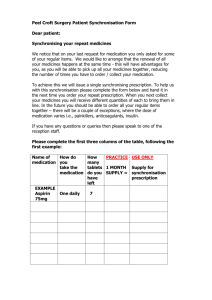
Repeat Prescribing Protocol
advertisement

Example of a Repeat Prescribing Protocol Nov 2007, Updated Jan 2009 & Feb 2011 Authors: Suzanne Quinlan and Dr Diarmuid Quinlan 1. HIGH RISK GROUPS: I. Patients aged 65 years or over. II. Patients on four or more medicines. III. High risk medicines: − Frequent claims for Antibiotics or Steroids by any route. − Toxic medicines. − Frequent injuries: NSAIDS, Anticoagulants. IV. Primary/Secondary care interface: − Recent hospital discharges. − Hospital OPD. − Specialist Referrals. 2. REQUESTING REPEAT PRESCRIPTION: − Repeat prescriptions may be requested in writing (post/delivery by hand/pharmacist). − Phone requests are not routinely accepted due to risk of error, except in special circumstances (ie, housebound patients). − Patients are to be supplied with “blue list” of repeat medicines and encouraged to use same. − Emergency verbal requests may be accepted but please inform the doctor. − Patients should be educated about the process and objectives of repeat prescribing. − Doctors should actively strive to reduce the number of requests for repeat prescriptions: where possible prescribe sufficient medication to last until the next review – give 3 or 6 months supply where appropriate. 3. PROCESSING & JOURNEY OF REPEAT PRESCRIPTIONS: On receipt of the request, date and time to be marked. The prescription should be carefully prepared by a secretary in a quiet area, free of distraction and interruptions. The completed prescription and the patient’s request are left for the doctor to carefully check and then sign. Ireland 2012 1 Target: Ideally prescription completed, checked and signed in less than 24 hours, and always in less than 48 hours. Patients requesting emergency medication are to be facilitated. However, please attach a note with the prescription asking for five days notice in future. Patients can request items not on their repeat list by writing the request on the blue form. However, only the doctor can add such items to the prescription. Secretaries must never add new medication to a prescription. To do so is a serious error. Doctors should support the secretaries in this matter. 4. UPDATING PRESCRIPTIONS FROM HOSPITAL LETTERS AND DISCHARGE SUMMARIES: Errors arise here very easily so exercise great caution. Updating prescriptions should be routinely done by the patient’s doctor, on receipt of hospital letters. Only the doctor can add a new medicine to a prescription. The doctor must ensure the clinical record and the medicine record are both updated and retained appropriately. In the event of medicines being discontinued, this should be recorded and “unretained”. Prescribing requested by specialist: Medico-legal responsibility lies with the doctor signing the prescription. GPs should not write a prescription at the request of secondary care colleagues until they are satisfied that the patient has been appropriately counselled re the medication, dangers and side effects. The doctor must have a robust system to ensure appropriate monitoring occurs. 5. REQUESTS TO COPY A HOSPITAL PRESCRIPTION TO G.M.S. PRESCRIPTION: Photocopy hospital prescription. Return original to patient and ask them to get a 7-day supply in their pharmacy. The doctor amends the clinical record and drug database, adds the new medicine and generates script. The photocopied hospital script is scanned into patient’s file. Admin staff must never initiate new medications. To do so is a serious error. It is legally indefensible for a secretary to add medicines to a prescription. Doctors should never ask, expect or allow the secretaries to do this. Ireland 2012 2 6. QUANTITY OF MEDICINES SUPPLIED: Currently in multiples of 30. Scripts should be synchronised where possible to make re-ordering easier for patients/staff. Single items should state “No Repeat”. Otherwise a pharmacist is entitled to repeat dispense. 7. ADDING ADDITIONAL/NEW REPEAT MEDICATION(S): Only doctors can add new medication(s). Admin staff must never add medication. To do so is a serious error. The doctor should update the repeat medication list when additional items are added or terminated. The clinical record should be amended to explain the changes. Ideally the new amended script should carry an explanation note for the pharmacist, ie, “Diovan discontinued; Co-Diovan started”/“Thyroxine dose changed”. 8. REVIEW DATES: New patients must see a doctor before any prescription is issued. All patients getting repeat prescriptions should be seen by their doctor at least once a year. This is to review the medical diagnosis, medication, compliance, monitoring etc. Certain groups need more frequent review: − Patients over 65 years of age. − Patients on four or more medicines. − Recent hospital and OPD discharges. − Those on high-risk medicines. This review should assess: − Patients understanding of medication, illness etc. − Update clinical summary and repeat medications. − Assess relevant monitoring tests. − Medication not currently used should be removed from the drug database. − The condition for which the patient is taking the repeat medication should be clear from the medical record, ie, “Gastritis” in the summary of a patient taking a P.P.I. Ireland 2012 3 9. INAPPROPRIATE MEDICATION AS A REPEAT: The following are considered inappropriate to be given as REPEAT medication. The doctor should see the patient and only then issue a prescription. − Very potent topical steroids: Betnovate, Dermovate etc. − Oral steroids. − Benzodiazepines (other than long-term existing patients, who have been appropriately counselled and this clearly recorded). − Antidepressants. − A.D.H.D. medicines (Ritalin etc). − Thyroxine. − Controlled drugs. − NSAID’s. − Oral contraceptive medication. − Hormone replacement therapy. 10. CONTROLLED DRUGS: Please generate a script on the computer. This leaves a “footprint” in the patient record. Controlled drug scripts must then be handwritten by the doctor on the printed copy. Record in the patient file who collected the script. Ideally such scripts should ONLY be given to the patient or an agreed relative. This helps stop misuse of controlled drugs. 11. POTENTIALLY TOXIC DRUGS: HAVE A ROBUST SYSTEM IN PLACE TO MONITOR PATIENTS TAKING TOXIC MEDICATION. The doctor should provide information to the patient about the risks/side effects of the toxic medication and the importance of blood monitoring and clearly document this. Prior to issuing a new prescription for a toxic medication, the doctor must ensure appropriate recent blood tests/investigations have been completed. If a blood test is due, supply a very limited quantity (1-2 weeks) of toxic medication. Write a note to the patient requesting attendance for a blood test and document this. The patient should ideally see the doctor to get a prescription and these scripts should be generic where possible. Ireland 2012 4 The following drugs should NEVER be given as a repeat medication: − Warfarin. − Lithium. − Methotrexate. − Azathoprine. − Amiodarone. − DMARDS. Great care is needed with potentially toxic drugs. Some consultants write private scripts for these medicines. We may be casually requested to monitor blood tests. I suggest: a. We notify the patient in writing of the need for blood tests at appropriate intervals AND stress the importance of the patient contacting the surgery to arrange same. b. We notify the consultant in writing of our concerns. The consultant has prescribed toxic medications in the belief that the GP will arrange and monitor blood tests. The patient may never attend the surgery for same. This is clearly a very unsafe practice. 12. OVERUSE AND UNDERUSE OF MEDICATION: Prescriptions that are not collected from the practice/pharmacy should be returned monthly to the prescribing GP. The doctor should enter a note in the patient file and the script is then shredded. This system will allow review of uncollected prescriptions, which may reflect poor compliance with potentially serious consequences for the patient. If the patient is due a review (medical, medication, blood tests) add a note to the repeat prescription asking the patient to make an appointment. Document this in the patient file. 13. Anti Coagulant Monitoring: “Errors of warfarin control are among the most frequent causes of GP litigation”. The start date, indication, duration of therapy and target INR should be prominently recorded, ideally in the patient summary. All patients should be counselled about the use and hazards of warfarin and the importance of regular monitoring. The doctor should inform the patient of the INR result, the warfarin dosage and follow-up appointment date. A simultaneous letter generates a permanent record, but this is at the doctor’s discretion. Ireland 2012 5 14. PHARMACY PROCEDURE: We greatly value the support and vigilance of our pharmacy colleagues. A pharmacist phoning with a medicine query should be put through to the appropriate doctor. As stated previously, a brief handwritten note on the script helps prevent confusion when a medicine is commenced, discontinued or dose changed. This enhances patient safety. Ireland 2012 6 “REQUESTING A REPEAT PRESCRIPTION” For reasons of safety when requesting a repeat prescription please note: 1. Verbal requests/phone requests will no longer be routinely accepted for safety reasons. In exceptional circumstances your doctor will accept such requests, eg, (housebound patients). 2. This list of your current medication is very helpful in an emergency. Please keep it safely on your person (purse/wallet/driving licence). 3. Your doctor will give you a list of current medication, please mark clearly on this list which medicines you require. 4. We aim to complete your request within 48 hours, but would appreciate 5 working days notice. 5. Please direct any queries or comments to your own doctor. THANK YOU FOR YOUR CO-OPERATION WITH THIS SAFETY INITIATIVE. Ireland 2012 7