiratory depression Side Effects- Diaphoresis, dizziness, Headache, Abnormal vision, Agitation, Seizure Medication Action Onset/ Duration Usual ADULT Dose Usual PEDIATRIC Dose Flumazanil (Romazicon) Reversal of Benzodiazepines Onset: 1-2 min Duration: 1-4 hrs Usual dose of flumazenil is 0.2 milligram administered IV over 15 seconds. If adequate sedation reversal does not occur after an additional 45 seconds, this dose may be repeated at 1-minute intervals, as needed up to 4 times, to a maximum total dose of 1 milligram. Doses should be based on patient response; most patients respond to doses of 0.6 to 1 milligram Usual dose of flumazenil in children 1 year or older is 0.01 milligram/kilogram (mg/kg; up to 0.2 mg) administered IV over 15 seconds. If adequate anesthesia reversal does not occur after an additional 45 seconds, further injections of 0.01 mg/kg may be repeated at 1 min intervals, as needed up to 4 times. The maximum total dose is 0.05 mg/kg or 1 mg, whichever is lower. N/A Should be administered as a series of small injections and not as a single bolus dose Monitor for return of alertness, reduction in sedation, the ability to comprehend and obey commands, and improvements in time/space orientation. Patients may experience re-sedation and respiratory depression Side Effects- Diaphoresis, dizziness, Headache, Abnormal vision, Agitation, Seizure Nalaxone (Narcan) Opiate Antagonist Onset: IV 2-3min Duration: 45180 min Reversal of opiate activity, 0.1 to 0.2 mg IV, repeat every 2 to 3 min as needed to desired degree of reversal; may repeat dose within 1 to 2 hr depending on amount and type of opioid and time interval since last opioid administration (Newborn infants) 0.001 mg to 0.015 mg/kg IV/IM, doses may be repeated as needed to maintain opiate reversal (Older infants/children) 0.001 mg to 0.015 mg/kg N/A Observe for re-sedation postoperative patients with preexisting cardiac disease risk pulmonary edema due to a significant shift of blood volume into the pulmonary vascular bed during labor; risk of severe hypertensive episodes in patients with mild to moderate hypertension; monitor blood pressures IV/INTRAOSSEOUS/IM/SUBQ, doses may be repeated as needed to maintain opiate reversal Reversal Agent Considerations/ Side Effects Side Effects- V-Fib, V-tach, Dyspnea Pulmonary Edema, Hypertension