How is acute hypermagnesaemia treated in
Medicines Q&As
Q&A 370.1
How is acute hypermagnesaemia treated in adults?
Prepared by UK Medicines Information ( UKMi ) pharmacists for NHS healthcare professionals
Date prepared: 11th March 2011
Background
There are no national guidelines for the treatment of acute hypermagnesaemia, and practice varies widely across hospital Trusts. Following a thorough search of the literature, this guidance has been prepared and adopted in Leeds Teaching Hospitals NHS Trust.
Reference ranges for serum magnesium vary between laboratories. For the purpose of this document, the reference range used for magnesium is 0.7-1.0 mmol/L, although treatment of hypermagnesaemia is unlikely to be required unless the serum magnesium concentration exceeds
2.0 mmol/L (1).
Serum magnesium concentrations are a poor indicator of total active ionised magnesium levels. The plasma contains only approximately 0.3% of total body magnesium and the relationship between serum magnesium levels and total magnesium stores has not been clearly defined (2).
Many symptoms of hypermagnesaemia at lower levels are non-specific (3). Although the absolute serum magnesium concentration is important, the rate of increase in magnesium concentration may be more significant (3, 4). In patients with normal renal function, clinically significant hypermagnesaemia is rare (5).
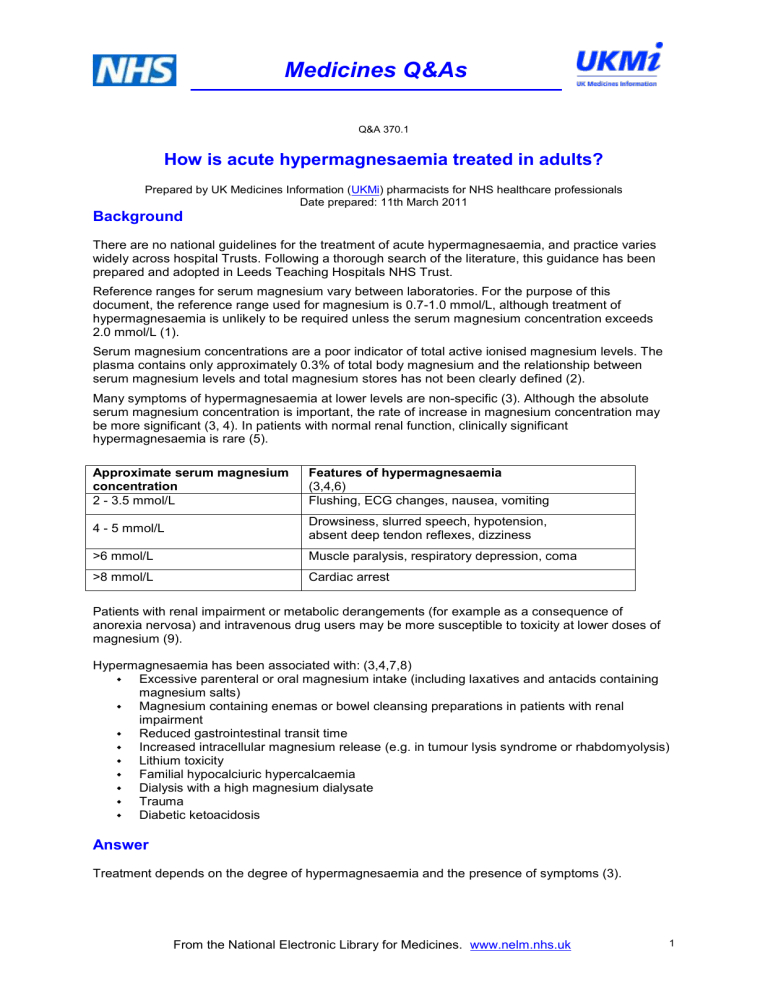
Approximate serum magnesium concentration
2 - 3.5 mmol/L
Features of hypermagnesaemia
(3,4,6)
Flushing, ECG changes, nausea, vomiting
4 - 5 mmol/L
>6 mmol/L
>8 mmol/L
Drowsiness, slurred speech, hypotension, absent deep tendon reflexes, dizziness
Muscle paralysis, respiratory depression, coma
Cardiac arrest
Patients with renal impairment or metabolic derangements (for example as a consequence of anorexia nervosa) and intravenous drug users may be more susceptible to toxicity at lower doses of magnesium (9).
Hypermagnesaemia has been associated with: (3,4,7,8)
Excessive parenteral or oral magnesium intake (including laxatives and antacids containing magnesium salts)
Magnesium containing enemas or bowel cleansing preparations in patients with renal impairment
Reduced gastrointestinal transit time
Increased intracellular magnesium release (e.g. in tumour lysis syndrome or rhabdomyolysis)
Lithium toxicity
Familial hypocalciuric hypercalcaemia
Dialysis with a high magnesium dialysate
Trauma
Diabetic ketoacidosis
Answer
Treatment depends on the degree of hypermagnesaemia and the presence of symptoms (3).
1 From the National Electronic Library for Medicines. www.nelm.nhs.uk
Medicines Q&As
If serum magnesium concentrations are mildly increased (2 - 4 mmol/L) and the patient is asymptomatic:
Remove the source of magnesium (3,4,7,8,10,11). Remember that in addition to magnesium supplements, magnesium may also be found in antacids, laxatives and bowel cleansing preparations. Refer to the BNF for further information.
Maintain good urine output (6).
Measure serum magnesium concentrations after 24 hours and provide further symptomatic and supportive treatment as necessary (1).
In patients with normal renal function, this is likely to be all that is required. In patients with impaired renal function more intensive monitoring may be required (1).
If serum magnesium concentrations are significantly increased (>4 mmol/L), or if the patient is showing significant clinical features of hypermagnesaemia:
Remove the source of magnesium (1).
Calcium salts antagonise the neuromuscular and cardiovascular effects of magnesium.
Consider giving 10mL calcium gluconate 10% by slow intravenous injection (5,7,8,10,12) over at least 5 minutes (13,14). Monitor serum calcium concentration (15). For further information on how to administer IV calcium gluconate, refer to the Medusa Injectable Medicines Guide or local policy.
Calcium salts are irritant and may cause tissue damage if extravasation occurs (6,10,13-
15).
Calcium salts should be given with caution to patients with renal impairment, hypercalcaemia or conditions associated with hypercalcaemia such as sarcoidosis and some malignancies, or in patients with a history of renal calculi (10).
Please note the following interactions with calcium gluconate. This is not an exhaustive
list, see product literature for further information
Digoxin - Calcium salts enhance the cardiac effects of cardiac glycosides (e.g digoxin)
and should be used with great caution in patients taking digoxin (10,15,16,17).
Diuretics - The potential for hypercalcaemia is greater in patients taking thiazide diuretics concurrently with parenteral calcium salts (16,17).
Other calcium salts are available, but are generally considered to be more irritant (10,15).
Intravenous calcium gluconate would be expected to have an immediate effect on ECG changes and may improve central depression. The effect will be transient unless the serum magnesium concentration falls. Arrhythmias will require continuous ECG monitoring and repeat intravenous calcium gluconate may be required. Recheck serum magnesium concentration after four hours (1).
If the patient is still hypermagnesaemic, discuss with a renal or biochemistry consultant. Dialysis may be needed (3-7,10,12).
Monitoring of plasma magnesium concentrations is essential, especially in patients with reduced urine output (1). In patients at risk of significant symptoms as a result of hypermagnesaemia or in those who have received intravenous calcium gluconate, measure serum magnesium concentrations every four hours (1).
Monitor other electrolytes as disturbances of magnesium rarely occur alone (1,5,18).
Summary
There is no national guidance on the treatment of hypermagnesaemia, and practice varies widely between hospital Trusts. The guidance in this document reflects practice at Leeds
Teaching Hospitals NHS Trust.
In asymptomatic patients with a serum magnesium concentration of 2-4 mmol/L, remove the source of magnesium, maintain good urine output and measure serum magnesium concentrations again after 24 hours.
In symptomatic patients or those with serum magnesium concentration above 4 mmol/L consider a slow intravenous injection of 10mL calcium gluconate 10%. Recheck serum magnesium concentrations after four hours.
If the serum magnesium concentration doesn’t decline sufficiently, dialysis may be required.
2 From the National Electronic Library for Medicines. www.nelm.nhs.uk
Medicines Q&As
Monitor serum magnesium concentrations and other electrolytes as appropriate. Closer monitoring is likely to be required in patients with renal impairment as magnesium is renally cleared.
Limitations
This Q&A is designed for adult patients only. This guidance is not suitable for chronic hypermagnesaemia or for patients with complex medical problems. There are no national guidelines for the treatment of hypermagnesaemia, and practice varies widely across hospital Trusts.
Disclaimer
Medicines Q&As are intended for healthcare professionals and reflect UK practice.
Each Q&A relates only to the clinical scenario described.
Q&As are believed to accurately reflect the medical literature at the time of writing.
The authors of Medicines Q&As are not responsible for the content of external websites and links are made available solely to indicate their potential usefulness to users of NeLM. You must use your judgement to determine the accuracy and relevance of the information they contain.
See NeLM for full disclaimer.
References
1. Leeds Teaching Hospitals NHS Trust. Clinical guideline for the treatment of hypermagnesaemia in adults. In house document. Review date February 2013
2. Noronha, J.L., Matuschak, G.M. Magnesium in critical illness: metabolism, assessment, and treatment. Intensive Care Med (2002) 28:667 –679
3. Ferry, R.J. Hypermagnesemia. Available at http://emedicine.medscape.com/article/921382overview (Accessed 23/02/2011)
4. Novello, N.P., Blumstein, H.A. Hypermagnesemia. Available at http://emedicine.medscape.com/article/766604 (Date accessed 23/02/2011).
5. Ryan, M.F. The role of magnesium in clinical biochemistry: an overview. Annals of Clinical
Biochemistry (1992) 28:19-26
6. National Poisons Information Service and Health Protection Agency. Toxbase. Available online http://www.toxbase.org. (Date accessed 10/01/2011)
7. Kumar, P., Clark, M. (eds) Clinical Medicine. Sixth Edition (2005). Elsevier Saunders.
8. Fulop, T. Hypermagnesemia. Available at http://emedicine.medscape.com/article/246489print (Accessed 23/02/2011)
9. Hutchison TA, Shahan DR & Anderson ML (eds) Drugdex System Internet version
Micromedex Inc. Greenwood Village, Colorado. Date searched 10/01/2011
10. Sweetman S (ed.). Martindale. The Complete Drug Reference, online edition. The
Pharmaceutical Press, London. (Date accessed 10/01/2011)
11. Weisinger, J.R. and Bellorin-Fon, E. Electrolyte quintet: magnesium and phosphorus.
The
Lancet . (1998) 352:391-396
12. Summary of Product Characteristics. UCB Pharma Magnesium Sulphate 50% Injection
®
. http://emc.medicines.org.uk/ (date accessed 23/02/2011; date last updated: 27/09/2010)
13. Medusa Injectable Medicines Guide. Available at http://medusa.wales.nhs.uk (Date accessed
23/02/2011)
14. Trissel LA. Handbook on Injectable Drugs, 14th Edition (2006 online edition). American
Society of Health-System Pharmacists, Bethesda, USA. Date accessed: 23/02/2011.
15. McEvoy GK (ed.). AHFS Drug Information 2009, online edition. American Society of Health-
System Pharmacists, Bethesda, USA. http://medicinescomplete.com. (Date accessed
10/01/2011)
16. Baxter K (ed). Stockley’s Drug Interactions, online edition. The Pharmaceutical Press,
London. (Date accessed 28/02/2011) http://medicinescomplete.com
17. Summary of Product Characteristics. (Hameln Pharmaceuticals Calcium Gluconate Injection
BP
®
). http://emc.medicines.org.uk/ (date accessed 23/02/2011; date last updated:
09/08/2010)
3 From the National Electronic Library for Medicines. www.nelm.nhs.uk
Medicines Q&As
18. Crook, M. A Study of hypermagnesaemia in a hospital population. Clin Chem Lab Med .
(1999) 37(4):449-451
Quality Assurance
Prepared by
Lucy Hennessy, Leeds Medicines Information Centre
Date Prepared
11th March 2011
Checked by
Dave Abbott, Leeds Medicines Information Centre
Date of check
11th March 2011
Search strategy
Embase [terms used: magnesium (exp), hypermagnesemia (exp), limited to English, Human and
Adult.]
Medline [terms used: magnesium (exp), hypermagnesemia (exp), limited to English, Human and
Adult]
In-house Database/resources
eMC
From the National Electronic Library for Medicines. www.nelm.nhs.uk
4