Title: Differential Patterns of Well-Being, Symptoms and
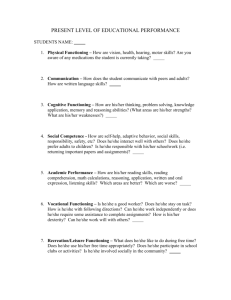
advertisement

COMBINE Manuscript Proposal Form For Administrative Use Only MS # O04 Date Received: 12/3/04 Date Reviewed: Priority Set: Scheduled for Review: Action: Title: Differential Patterns of Well-Being, Symptoms and Functioning Outcomes to Pharmacotherapy and Psychotherapy Interventions. Proposed Writing Group Members: Members of the Functional Outcomes of COMBINE Treatments Ancillary Study Group (Cisler lead then alphabetical order): R. Cisler (Milwaukee), D. Donovan (Washington), D. Gastfriend (MGH/Harvard), J. LoCastro (Boston University), R. Longabaugh and Robert Swift (Brown), M. Mattson (NIAAA) and H. Pettinati (Pennsylvania), A. Zweben (Milwaukee). Rationale: This analysis was proposed and approved as a COMBINE ancillary study entitled, “Functional Outcomes of COMBINE Treatments.” This study and proposed analyses is an extension of work by the primary investigator (Cisler) and colleagues of innovative alcoholism treatment assessment including development of a clinically-interpretable composite outcome index (Cisler & Berger, 2001; Cisler & Zweben, 1999, Zweben & Cisler, 2003), recommendations for innovative assessment approaches in clinical trials (Flannery, Allen, Pettinati, Rohsenow, Cisler, & Litten, 2002), assessing non-drinking outcomes in COMBINE (Cisler, Kivlahan, Donovan & Mattson, In press) and quality of life as an outcome measure (Donovan, Mattson, Cisler, Longabaugh & Zweben, In press). The current analysis is consistent with the dose-response model or phase model of behavioral treatment outcome assessment (Howard et al., 1993; Howard et al., 1996) and will examine the differential effects of pharmacotherapy (two types of medications, naltrexone and acamprosate) and psychotherapy (two forms of counseling: Medication Management (MM) and COMBINE Behavioral Intervention (CBI). As applied to COMBINE, the three phases/goals of treatment and associated outcomes are summarized as follows: (1) Remoralization goals of Medication/MM and motivational aspects of CBI with Subjective Well Being as primary outcome; (2) Remediation goals of Medication/MM and CBI with Alcohol-Related Symptoms as primary outcome; and (3) Rehabilitation goals of CBI with Psychosocial Functioning as primary outcome. Hypotheses: MM/Medication is expected to affect well-being and symptoms during treatment; effects of medication may disappear after treatment is removed. CBI is expected to affect well-being, symptoms and functioning both during and after treatment; CBI should promote functional improvement that sustains after treatment is removed. Finally, MM/Medication plus CBI may have additive effects on well-being, symptoms and sustained functioning. Target dates: Initial analyses to be completed by June, 2005. Final analyses completed by August, 2005. Paper to be written and submitted by October, 2005. Proposed inclusion/exclusion criteria for cases: It is anticipated that 750 participants will be involved in this study (i.e., approximately 125 participants at each of six performance sites). This sample size should be ample to test basic differences between pharmacologic and behavioral interventions. All participants who intended to be treated at six COMBINE sites will be examined with those not providing data being determined as non-responders. Description of data sources (forms) used: Data collection procedures for this study were consistent with established collection of self-report data in COMBINE. Symptom data such as consequences (DrInC; Miller et al., 1995) and craving (OCDS; Anton et al., 199X) were collected at regular intervals during and after treatment as part of the primary assessment battery. The Subjective Well-Being Scale (Howard et al., 1993; Howard et al., 1996; Seligman, 1995) was administered at baseline, during treatment (at weekly visits 0, 1, 2, 4, 6, 8, 10, 12, and 16 weeks) and at follow-up (visits 6, 12, and 16 months). The Psychosocial Functioning Inventory (Feragne, Longabaugh, & Stevenson, 1983) was administered at baseline, during treatment (at weeks 8 and 16) and at follow-up (visits 6, 12, and 16 months). Data analysis: Mean well-being, symptoms (reversed) and functioning will be plotted as a function of number of sessions of treatment using measures collected at baseline, during treatment and at the end of treatment. Cross-classification analyses will examine whether an improvement in subjective well-being is a necessary condition for a reduction in symptoms and whether a reduction in symptoms is a necessary COMBINE Manuscript Proposal Form For Administrative Use Only MS # O04 Date Received: 12/3/04 Date Reviewed: Priority Set: Scheduled for Review: Action: condition for an improvement in functioning. Outcomes will first be operationalized by categorizing participants as improved versus non-improved (in relation to baseline values) on each measure at each time period. The assessment of change in clinical status (improved versus not improved) will follow procedures used by Cisler and colleagues (Cisler, Kowalchuk, Saunders, Zweben & Trinh, Under review; Cisler & Saunders, 2000; Saunders & Cisler, 2000). In order to examine the causal relationship between any two outcome variables, a 2 X 2 cross-classification table will be generated. Rows will represent improvement or non-improvement on one variable (e.g., subjective well-being) and the columns will represent improvement or non-improvement on a second variable (e.g., symptoms). The hypothesis to be tested in this example, will be that if improvement in subjective well-being is a necessary condition for improvement in symptoms, there should be no (or relatively fewer) participants who show improvement in symptoms who do not show improvement in well-being. Similar analyses will examine the relationship between symptoms and functioning. Separate analyses will be conducted to examine persistence of effects over longer term follow-up with psychosocial functioning being the primary measure considered for assessing sustained or longer-term effects of treatment after the four-month treatment period has ended. Finally, subjective well-being can also be used to identify treatment responders and treatment non-responders. Along with other measures such as the POMS, patient side effects and adverse reactions, subjective wellbeing could indicate whether patients are responsive to, in particular, the medications provided in the study. References: Cisler, R. A., & Berger, L. (2001). Assessing Alcoholism Treatment Composite Outcome: Further evidence utilizing brief measures. Journal of Mental Health, 10(6), 657-672. Cisler, R. A., Kowalchuk, R. K., Saunders, S. M., Zweben, A., Trinh, H. Q. (Under review). Clinical significance of Project MATCH: Determining individual-level functional and reliable outcomes in alcoholism treatment research. Alcoholism: Clinical and Experimental Research. Cisler, R. A., Kivlahan, D. R., Donovan, D., & Mattson, M. E. (In press). Assessing non-drinking outcomes in combined pharmacotherapy and psychotherapy clinical trials for treatment of alcohol dependence. Journal of Studies on Alcohol. Cisler, R. A., & Saunders, S. M. (2000). Analysis of clinically significant and reliable change outcomes in Project MATCH. Alcoholism: Clinical and Experimental Research, 24(5, Supplement), Abstract 201, 40A. Cisler, R. A., & Zweben, A. (1999). Development of a composite measure for assessing alcohol treatment outcome: Operationalization and validation. Alcoholism: Clinical and Experimental Research, 23(2), 263-271. Donovan, D., Mattson, M. E., Cisler, R. A., Longabaugh, R., & Zweben, A. (In press). Quality of life in alcoholism treatment clinical trials. Journal of Studies on Alcohol. Feragne, M. A., Longabaugh, R., & Stevenson, J. F. (1983). The Psychosocial Functioning Inventory. Evaluation in Health Professions, 6, 25-41. Flannery, B. A., Allen, J. P., Pettinati, H. M., Rohsenow, D. J., & Cisler, R. A., & Litten, R. Z. (2002). Using acquired knowledge and new technologies in alcoholism treatment trials. Alcoholism: Clinical and Experimental Research, 26(3), 423-429. Howard, K. I., Lueger, R. J., Maling, M. S., & Martinovich, Z. (1993). A phase model of psychotherapy outcome: Causal mediation of change. Journal of Consulting and Clinical Psychology, 61(4), 678-685. Howard, K. I., Moras, K., Brill, P. L., Martinovich, Z., & Lutz, W. (1996). Evaluation of psychotherapy: Efficacy, effectiveness, and patient progress. American Psychologist, 51(10), 1059-1064. Saunders, S. M., & Cisler, R. A. (2000). The Clinical Significance of Project MATCH. Society for Psychotherapy Research Annual Meeting. Chicago, IL. (June). Seligman, M. E. P. (1995). The effectiveness of psychotherapy: The Consumer Reports study. American Psychologist, 50(12), 965-974. Zweben, A., & Cisler, R. A. (2003). Clinical and methodological utility of composite outcome measures in alcoholism treatment research. Alcoholism: Clinical and Experimental Research, 27(10), 1680-1685.