Curriculum Vitae
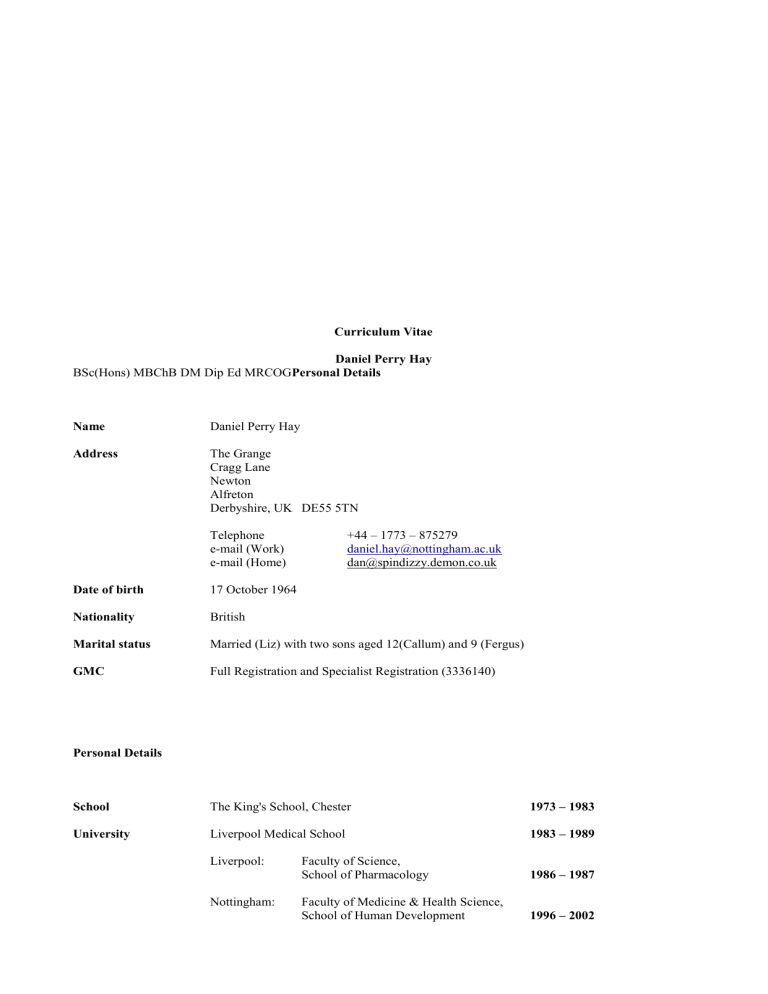
Marital status
GMC
Personal Details
School
University
Curriculum Vitae
Daniel Perry Hay
BSc(Hons) MBChB DM Dip Ed MRCOG Personal Details
Name
Address
Date of birth
Nationality
Daniel Perry Hay
The Grange
Cragg Lane
Newton
Alfreton
Derbyshire, UK DE55 5TN
Telephone e-mail (Work) e-mail (Home)
17 October 1964
British
+44 – 1773 – 875279 daniel.hay@nottingham.ac.uk
dan@spindizzy.demon.co.uk
Married (Liz) with two sons aged 12(Callum) and 9 (Fergus)
Full Registration and Specialist Registration (3336140)
The King's School, Chester
Liverpool Medical School
Liverpool:
Nottingham:
Faculty of Science,
School of Pharmacology
Faculty of Medicine & Health Science,
School of Human Development
1973 – 1983
1983 – 1989
1986 – 1987
1996 – 2002
BSc(Hons):
MBChB
DM
MRCOG
Faculty of Medicine & Health Science,
Centre for Postgraduate & Continuing
Medical Education
Class two, division one; Pharmacology
'Trophoblastic Embolisation to the Maternal
Peripheral Circulation in and prior to the onset of
Pregnancy Induced Hypertension/Pre-Eclampsia.'
2000 - 2005Qualifications
1987
' The transdermal absorption and metabolism of
Norethisterone acetate.'
1989
1997
2002
Dip Ed
CCST holder since May 2001.
Entered on the Specialist Register of the GMC August 2001.
First 5 year cycle of Continuing Medical Education (RCOG) completed August 2006.
BSCCP (colposcopy qualification) expired in September 2006 as
I no longer perform colposcopy; this can be reinstated with ease if required.
Awards
King's School Mothers' Guild University Leavers' Award
(for books and equipment pertinent to the study of medicine)
Faculty of Medicine Undergraduate Scholarship
(for tuition fees whilst reading pharmacology)
1983
1986
2006
Ciba – Geigy 1986
(for materials for the study of the transdermal pharmacokinetics of Norethisterone acetate)
Benjamin Hall Trust
(for subsistence and for materials for the study of trophoblastic embolisation)
1994
SMART award from the Department of Trade and Industry (UK Gov't)
(to develop the filtration enrichment technique to isolate trophoblast from blood)
1996
Best Teaching Firm (jointly with Mr Srini Vindla) 2004
(a much appreciated accolade for our firm from the Sheffield medical students) Appointments (All UK)
Current
19 Dec 2005 to date
Previous Appointments
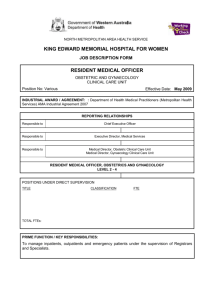
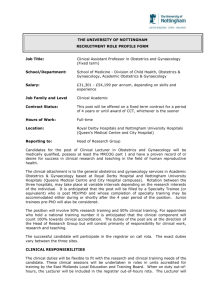
Associate Professor in Medical Education
School of Human Development
University of Nottingham
Consultant in Obstetrics & Gynaecology
Derby City General Hospital NHS Trust
2
1 Sept 2004 to 19 Dec 2005
10 Dec 2001 to 19 Dec 2005
1 Oct 1996 to 30 Nov 2001
1 Feb 1994 to 30 Sept 1996
1994
1 Feb 1994 to 31 July 1994
Senior House Officer posts
1 Feb 1990 to 31 Jan 1991
Associate Director of Teaching
Sheffield Medical School
Consultant in Obstetrics & Gynaecology
Chesterfield Royal Hospital NHS Foundation Trust
Specialist Registrar in Obstetrics & Gynaecology
Mid Trent Rotation
Training Programme Director: Miss MBA MacPherson
SpR 5/CCST holder:
SpR 4:
SpR 3:
Queen's Medical Centre
Nottingham
Miss MBA MacPherson
City Hospital, Nottingham
Messrs CN Bain & JEF Bruce
King's Mill Hospital, Mansfield
Mr CJ Pickles &
Miss PA Makepeace
SpR 2:
SpR 1:
Derby City General Hospital
Messrs FJ Darné & MP Cust
Chesterfield Royal Hospital
Messrs JM McDonnell,
Mr S Krishnamurthy &
Miss JL Cresswell
Research Fellow University Hospital Nottingham
Mr GM Filshie
Part time Resident Medical Officer
BMI Park Hospital, Nottingham
Mrs S Quickmire 1 Feb 1991 to 31 Jan
Obstetrics & Gynaecology (12m)
Queen's Medical Centre
Messrs GM Filshie & MC
Powell
Oncology (6m)
General Hospital, Nottingham
Drs EM Bessell & SY Chan
Genito-Urinary Medicine (6m)
City Hospital, Nottingham
Drs CJ Bignell, IH Ahmed &
CA Bowman
Obstetrics & Gynaecology (12m)
City Hospital, Nottingham
Prof IR Johnson & Mr AJ Tyack
Pre Registration House Officer posts
Surgery (6m)
Warrington District General
Messrs Croton, Johnson, Seddon
& Wake
Medicine (6m)
3
Warrington District General
Drs JM Jefferson & BD Linaker
Clinical Experience
I have been a generalist consultant in Obstetrics & Gynaecology sub-specialising in medical education for five years. I moved into my current post less than a year ago replacing Prof Ian Symonds who took a chair in Australia. My recent clinical experience therefore spans two sites; Derby and Chesterfield. For clarity I will delineate them separately.
Derby City General Hospital
A large tertiary centre, teaching hospital which is due to become twice its current size as it will join with Derby Royal
Infirmary (also a tertiary centre) on the City site next year. A graduate entry medical school is attached and we also accept Nottingham students (school-leaver entry) for clinical attachments.
There are 4,700 deliveries per annum. It has CNST 2 status.
My weekly clinical commitment breaks down as follows:
One session (or PA):
One session:
One session:
One session:
Three-quarter session:
Quarter session:
Quarter session:
Administration
Gynaecology Out-Patients
Ante-Natal Clinic incorporating the service for pregnant drug-dependant women
Gynaecology theatre
On-call for both Obstetrics & Gynaecology
Ward rounds
Gynaecology Audit Lead
(Six sessions University)
I perform and teach all the routine minor and major gynaecological procedures and accept vaginal hysterectomies and pelvic floor work from Prof RW Shaw who reciprocates by taking laparoscopic laser surgery cases from me. I offer
Tensionless Vaginal Tape procedures (obturator approach) to the urogynaecology unit. I am competent at managing ectopic pregnancy both medically and laparoscopically.
My intra-partum care and gynaecological emergency activity is restricted to when I am on-call. The on-call runs in two parallel systems. A week of day time on-call rotates round all the consultants; weekend and overnight on-call rotates on a one in 23 basis (for academics).
During on-call I provide support, supervision and training to the on-call team which consists of two tiers of SpRs and two SHOs. The unit is often busy and when on-call I expect resident for much of the time. We are a tertiary centre that accepts high risk pregnancies and consequently I am needed to be on site to lead the management of these cases on the labour suite. I perform and teach all the usual instrumental and operative delivery techniques including Kjelland's rotation forceps.
I am experienced in dealing with obstetric emergencies (including post-partum hysterectomy) and provide training in them..
Chesterfield Royal Hospital
I was a generalist consultant with special interests in medical education, urogynaecology and colposcopy for four years there. My weekly activities were as follows:
Two sessions:
One session:
One session:
One session:
One session:
Half session:
Quarter session:
Quarter session:
Quarter session:
Labour Suite
Gynaecology Out-Patients
Ante-Natal Clinic
Gynaecology/Urogynaecology theatre
Administration
Colposcopy (BSCCP certification expired September 2006)
Caesarean Section list
Urodynamics
Ward rounds
4
(Two sessions: Associate Director of Teaching/Education provision)
(Quarter session: In house teaching for the SHOs)
The on-call rotated on a 1 in 6 basis covering both Obstetrics & Gynaecology. Chesterfield is a CNST 3 unit with 2,700 deliveries per annum.
I was the obstetric lead for the introduction of multidisciplinary training in obstetric emergencies. I designed the curriculum for a rolling programme and introduced it at neutral cost/cost-improvement (funding came indirectly through the consequent upgrading of CNST 3 status and a reduction in the trust's premium). This training was a main plank for our success at gaining CNST 3 status.
Education
This is my principal area of interest. I have devoted much of the last five years to obtaining the relevant qualifications in medical education but I have a longstanding interest.
1. Personal Development in Education
Diploma in (Clinical) Education
There were four modules on this course:
1.
Teaching: Effective teaching, lecturing, small group work, one-to-one teaching and problem based learning were covered.
2.
Assessment: Both formative and summative: curriculum design and curriculum quality assurance were also covered. Distinction awarded
3.
IT:
4.
PDA
(Information technology) This developed our skills to a level where we were creating interactive web pages complete with hyperlinks and roll-overs (using
Dream-weaver). For my assignment I designed a CAL-package for teaching undergraduates about menstrual disorders.
(Personal Development & Appraisal) This included training in reflective practice (Schönian model) and counselling skills. Also covered were revalidation and appraisal.
2. Associate Professor in Medical Education
In my current role my main remit is to provide education in Obstetrics & Gynaecology to a combination of school entry and graduate entry medical students. I work in a team of committed educationalists comprising myself, an NHS consultant in Obstetrics & Gynaecology with a teaching remit, two acute service midwives, one community midwife and my teaching fellow. Other consultants and academics contribute. We have dedicated clerical and administrative support.
We have two dedicated buildings for education provision with near full specification for multi-format teaching.
We use a number of techniques covering nearly all the teaching methods. We still do a few lectures which are good at covering broad based topics in an efficient manner. We try to incorporate break-out groups or an exercise within those lectures to keep the students stimulated. Most of our teaching is delivered in interactive small-group tutorials. These have a varied format and include traditional bedside teaching. Other formats include SHARP (scenario, history and role play) sessions, obstetric emergency moulages (including the midwifery students), brainstorming and pyramid sessions.
I run a second gynaecology clinic in the week as a teaching clinic with five new patients who have agreed to have their histories taken by students and allow, within reason, the students to help with the pelvic examination i.e. pass the speculum. My NHS counterpart has a similar arrangement for antenatal clinic.
Students also experience GU medicine, community midwifery and provision of antenatal and post-natal care at GP surgeries whilst on attachment to us. They undertake one week of labour suite attachment and perform normal deliveries under the supervision of senior midwives.
We run a formative exam and OSCE towards the end of their attachment.
Students keep a log of their activities and this incorporates provision for them to reflect on their experience. The logbook becomes part of their summative assessment for MBBS finals.
In the larger university I assist in the design of their summative assessment which is by VRQs (varied response questionnaire) and an OSCE. I sit on the undergraduate education committee which is largely to do with curriculum design, quality assurance and examination setting as well as the usual mundane matters of finding examiners and locations to hold examinations in.
I sit on FAGILE (Faculty Advisory Group on Interprofessional Learning and Education) which advises the schools of medicine, nursing, midwifery and the peripatetic disciplines on multidisciplinary training. We have held two multidisciplinary conferences this year in which we discussed a wide range of issues that impact on several professions
5
e.g. the Victoria Climbie case. The format was lectures and break-out sessions.
I sit on the IPE (Interprofessional Education) committee which has a similar role to FAGILE but is concentrated on the
Obstetrics & Gynaecology/Midwifery interface. This committee has been very successful in introducing highly rated interprofessional training in intrapartum care.
Nationally I contributed to the RCOG/RCM joint working party on the clinical learning environment and recruitment.
This party's report was published in January 2008. It is concerned with the quality of education and support for students and trainees.
3. Associated Director Teaching (ADT), Sheffield Medical School
I held this post whilst I was a consultant at Chesterfield which had become an associate teaching hospital at that time.
Sheffield was rolling out its new teaching programme (a Maastricht hybrid) and simultaneously expanding its intake.
Their lead-in time was short. They were facing significant problems with curriculum design because of this.
Departments were being asked to produce PBL (problem based learning) curricula and were failing to do so.
Many were struggling with the concept of PBL. I remain ambivalent. Whilst I recognise the theoretical benefits, I perceive a philosophical dichotomy. PBL is by definition student-centred but we must teach medical students to be patient-centred, There is a potential for students to indulge in navel-gazing when they should be engaged with the patient. This has been borne-out in some instances.
Nevertheless I enjoyed the challenge.
The majority of my time in this role was spent in explaining PBL and assisting in curriculum design, negotiating with clinical directors to take on more students and negotiating more SIFT (Service Increment For Training) money from the university. Ultimately, we achieved all our targets and the new curriculum is widely regarded as a success.
4. Multidisciplinary Training and Acquisition of CNST 3 status (Chesterfield)
I designed the training package that was crucial to our gaining CNST 3 status and, as was my remit, achieved it at a cost-neutral basis.
The training was for all personnel on labour suite (including health care assistants) and had behavioural objectives. The format varied between small group tutorials and mock scenarios using props (moulage). I had help from my colleagues in Obstetrics, Midwifery, Anaesthetics and Paediatrics.
Nationally we were one of the first three units to gain CNST 3 status.
5. Postgraduate Training
In house I deliver practical tutorials to SHOs and SpRs on areas of clinical concern and other issues of import e.g. critical appraisal.
I sit on the Sub-Deanery Education Committee which concerns itself with the delivery of education to SpRs in the Mid-
Trent area. I am currently responsible for their training programme.
I am the University of Nottingham course academic lead for our successful part I and part II MRCOG courses and deliver lectures for both (q.v. section 9). I also lecture to DRCOG and DFFP candidates. At time of writing 60% of our part II course candidates have passed their written examination and have moved to the OSCE stage (3/40 did not sit this time).
I have been an RCOG tutor (at Chesterfield).
I provide mentorship and support to my teaching fellow who is taking her Cert.Ed and wants to move on to a diploma in time.
I am co-supervisor of two MD students registered at St. George's, London.
I provide clinical training, mentorship and support to my lecturer and SHO.
6. Doctors in Difficulty Programme
I set up this programme with a colleague at Chesterfield. It was need that drove us to develop this programme rather than foresight, nevertheless it was based on principals that I had been taught during my PDA training. A timely RCOG document (April 2002) discussing this issue was most helpful. So far we have put three doctors through this programme, all the while maintaining communications with the office of the Postgraduate Dean who has been most supportive.
6
7. General Practitioners
I am involved in the continuing education of General Practitioners, usually at evening gatherings. I plan these sessions to be interactive and fun as well as having a serious message. These have been well received (q.v. invited lectures heading).
8. Nurses
I have been a guest speaker at the University of Nottingham’s School of Nursing's biannual course 'Management of
Care in a Gynaecological Setting' since 1997. I lecture to a group of about twelve nurses on menstrual disorders and premenstrual syndrome.
9. Current Course Involvement
DFFP course, Nottingham (from 2001) sterilisation
DFFP course, Chesterfield (from 2002) medico-legal
MRCOG part I course, Nottingham (from 2001)
Academic Lead (from 2006) introduction structure of exam pharmacology
MCQ review structure of exam pharmacology
MCQ review
MRCOG part I course, Manchester (from 2005)
MRCOG part I course, RCOG, London (from 2006)
MRCOG part II course, Nottingham (from 1998)
Academic Lead (from 2006) introduction pharmacology introduction obstetric emergencies critical appraisal endometriosis premenstrual syndrome
MCQ review essay contributor
VRQ contributor
OSCE examiner
Basic Surgical Skills, Nottingham (from 2005) facilitator
10. Consultant Appraisal
I am a trained appraiser and have undertaken this role for three years.
Administration
I currently run four MRCOG courses a year as academic lead, q.v.under sections 5 & 9 in Education. I organise the speakers, the timetable, the OSCE stations and the feedback. On the last course I did I also had to organise an alternative venue for the OSCEs and get the examiners and candidates there. Examiners and actress patients are apt to cancel at the last minute. I organise back-up.
I am the Gynaecological audit lead for my unit. I organise the subject material, provide statistical support and chivvy completion of audits.
In my role as ADT (q.v. section 3 under Education) I had to draw on man-management skills and a level of diplomacy that I did not believe I could achieve. The role whilst I was there was administratively unsupported and in a short space of time I had to become au-fait with the workings of a medical school and the structure of my own hospital from practically every angle. Problems came down to three main issues:
1.
Student placement
2.
Curriculum change
3.
Money
I dealt with some pretty forceful characters and by diplomacy and compromise achieved my objectives.
7
Audit
I am the Gynaecological Audit Lead at Derby (q.v. under Administration), the same unit where I was a member of the
Maternity & Gynaecology Audit Committee as an SpR in 1997-8. Audit proposals are screened and allocated to SHOs and SpRs. Their progress is checked upon. Conclusions of audits are seen to be put into practice and re-audit dates set.
I am fully conversant with the audit process and concept of the audit spiral.
These are the titles of the audits I have undertaken personally:
Ovarian Diathermy Chesterfield, 1997
Out of hours paging
Induction
Mirena in menorrhagia
U/S in Obstetric Pain
Protocol Adherence
Day Case Usage
Trans-Obturator Tape
Gynae Ultrasound
Postgraduate Courses Attended
Part 1 MRCOG course, Nottingham
GU Medicine Study Weekend, Leeds
Family Planning Course, Nottingham
Part II MRCOG course, Nottingham
Colposcopy Course, Whittington Hospital
ALSO provider Course, Eastbourne
Health Service Management Programme, Sheffield
Appraiser Training, Chesterfield
Racial Awareness, Chesterfield
Dip Ed Course
Invited Lectures
HRT – Risks and Benefits.
A seminar aimed at health visitors and practice nurses
Derby, 1998
Derby, 1998
Mansfield, 1999
Chesterfield, 2004
Chesterfield, 2005
Chesterfield, 2005
Chesterfield, 2005
Chesterfield, 2005
July 1991
April 1992
September 1993
July 1997
June 1999
April 2000
April 2000
April 2002
May 2002
(See section 1 under Education)
Chesterfield 1997
PMS – Help for your heartsink patients
Northern Interbranch Doctors' Group (GPs)
PMS
Northern Menopause Society
Therapeutics of PMS and the Menopause
(Practice nurses)
PMS
(GPs)
Practical Prescribing of HRT
(Multidisciplinary audience)
Practical Prescribing of HRT
(Multidisciplinary audience)
Stérilisation Tubaire dans le Royaume-Unis
XVIème Journée Pyrenees de Gynecologie
Given in French to an audience of French Gynaecologists.
Leeds 1998
Doncaster 1998
Pontefract 1998
Nottingham 1998 & 1999
Nottingham 2000
Chesterfield 2000
Pau, France 2002
8
Appraising WHI
Specialist trainees programme
PMS treatment options
(Multidisciplinary audience)
HRT post WHI
(GPs)
Trophoblast in Health and Disease
(Audience of Obstetricians and Scientists)
Signs and Symptoms of Prolapse
(Practice Nurses on a ring pessary training day)
Menstrual Disorders and PMS
(Study day for Practice Nurses)
Modernising Medical Careers
Audience of Consultants and Adminstrators
Update on Contraception
(GPs)
Menstrual Disorders and PMS
(Study day for Practice Nurses)
PCOS Update
(Multidisciplinary audience)
Chesterfield 2002
Chesterfield 2002
Chesterfield 2002
Trent Region 2002
Wolverhampton 2003
Derby 2003
North Derbyshire 2004
Leicester 2004
Nottingham 2004
Nottingham 2004
Endometriosis
(Multidisciplinary audience)
Teaching in the Twilight
(Audience of Obstetricia & Gynaecologists at St George's)
Sex after the Menopause
(Multidisciplinary audience)
Managing PCOS and Hirsutism
(Multidisciplinary audience)
Multidisciplinary Working
International Uro-Gynaecological Association
Managing PCOS and Hirsutism
(Practice nurses)
Nottingham 2004
London 2005
Chesterfield 2005
Chesterfield 2005
Athens 2006
Derby 2006
Conferences Attended
Fetal cells in the Maternal Circulation: IIIrd workshop
27 th British Congress of Obstetricians & Gynaecologists
Hinckley 2002
Specialist Registrars' Conference
(Poster presentation)
Nottingham 1998
8 th Congress of the European Society of Gynaecological Endoscopy Stockholm 1999
Pathophysiology of Perinatal Asphyxia and its prevention
(Prize winner:
Best Presentation)
London 2002
31 st Nuffield Obstetrics & Gynaecology Society
Leeds 1995
Dublin 1995
9
XVIème Journée Pyrenees de Gynecologie
32 nd Nuffield Obstetrics & Gynaecology Society
International Continence Society
11 th World Congress of Gynecological Endocrinology
33 rd Nuffield Obstetrics & Gynaecology Society
International Uro-Gynaecological Association
(Elected Treasurer)
Pau, France 2002
(Speaker)
Hinckley 2003
(Treasurer)
Florence 2003
Florence 2004
Alton Towers 2004
Athens 2006
(Speaker & Chair)
Research
I have recently returned to academia and have commenced supervision of a clinical fellow at the end of August 2006.
We are currently working together to devise a suitable research project and one potential study is exploring medical students' attitudes to training broken down into comparison groups (GEM students and traditional entry students). We are involving one of the students as part of the study group. He is eager to pursue a career in Obstetrics & Gynaecology and I am encouraging him and helping as best as I can.
I have been providing statistical support to groups who have data they wish to analyse and/or present and are either uncertain how to go about it or their statistical methodology is flawed. I have provided this support to St. George's
Urogynaecology unit in the past and they are kindly involving me in the analysis of some of their data relating to QOL scoring.
DM
My principal research was in the pathogenesis of pre-eclampsia. I tested the hypothesis that trophoblast deported into the maternal circulation is fundamental to the pathogenesis and should therefore be present in higher quantities in women who have pre-eclampsia and who go on to develop pre-eclampsia.
During my two year research programme I acquired antibodies to demonstrate trophoblast from Flinder's University in
South Australia; developed a filtration enrichment technique to capture trophoblasts from blood samples; developed a radio-immunoassay to quantify them; and performed a cross sectional study (pre-eclamptic patients versus matched controls) and a longitudinal study.
BSc(Hons)
I was introduced to laboratory based research at Liverpool University in the Honours School of Pharmacology. My research was into the transdermal pharmacokinetics of Norethisterone acetate.
Free Communications
Laparoscopic oophorectomy for trapped ovarian syndrome with occlusion of the infundibulopelvic ligament prior to division by the use of the Filshie clip. Filshie GM, Powell MC, Xenophou X, Hay DP. 2 nd European Congress in
Gynaecological Endoscopy and New Surgical Techniques. Heidelberg 1993.
Laparoscopic oophorectomy for trapped ovarian syndrome with occlusion of the infundibulopelvic ligament prior to division by the use of the Filshie clip. Filshie GM, Powell MC, van Wijngaarden WJ, Hay DP. 2 nd European Congress
in Gynaecological Endoscopy and New Surgical Techniques. Davos 1995.
Hygroscopic cervical dilators v. prostaglandin for cervical ripening prior to induction of labour. Hay DP, Robinson G,
Filshie GM, James DK. British Congress of Obstetricians & Gynaecologists. Dublin 1995.
Changes in cervical compliance and structure subsequent to treatment with Dilapan-S and gemeprost. J Owen, A
Rostocil, D Hay, J Jelinek, W van Wijngaarden, L Pilka, G Robinson, L Slavik, M Filshie. XVth European Congress of
Perinatal Medicine. Glasgow 1996.
Laparoscopic Ovarian Diathermy for PCOS. D Hay. Birmingham & Midland Obstetrical & Gynaecological Society.
10
Wolverhampton 1998.
Kallman's Syndrome. D Hay. Derby Medical Society 1998.
Laparoscopic Assisted Vaginal Hysterectomy and Bilateral Salpingo-Oophorectomy. What a waste of time! Results of
64 cases. Krishnamurthy S, Ravi A, Hay D. 8 th Congress of the European Society of Gynaecological Endoscopy.
Stockholm 1999.
Predicting whom benefits from ovarian diathermy for non-clomiphene responding anovulatory subfertility associated with the polycystic ovarian syndrome: a study of 47 consecutive patients using take home baby as the outcome measure.
Hay D, Krishnamurthy S. 8 th Congress of the European Society of Gynaecological Endoscopy. Stockholm 1999. First
Prize Winner.
Publications
Changes in cervical compliance and structure subsequent to treatment with Dilapan-S and gemeprost. J Owen, A
Rostocil, D Hay, J Jelinek, W van Wijngaarden, L Pilka, G Robinson, L Slavik, M Filshie. Prenatal and Neonatal
Medicine . 1: suppl 1; 257. 1996 .
Laparoscopic oophorectomy for trapped ovarian syndrome with occlusion of the infundibulopelvic ligament prior to division by the use of the Filshie clip. Daniel Hay, Xenakis Xenophou, Martin Powell, Marcus Filshie. Gynaecological
Endoscopy. 4: 241-243. 1996.
Removal of a stuck IUCD in a needle phobic patient by use of a hygroscopic cervical dilator in preference to conventional dilatation under general anaesthesia. Hay DP, van Wijngaarden WJ, Filshie GM. Br J Fam Planning. 22:
154-155. 1996.
Subcutaneous Hormone Implantation. Filshie GM & Hay DP. In Essential Medical Procedures. Ed Toghill PJ: 41-43.
Arnold, London 1997.
Taking a Cervical Smear. Hay DP & Filshie GM. In Essential Medical Procedures. Ed Toghill PJ: 123-128. Arnold,
London 1997.
Potentially Dangerous Complication of an ineffective Shelf Pessary. DP Hay, WL Martin, FJ Darné. Journal of
Obstetrics & Gynaecology. 19(6):669. 1999
Continuous Combined HRT: Can it improve compliance? Daniel Hay and Marcus Filshie. Trends in Urology,
Gynaecology and Sexual Health. Current thinking suppl: 6-11. 2000
Sexually Transmitted Infections. Jennifer Parratt and Daniel Hay. Current Opinion in Obstetrics & Gynaecology. 13(4):
224-232. 2003
Medical Literature Appraisal. DP Hay. Current Opinion in Obstetrics & Gynaecology. 14(6): 434-438. 2004
Sexually Transmitted Infections. Eimear Kieran and Daniel Hay. Current Opinion in Obstetrics & Gynaecology. 16:
218-225. 2006
Timing of Induction of labour for post maturity and caesarean section patterns. F Bano, H Hamoud, D Hay, C Pickles
Current Women's Health Reviews.
2(3): 193-195. 2006
The Clinical Learning Environment and Recruitment. Joint RCOG/RCM Working Party (Contributor). RCOG Press,
London. 2008
Outside Activities
I spend as much time as I can with my family. We spend the majority of our time together walking in the Peak District with our our Labrador, Louie. We are members of the National Trust and English Heritage. We also enjoy swimming, ten-pin bowling and trips to the seaside.
11
My older son (Callum) enjoys a game of chess and is starting to beat me! Callum and I both enjoy skiing and go once a year to the Aosta Valley.
Fergus, our younger son, is on the autism spectrum presenting predominantly with speech delay. Liz and I spend much of our free time working with him to develop strategies to encourage him to use language more.
I enjoy cookery, a hobby of mine since medical school, and entertain family and friends with ever more lavish and intricate dinner parties. On a more atavistic level I love to barbecue. A love of food has led to my taking up vegetable gardening as the flavour of home-grown is hard to beat. I have four beds on a crop rotation, a greenhouse (tomatoes), a strawberry patch, two apple trees and a pear tree.
Referees
Miss Janet L Cresswell
Clinical Director and Consultant Obstetrician & Gynaecologist
Women & Children's Directorate
Chesterfield Royal Hospital
Chesterfield S44 5BL
UK
Tel: +44 1246 277271 e-mail: janet.cresswell@chesterfieldroyal.nhs.uk
Mr Mike P Cust
Consultant Obstetrician & Gynaecologist
Derby City General Hospital
Uttoxeter Road
Derby DE22 3NE
UK
Tel: +44 1332 340131 e-mail: michael.cust@derbyhospitals.nhs.uk
Miss Michelle Fynes
Consultant Urogynaecologist
Dept. of Reconstructive Pelvic Surgery & Urogynaecology
Level 4
Lanesborough Wing
St George's Hospital
Tooting
London SW17 0RE
UK
Tel: +44 208 725 1909 e-mail: beatrice.benjamin@stgeorges.nhs.uk
Dr Reg Dennick
Assistant Director of Medical Education
The Medical Education Unit
The Medical School
Queen's Medical Centre
Nottingham NG7 2UH
UK
Tel: +44 115 8230028 e-mail: reg.dennick@nottingham.ac.uk
Dr Louise Kenny
Senior Lecturer in Obstetrics
Centre for Human Molecular Reproduction
Anu Research Centre
12
5th Floor
Cork University Maternity Hospital
Wilton, Cork
University College Cork
Tel: 00353866033272 e-mail: l.kenny@ucc.ie
Miss Susan Ward
Associate Postgraduate Dean, Trent Multi-Professional Deanery
Consultant Obstetrician & Gynaecologist
Sherwood Forest Hospital's Trust
Mansfield Road
Sutton in Ashfield NG17 4JL
Tel: +44 1623-622515
E-mail: Susan.ward@sfh-tr.nhs.uk
13