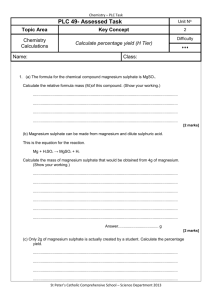
Can magnesium sulphate be given
advertisement

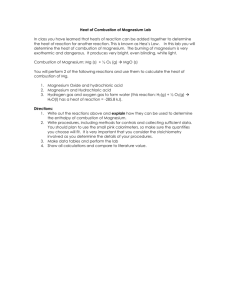
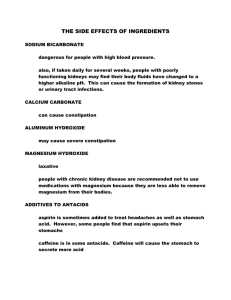
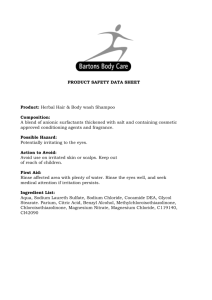
Medicines Q&As Q&A 14.4 Can magnesium sulphate be given subcutaneously? Prepared by UK Medicines Information (UKMi) pharmacists for NHS healthcare professionals Before using this Q&A, read the disclaimer at www.ukmi.nhs.uk/activities/medicinesQAs/default.asp Date prepared: 25th July 2011 Background Hypomagnesaemia can arise from a variety of causes. Some of the commonest include gastrointestinal disorders characterised by malabsorption or chronic fluid loss, various renal diseases and persistent hypercalcaemia. The reference range for plasma magnesium is approximately 0.65 – 1.1 mmol/L. Sometimes it is impossible or inconvenient to use either the oral or intravenous routes to correct deficiency. This can be the case, for example, in patients with chronic intestinal malabsorption of magnesium who are regularly admitted to hospital with symptomatic hypomagnesaemia for intravenous replacement. If it were possible to offer patients such as these regular subcutaneous magnesium, then repeated admissions to hospital could be avoided. Answer Unlike electrolytes such as calcium and potassium, the parenteral administration of magnesium salts has not been widely associated with local tissue damage during use of concentrated solutions or following extravasation. The reduced propensity to cause tissue damage is supported by the fact that in the US magnesium sulphate 50% solution is given intramuscularly to treat hypomagnesaemia (1). In mild deficiency, a common adult dose is 1g (4mmol) IM every 6 hours, for four doses. However, in severe deficiency, doses as high as 0.5mL/Kg bodyweight of the 50% solution can be given within a 4 hour period by multiple IM injections. The injection may be painful and it is clearly not a suitable longterm option in patients suffering from chronic hypomagnesaemia, but the tolerance of human tissues to these very high local concentrations of magnesium suggest that subcutaneous administration could be possible. Some further credence to this approach is given by the fact that subcutaneous magnesium sulphate has been used in animal studies. High doses (up to 1000mg/Kg) have been given to rats subcutaneously in studies, but unfortunately the concentrations used are not documented (2,3). In a 1991 case report a 63-year old patient, who developed severe and persistent hypomagnesaemia following a total regional pancreatectomy, was successfully treated for 24 months with subcutaneously administered magnesium sulphate (4). The dose was titrated to magnesium sulphate 14mmol (8ml) and 7ml of sterile water administered subcutaneously via a microinfusion pump over 10 hours overnight. On one occasion two 1-cm dark coloured superficial skin abscesses were reported, which were attributed to a delayed absorption as a result of the needle being placed too superficially. No further skin complications occurred and serum magnesium levels were maintained within a low normal range. A paper in 2000, described a 28-year old man with combined intestinal malabsorption of magnesium and excessive renal loss (5). This resulted in a perpetually low plasma magnesium, dropping as low as 0.4mmol/L, which caused recurrent seizures. Daily administration of a short intravenous magnesium sulphate infusion was insufficient to maintain plasma levels of magnesium because it was eliminated by the body too quickly. However, continuous subcutaneous infusion of magnesium sulphate maintained plasma levels within the normal range (variation approx 0.67 - 0.83mmol/L over 6 days). The magnesium sulphate was prepared as a 10% solution in 20mL and was given at a rate of 0.3mmol/hr via a portable infusor. There were no local reactions and the patient learned to self administer the infusion. Although no specific time period is given, the authors note that the patient remained symptom free in the days after discharge from hospital. From the NHS Evidence website www.evidence.nhs.uk 1 Medicines Q&As A further case study described a 56-year old woman with a high-output stoma following bowel resections for Crohn’s disease, who had persistent hypomagnesaemia despite intravenous and subsequently oral magnesium supplementation (6). She was treated with twice-weekly home subcutaneous saline (1 litre) and magnesium (4mmol) infusion, together with oral 1α-hydroxycholecalciferol (500 nanograms/day), which maintained her serum magnesium levels. The infusion rate and duration of treatment are not stated. In a more recent case report, a 71-year old man with a high-output ileostomy and subsequent hypomagnesaemia was treated initially in hospital with subcutaneous magnesium sulphate 12mmol in one litre of saline over 12 hours (7). He was then discharged home and self-administered subcutaneous infusions of 500ml of saline solution with 3mmol of magnesium sulphate over 6 hours each day. Serum magnesium levels maintained within the normal range for 137 days after discharge were reported. One study of eight patients who self-administered overnight subcutaneous rehydration fluids utilised low concentrations of magnesium sulphate (e.g. 2 – 4mmol in 500mL to 1 litre) as a top-up to oral magnesium supplements. This proved safe and effective (8). In the UK, the commonest strength of magnesium sulphate injection is 50% w/v (2mmol/mL), yet an isotonic solution of magnesium sulphate is 6.3% w/v in water (25.2mmol in 100mL) (9). It would seem a wise precaution if considering the administration of magnesium subcutaneously, to start by using isotonic solutions where possible. This would reduce the likelihood of pain or tissue damage at the injection site. One report has suggested that, since magnesium sulphate is a salt and may cause skin irritation, it should only be given in the abdominal subcutaneous adipose tissue, together with site rotation (4) Summary Despite little published clinical experience in humans, the properties of magnesium sulphate suggest that the subcutaneous route of administration could be explored in individual cases where other routes are impractical or impossible. The concentration should be kept as low as possible and ideally should not greatly exceed 6.3%. Administration in the abdominal subcutaneous adipose tissue has been suggested in one report (4). This use in the UK is unlicensed. Limitations Despite subcutaneous administration seeming a reasonable approach in theoretical terms, only four case reports and one small study have described its use in humans. There are no data on long-term benefits or harm. References 1) American Society of Health-System Pharmacists. AHFS Drug Information. Electronic edition. Bethesda, Maryland: American Society of Health-System Pharmacists. Accessed via http://www.medicinescomplete.com/ on 25th July 2011. 2) Sirin BH et al. Neuroprotective effects of preischemia subcutaneous magnesium sulfate in transient cerebral ischemia. European Journal of Cardio-Thoracic Surgery 1998; 14:82-88. 3) Katsumata Y et al. A study for effects on pre- and postnatal development, including maternal function in rats treated subcutaneously with magnesium sulfate. Journal of Toxicological Sciences. 1998; 23(SUPPL. 1): 67-79. 4) McDermott KC, Almadrones LA, Bajorunas DR. The diagnosis and management of hypomagnesemia: a unique treatment approach and case report. Oncology Nursing Forum 1991; 18(7): 1145-1152. 5) Aries PM et al. Subkutane Magnesiumpumpe bei einem Patienten mit kombiniertem Magnesiumtransportdefekt. Deutsche Medizinische Wochenschrift 2000; 125: 970-72. (English abstract; original paper translated by Anya Richter, Pharmacy, Southampton University Hospitals Trust.) From the NHS Evidence website www.evidence.nhs.uk 2 Medicines Q&As 6) Tsao SKK, Baker M, Nightingale JMD. High-output stoma after small-bowel resections for Crohn’s disease. Nature Clinical Practice Gastroenterology and Hepatology 2005; 2(12): 604608. 7) Alfaro Martinez JJ, Botella Romero F, Lamas Oliveira C, Hernandez Lopez A. Severe hypocalcemia secondary to hypomagnesaemia, successfully treated by self-administered subcutaneous magnesium. Nutr Hosp 2009;24:354-356. 8) Martinez-Riquelme A et al. Self-administered subcutaneous fluid infusion at home in the management of fluid depletion and hypomagnesaemia in gastro-intestinal disease. Clinical Nutrition 2005; 24:158-163. 9) Wade A (editor). Pharmaceutical Handbook. 19th Edition. London: Pharmaceutical Press;1980 p.257. Quality Assurance Prepared by Kate Pickett, Medicines Q&A Pharmacist (based on earlier work by Dr Simon Wills), Wessex Drug and Medicines Information Centre, Southampton University Hospitals NHS Trust. Date Prepared 25th July 2011 Checked by Nicola Watts, Wessex Drug and Medicines Information Centre. Southampton University Hospitals NHS Trust. (With thanks to Peter Rhodes, Principal Pharmacist for Technical Services, Southampton University Hospitals NHS Trust.) Date of check 5th September 2011 Search strategy Embase (search strategy: [exp MAGNESIUM CHLORIDE/sc or exp MAGNESIUM/sc or exp MAGNESIUM SULFATE/sc] limit to human) Medline (search strategy: [exp MAGNESIUM CHLORIDE/ or exp MAGNESIUM/ or exp MAGNESIUM SULFATE/] and [exp INJECTIONS, SUBCUTANEOUS/] ) Internet Search (Google: magnesium subcutaneous) National electronic Library for Medicines. Accessed via http://www.nelm.nhs.uk/ CINAHL (search strategy: [exp INFUSIONS, SUBCUTANEOUS/ or exp INJECTIONS, SUBCUTANEOUS/] and [exp MAGNESIUM COMPOUNDS/ or MAGNESIUM/ or MAGNESIUM SULFATE/] ) British Nursing Index (1985 onwards) [SUBCUTANEOUS.af and MAGNESIUM.af]. Technical Services expert In-house texts From the NHS Evidence website www.evidence.nhs.uk 3