Urticaria-patient-information-English
advertisement

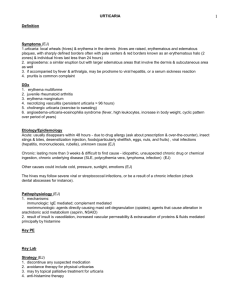
URTICARIA PATIENT INFORMATIONSee more articles » Your disease is called "Urticaria" which in layman’s term is also called hives. In it you get raised areas of the skin that itch intensely and are red with a pale center. This is a common condition and although looks scary is most of the time not serious. About 20 percent of people may have hives at some time during their lives. Urticaria is classified as acute and chronic What is acute urticaria? Acute urticaria - if it develops suddenly and lasts less than six weeks. Most cases last 24-48 hours. About 1 in 6 people will have at least one bout of urticaria in their life. It can affect anyone at any age. Some people have recurring bouts of acute urticaria. What does the rash of acute urticaria look like? The rash usually appears suddenly and can affect any area of skin. Small raised areas called weals (or wheals) develop on the skin. The weals look like mild blisters and they are itchy. Each weal is white or red and is usually surrounded by a small red area of skin which is called a flare. The weals are commonly 1-2 cm across but can vary in size. There may be just a few but sometimes many develop over various parts of the body. Sometimes weals next to each other join together to form larger ones. The weals can be any shape but are often circular. As a weal fades, the surrounding flare remains for a while. This makes the affected area of skin look blotchy and red. The blotches then fade gradually and the skin returns to normal.Each weal usually lasts less than 24 hours. However, as some fade away, others may appear. It can then seem as if the rash is moving around the body. The rash may appear quite dramatic if many areas of skin are suddenly affected. Are there any other symptoms? Most people with acute urticaria do not feel ill, but the appearance of the rash and the itch can be troublesome. In some cases a condition called angio-oedema develops at the same time as urticaria. In this condition some fluid also leaks into deeper tissues under the skin, which causes the tissues to swell. The swelling of angio-oedema can occur anywhere in the body but most commonly affects the eyelids, lips and genitals. Sometimes the tongue and throat are affected and become swollen. The swelling sometimes becomes bad enough to cause difficulty breathing. Symptoms of angio-oedema tend to last longer than urticarial weals. It may take up to three days for the swollen areas to subside and go. A variation called urticarial vasculitis occurs in a small number of cases. In this condition the weals last more than 24 hours, they are often painful, may become dark red, and may leave a red mark on the skin when the weal goes. What causes acute urticaria? A trigger causes cells in the skin to release chemicals such as histamine. These chemicals cause fluid to leak from tiny blood vessels under the skin surface. The fluid pools to form weals. The chemicals also cause the blood vessels to open wide (dilate) which causes the flare around the weals. The trigger is not known or identified in about half of cases. Some known triggers include: Allergies - for example: Food allergies such as allergies to nuts, strawberries, citrus fruit, egg, food additives, spices, chocolate, or shellfish. Sometimes you can develop an allergy to a food even if you have eaten it without any problem many times before. Allergies to insect bites and stings. Allergies to medicines such as penicillin, aspirin, anti-inflammatory painkillers, etc. A viral infection such as a cold or flu can trigger an urticarial rash in some people. (You react to the virus.) A mild viral infection which causes few other symptoms is probably a common trigger of an urticarial rash that develops without an apparent cause. Skin contact with sensitisers causes a local area of urticaria in some people. For example, chemicals, latex, cosmetics, plants, ointments, etc. Physical urticaria. This is a type of urticaria in which a rash appears when the skin is physically stimulated. The most common is called dermatographism when a rash develops over areas of skin which are firmly stroked. Sometimes an urticarial rash is caused by heat, cold, emotion, exercise, or strong sunlight. Is acute urticaria serious? Usually not. The rash is itchy but normally fades within a day or so and causes no harm. Most people with acute urticaria do not feel too unwell unless they have a cold or flu that is triggering the rash. The cause of the rash is not known in more than half of cases and it is commonly a one-off event. However, urticaria may be more serious in the following situations: Food allergy. If a food allergy is the cause then the rash is likely to return each time you eat the particular food. This is more often a nuisance than serious. Severe allergies. People who have a severe allergic reaction to peanuts, insect stings etc, often have an urticarial rash as one of the symptoms. This is in addition to other symptoms such as severe angio-oedema, breathing difficulties, collapse, etc. A severe allergic reaction is called anaphylaxis. Start a discussion » What is the treatment for acute urticaria? Often no treatment is necessary as the rash commonly goes within 24-48 hours. A cool bath or shower may ease the itch. Calamine lotion or menthol 1% in aqueous cream can help with itching, although if it is left on for too long the itch may come back. It can be bought without a prescription. Antihistamine tablets can ease symptoms. Antihistamines block the action of histamine which is involved in causing urticaria. You can get antihistamines on prescription. You can also buy them from pharmacies. There are several brands. The pharmacist will advise: Modern brands usually work well and are unlikely to cause side-effects. They sometimes cause drowsiness - particularly if you drink alcohol. Older brands will often make you drowsy - but this effect may be welcome at bedtime if itch is troublesome. If you can identify a trigger such as a food, then it would be sensible to avoid it in the future. A short course of steroid tablets is sometimes prescribed in severe cases to help reduce swelling in the skin. If extra control is needed you may be prescribed an antileukotriene medicine. These medicines also help to block the action of histamine and are intended to be taken with antihistamines. If you have a severe episode of urticaria then you may be referred to a skin specialist. Skin specialists (called dermatologists) or allergy specialists (called immunologists) may be able to help. In particular, if angio-oedema or anaphylaxis occurred at the same time, you would be referred or admitted to hospital. This is to confirm the diagnosis, and where possible, to identify a cause. You may then be given advice on how to avoid the cause, and on what to do if it should occur again. What is chronic urticaria? Chronic urticaria - if it persists long-term. In chronic urticaria a rash develops on most days for at least six weeks. This is uncommon. About 1 in 1,000 people develop chronic urticaria at some stage in their life. It is more common in women than it is in men. Some people have an urticarial rash on and off for months, or even years. What does the rash of urticaria look like? The rash can affect any area of skin and is same as acute urticaria. There may be just a few but sometimes many develop over various parts of the body. Are there any other symptoms? The appearance of the rash and the itch can cause distress. A related condition called angio-oedema occurs from time to time in some people with persistent (chronic) urticaria. In this condition some fluid also leaks into deeper tissues under the skin, which causes the tissues to swell. What causes chronic urticaria? A trigger is thought to cause the release of chemicals (such as histamine) from cells in the skin. The trigger is not known or identified in many cases. Possible causes in some cases include the following: In many cases the cause may be an autoimmune problem. Autoimmune means that our own immune system causes damage to some of our body's own cells. In autoimmune diseases the body makes similar antibodies (autoantibodies) that attack its normal cells. In urticaria, these antibodies attach to cells under the skin and cause them to release histamine and other chemicals. The reason why this happens is not clear. An allergy to a food, medicine or parasite (such as worms in the gut) is an uncommon cause of persistent (chronic) urticaria. Physical urticaria. This is a type of urticaria in which a rash appears when the skin is physically stimulated. The most common example of this is called dermatographism (dermatographia) - a rash develops over areas of skin which are firmly stroked. In other cases an urticarial rash is caused by heat, cold, emotion, exercise, or strong sunlight. This kind of urticaria often causes bouts of sudden-onset (acute) symptoms, but sometimes causes chronic symptoms. A germ (bacterium) called Helicobacter pylori (H. pylori) which is commonly found in the stomach may be a factor in some cases. Is chronic urticaria serious? The rash is usually itchy. Each weal usually lasts less than 24 hours. However, as the rash may constantly come and go, the ongoing itch may cause distress and difficulty sleeping. What is the course and outcome (prognosis) of chronic urticaria? Persistent (chronic) urticaria tends to come and go. You may have times when the rash appears on most days, and then times when the rash may go away for a while. The severity of the rash and itch varies from person to person. Some things such as heat, cold, menstrual periods, stress, or emotion may make the rash flare up worse than usual. Symptoms may go away completely after a few months, but the condition lasts several years in some cases. In about half of cases, symptoms go within 3-5 years after it first starts. In about 1 in 5 cases the symptoms persist on and off for more than 10 years. What are the treatments for chronic urticaria? Antihistamine tablets The release of histamine under the skin is involved in causing urticaria. Antihistaminesblock the action of the histamine. Most affected people have at least partial relief, and sometimes total relief, of their symptoms with antihistamines. There are various antihistamines: Some older ones tend to cause drowsiness, but may be useful to take at bedtime. Modern antihistamines are less likely to cause drowsiness. If needed, you can take them regularly. Some people take an older sedating antihistamine at bedtime, and a modern nonsedating one during the daytime. Some people respond to one antihistamine better than another. If one antihistamine has not helped much, a different one may suit better. It is usually worth trying an antihistamine for 1-2 weeks before deciding if it helps or not. Some people take antihistamines 'as required' when symptoms flare up. However, if the rash usually develops on three or more days each week, it is best to take the antihistamine every day whether the rash is present or not. This is to prevent the rash and itch from developing rather than taking medication now and then in response to a rash that develops . Soothing the rash Creams such as menthol in aqueous cream are useful to cool the skin and help to relieve itch. Calamine lotion can also help. A tepid bath or shower may relieve the itch before bedtime and help you to sleep. Avoiding triggers or aggravating factors Occasionally a trigger such as a food is identified which causes the rash. You may then be able to avoid it. However, it is unusual to identify a trigger. For example, if a food trigger is suspected, then you may be asked to keep a food diary to try to identify which food is responsible. Try avoiding tight clothes, as weals sometimes tend to occur at sites of local pressure. For example, under belts, under tight-fitting shoes, etc. Rubbing or scratching: Avoid harsh soaps and tight clothing. Frequent bathing may reduce the problem of dry skin, which can cause itching and scratching that can aggravate this condition. Change in temperature: If your hives are caused by cold, you should not swim alone. If you have severe cold urticaria, you should not swim at all. Sun exposure: Wear protective clothing and apply sun block when outdoors. Try keeping cool, as urticaria may tend to flare up in warmer conditions. In particular, keep the bedroom cool at night. Some things worth considering include: alcohol, hot baths, strong sunlight, and undue emotion. If you think any of these are making symptoms worse then it may be helpful to avoid them. See a doctor if you think a medicine is making symptoms worse, as a change in medication may be an option. Some medicines that may be triggers include aspirin,anti-inflammatory painkillers, codeine,etc. Steroid tablets Steroids reduce inflammation and may ease urticaria. However, it is not a usual treatment due to the serious side-effects which are likely to occur if you take steroids regularly. A short course of steroids may be advised occasionally for a bad flare-up of symptoms. Start a discussion » Other treatments Various other treatments have been tried with variable success. One may be advised by a specialist. For example: Strict diets which avoid possible food triggers. Pills which suppress the immune system (immunosuppressant therapy eg,( ciclosporin.) Other medicines which have limited evidence of working in most cases, but may work in a few cases. If relevant, clearing H. pylori infection of the gut . Treatment of associated angio-oedema Antihistamines usually help to reduce the swelling of angio-oedema. Occasionally, an adrenaline injection and emergency hospital treatment are necessary if the swelling affects the throat and breathing becomes difficult. URTICARIA TESTING Most people with hives do not need any testing. The diagnosis is usually based on their symptoms and a physical examination. However, tests may be recommended if hives do not resolve within six weeks Full blood count to identify eosinophilia caused by allergy or parasitic infestation, and low white blood count from systemic lupus erythematosus. Thyroid antibodies and function in chronic urticaria if autoimmune origin is considered likely. Skin prick testing and blood tests for specific allergy (RAST, or radiollergosorbent tests, or CAP fluoroimmunoassay). Autologous serum skin prick test (if available) in chronic urticaria. Complement tests in case of angioedema without urticaria or urticarial vasculitis. Skin biopsy if weals are prolonged, to identify vasculitis. . . . .