Antenatal risk assessment
advertisement

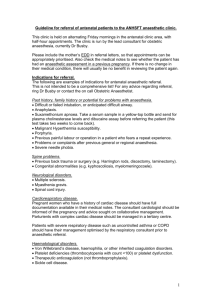
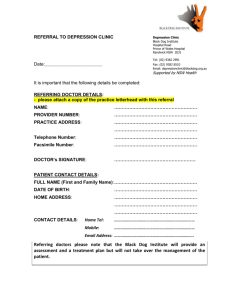
MAT/GUI/0310/ANTASS MATERNITY SERVICE GUIDELINE TITLE: AUTHORS: GUIDELINE LEAD: RATIFIED BY: ACTIVE DATE: RATIFICATION DATE: REVIEW DATE: APPLIES TO: EXCLUSIONS: RELATED POLICIES Clinical Risk Assessment: Antenatal Annie Nowell - Midwife Denise McEneaney - Consultant Midwife/ Supervisor of Midwives Denise McEneaney Guidelines group April 2010 March 2010 March 2013 All maternity staff None Women declining blood products in pregnancy The Management And Treatment Of Clients Refusing Blood Transfusion -BLT/POL/21809/MDR Safeguarding Children THIS DOCUMENT REPLACES 1. INTRODUCTION/PURPOSE OF THE GUIDELINE This guideline provides a framework to describe the process for antenatal and intrapartum risk assessment, in order that women receive standardised and appropriate care dependent on their own individualised needs. Antenatal Risk Assessment The National Service Framework’s guidance on maternity services advises individualised antenatal risk assessment and care planning for all women and their babies. Both CEMACH and NICE have recommended the development of a national standardised risk assessment for all antenatal women. 2. IMPLEMENTATION Paper copy will be attached to guideline and audit notice boards. Emailed copies to all midwives and obstetricians. Will be available via the trust intranet. Circulated to guidelines folders. Page 1 of 16 MAT/GUI/0310/ANTASS 3. ROLES AND RESPONSIBILITIES It is the responsibility of all maternity unit staff to carry out clinical care as described in the guideline unless there is justification for variation and the reason is documented. 4. GUIDELINE This guideline relates to the timing of risk assessments, the management plan and referral process if risk is identified. 4.1.1 TIMING OF ANTENATAL RISK ASSESSMENT 4.1.2 All women should have an initial risk assessment at their antenatal booking appointment with a midwife. Women will be risk assessed by the midwife asking the woman about specific conditions, documenting their response in the pregnancy notes and determining the most appropriate care pathway following local clinical guidelines. This will include identifying if a referral is required to more specialist care of the maternity team. The relevant sections in the maternity include: Lifestyle History - Social Assessment, smoking and drug use Ethnic origin Medical History including Mental Health Family History Previous Births and early pregnancy loss 4.1.2 Women will be offered antenatal screening blood tests at the booking appointment. The results of these tests and next review of the risk assessment will be undertaken at the midwife led Baby and Me Clinic appointment at 11- 13 weeks gestation immediately following the combined screening appointment. 4.1.3 Women admitted antenatally should have an additional risk assessment at every new attendance. 4.1.4 Risk assessment is a dynamic and potentially on-going process as risk factors may arise or be disclosed at any point in pregnancy. Risk assessments can therefore be revised at any stage of pregnancy. 4.1.5 Issues that women do not want to be documented in her handheld records should be documented in the woman's trust records and the confidentiality box (on page 2) should be ticked. 4.2 MEDICAL CONDITIONS TO BE CONSIDERED: 4.2.1 Any medical conditions will be documented in the ‘Medical History’ section of the Pregnancy Notes; this includes anaesthetic history (on page 3). Any issues will be expanded upon in the ‘notes’ section. The following conditions (including anaesthetic problems) are reviewed during the booking appointment: Anaesthetic problems Back problems Cancer Epilepsy/neurological problems Female circumcision Genital infections, including Herpes Page 2 of 16 Asthma or chest problems Blood disorders Diabetes Fertility problems Gastro-intestinal problems i.e. Crohns Gynaecological operations/problems MAT/GUI/0310/ANTASS Heart problems Incontinence – urinary and /or faecal Kidney or urinary problems Migraine or sever headache Pelvic injury Sickle cell or Thalassaemia thrombosis General questions about any other medical problem not listed High blood pressure Infections i.e. MRSA, GBS Liver disease i.e. hepatitis Musculo-skeletal problems Pregnancy problems i.e. cholestasis, HELLP TB exposure Thyroid problems Mental Health 4.2.2 In additional women are asked about the following: Admissions to ITU Allergies Date and result of last cervical smear Previous operations If woman is taking folic acid tablets 4.3 4.4 Admissions to A&E in last 12 months NB – this questions will then prompt the midwife to ask about domestic abuse and should always be done when alone with the woman. See Domestic Abuse guideline for more detail Blood transfusions Exposure to toxic substances Medication in the last 12 months Vaginal bleeding in this pregnancy FACTORS FROM PREVIOUS PREGNANCIES The midwife will document details from previous pregnancies. The history includes whether the current pregnancy is with a new partner. Areas to highlight include: Date, sex, gestation, place of booking/birth The child’s conditions now and where the child lives Antenatal summary, identifying any complications Details of onset of labour, type of anaesthetic (if any) used. Type of birth, details of third stage management and blood loss, type (if any) of perineal tear and repair Detail of labour and postnatal period Type of infant feeding Details of early pregnancy loss LIFESTYLE AND SOCIAL HISTORY The midwife will ask the woman about the following at the booking appointment and record the woman’s response on pages 1 and 2 of the pregnancy notes. (* these questions are repeated in the second and third trimesters). This section includes recording details of: Communication needs and if assistance Marital status required Citizenship status Partner’s details Employment status Housing situation Page 3 of 16 MAT/GUI/0310/ANTASS Support - family, friends Name of Social Worker (if any) *Smoking – type/frequency/stopped in *Drug use – type, frequency, close last 12 months contacts and drug use *Alcohol consumption – pre-pregnancy and current 4.5 FAMILY HISTORY (woman’s children, women’s parents, grandparents, siblings) The midwife will document if there are positive responses to the following questions: Diabetes High blood pressure/eclampsia Thrombosis Consanguinity 4.5.1 In addition the midwife will ask if there are specific questions about the woman and partner’s families including history of familial/hereditary medical conditions, stillbirths/miscarriages, congenital abnormalities, learning disabilities, hearing loss. 4.6 IDENTIFICTION OF WOMEN WHO WILL DECLINE BLOOD AND BLOOD PRODUCTS 4.6.1 At present, Jehovah’s Witnesses form the majority of women who may decline blood and blood products. All women are asked about their religious beliefs and this is recorded on page 2 of the Pregnancy Notes. Women identifying themselves as Jehovah’s Witnesses are asked directly whether they would accept or decline blood and blood products and this must be documented This will prompt midwives to refer women who are Jehovah’s Witnesses to the Obstetric/Anaesthetic High Risk Clinic. All women are asked if they have had any blood transfusions on page 3 of the Pregnancy Notes – any response from the woman indicating that she may decline blood or blood products will prompt the midwife to refer the woman to the maternity team as above. Further details are in the Maternity Guideline (Women declining blood products in pregnancy) and Trust Policy - The Management and Treatment of Clients Refusing Blood Transfusion. 4.7 DEVELOPMENT OF AN INDIVIDUAL MANAGEMENT PLAN 4.7.1 Any risk factors identified in the risk assessment (as outlined above) are documented in the Risk Assessment Section on page 11 of the Pregnancy Notes and a management plan will be agreed. This will be informed by the relevant clinical guidelines and care pathways depending on the risks identified. Appendix 1 contains some guidance on factors to consider when agreeing the management plan. This midwife will document this at the booking appointment and review this at the Baby and Me appointment. 4.7.2 Key factors from the management plan (on page 11) are documented in the key points section (on page 15). 4.7.3 The individual management plan is reviewed at each subsequent antenatal appointment and antenatal admission. The healthcare provider will document this in the Antenatal Visit section (page 15) 4.8 PROCESS FOR REFERRAL OF WOMEN IN WHOM RISKS ARE IDENTIFIED DURING THE CLINICAL RISK ASSESSMENT 4.8.1 The type and method of referral will varying according to the risk identified, and can the form of completion of referral form or requesting specific Page 4 of 16 MAT/GUI/0310/ANTASS appointments. Appendix 1 contains information in risk factor identified, factors to consider and possible referral route for planning subsequent management. 4.8.2 Obstetric Referral Midwives and GP’s can refer directly to the obstetric team by requesting a consultant led appointment in the relevant antenatal clinic session by calling 020 7377 7431. The obstetric team have clinic sessions Monday – Friday in the hospital based Antenatal Clinic as follows: Clinic Mon am Tues am Tues am (1/4) Tues pm Wed am Wed am Thurs am Thurs pm Fri am Lead obstetrician Mr Hogg Miss Beski Mr Khan Mr Khan Mr Wee Mr Aquilina Mr Okaro Miss Sanghi Specialty General obstetrics HIV Barkantine link consultant Medically high risk Anaesthetic high risk Cardiology Neurology Renal Psychiatric, Substance Misuse Twins and other multiples General obstetrics General obstetrics Endocrine Diabetes 4.8.3 Specialist Midwifery referral The service has specialist midwives who provide midwifery care for a specified caseload. GP’s, midwives, obstetricians and other healthcare providers can refer directly to these services as follows: Gateway team Vulnerable women including Mental Health, domestic abuse, teenagers in need, child protection concerns, asylum seekers or refugees Contact: via Gateway Team Referral Form (ring 0207 377 7000 ext. 3486 if further advise needed) Substance Misuse Drug and Alcohol Misuse and HIV positive women Contact: Tel. 020 7377 7000 ext 3470 Diabetes Women known to have Type 1 or 2 Diabetes Contact via Antenatal Clinic on 020 7377 7431 for appointment Antenatal Screening for further support advise re antenatal screening tests Contact Tel 020 7377 7000 ext 2467 Page 5 of 16 MAT/GUI/0310/ANTASS 4.8.4 Children and Families Social Work Team All referrals must be completed by using the Social Work Referral Form, available in all clinic areas. This should be faxed on 020 7377 7416. Telephones advise can be sought be calling 020 7377 7225 and ask for the duty Social Worker. 4.8.5 Smoking Cessation Referral is made to the smoking cessation team by completing the ‘Smokefree’ proforma available in all clinic areas. 4.8.6 Perinatal Mental Health Team Ideally this referral will be facilitated following referral to the Gateway Team Midwives. However, direct referral can be made by completion of referral form available in all clinic areas and faxing this to 020 8121 5636. If there are acute concerns regarding the woman’s mental health, consider referral either to the Crisis Intervention Service (CIS) during office hours (contact via switch) or the Psychiatric Liaison team outside office hours (contact by aircall via switchboard). 4.8.7 Women who will decline blood and blood products Women identified as likely to decline blood products should be referred to the Obstetric/Anaesthetic high risk clinic by calling 020 7377 7431. 4.9 RISK ASSESSMENT FOR APPROPRAITE PLACE OF BIRTH – WOMEN WHO PLAN TO LABOUR OUTSIDE THE CONSULTANT LED UNIT 4.9.1 Women who wish to book for a home birth or the Barkantine Birth Centre are risk assessed at 36 weeks using the proforma (Appendix 2). Women should have this proforma completed and fixed into their pregnancy notes. 4.9.2 Women with risk factors suggesting planned birth on labour ward, who wish to continue to plan a non-hospital birth, are referred to a consultant obstetrician for further care planning. Ideally this should the Barkantine/homebirth link consultant. The midwife should contact the Supervisor of Midwives if support is required in planning care according to the woman’s choice. 4.9.3 Women with risk factors suggesting individual risk assessment should be referred to a consultant midwife or obstetrician for further care planning if they wish to continue planning a non-hospital birth. 4.10 REFERRAL BACK TO MIDWIFERY LED CARE 4.10.1 The specialist team will document their findings and recommendations for future care in the pregnancy notes. If it is appropriate to continue midwifery led care and a midwife led appointment is not already in place, the woman will be asked to contact her community midwife (usually facilitated by contacting the GP surgery/health centre where clinics are held) to arrange an appointment at the specified time. 5 BREACH OF GUIDELINE The incident will be reviewed within the risk management framework. The impact of this incident will be reviewed by the appropriate lead clinician and feedback/training given to staff as required. 6 MONITORING COMPLIANCE Page 6 of 16 MAT/GUI/0310/ANTASS See monitoring template. REFERENCES 1. Confidential Enquiry into Maternity and Child Health. (2004). Why Mother’s Die 2000-2002. London: RCOG Press 2. Confidential Enquiry into Maternity and Child Health. (2007) Saving Mother’s Lives: Reviewing maternal deaths to make motherhood safer 2003-2005. London: CEMACH. 3. National Institute for Health and Clinical Excellence. (2008). Antenatal care: Routine care for the healthy pregnant woman. London: NICE. 4. Royal College of Anaesthetist, Royal College of Midwives, Royal College of Obstetrician and Gynaecologists, Royal College of Paediatrics and Child Health. (2007). Safer Childbirth: Minimum Standards for the Organisation and Delivery of Care in labour. London: RCOG Press Page 7 of 16 MAT/GUI/0310/ANTASS MONITORING TOOL Elements to be monitored Monitoring lead Monitoring tool Monitoring time frame. Risk assessment completed at booking, 28 weeks and 34 weeks - page 11 of pregnancy notes Medical conditions documented and referred appropriately including factors form other pregnancies Audit and Quality midwife Documentation audit tool 10 sets of notes each month Audit and Quality Midwife Documentation audit tool 10 sets of notes each month Lifestyle, medical conditions and obstetric history noted in risk assessment Management plan in place Audit and Quality Midwife Audit and Quality Midwife Lead MW ANC & Consultant MW Lead MW ANC & Consultant MW Lead MW Gateway team Documentation audit tool 10 sets of notes each month Documentation audit tool 10 sets of notes each month Map referral process against risk factors 1 week of new referrals bi-annually Map referral process 1 week of referrals back to midwife led care bi-annually Map referral process against risk factors 1 week of new referrals bi-annually Lead Obstetric consultant anaesthetist/ lead ANC midwife Map referral process, Advanced Decision form completed and in records Audit tool developed All records for women who decline blood products Referral process: Obstetrics method/timing/appropriate referral Referral back to midwife led care method/timing/appropriate referral Referral process; Gateway team: method/timing/appropriate referral Management plan in place for women who decline blood & blood products Risk assessment completed for all women birthing at home or birth centre Page 1 of 16 Lead midwife BBC Consultant midwife 10 sets of notes each month Committee to receive the report. The Maternity and Gynaecology Audit Committee will receive completed reports. Audit feedback and resultant action plans will be fed back to the maternity and Gynaecology governance Board The leads of the Audit Committee will be expected to read and interrogate the report to identify deficiencies in the record keeping system. Minutes will be clearly documented. Any deficiencies will be addressed through multiprofessional action planning. Actions will be taken through teaching where necessary. The Maternity Services Liaison Committee reviews the Birth Reflections Survey Report each quarter. Action plan lead committe e Acting on recommendation s and Lead(s) The Maternity and Gynaecology Audit Committee will lead on the action plan. Recommendations will be allocated to key areas of practice with identified leads. Required actions will be identified and completed in a specified timeframe and monitored by the Maternity and Gynaecology audit committee. Implementing and sharing best practice Change in practice and lessons to be shared Required changes to practice will be identified and actioned within a specific time frame documented in the agreed action plan. A lead member of the team will be identified to take each change forward where appropriate. Lessons will be shared with all the relevant stakeholders. MAT/GUI/0310/ANTASS APPENDIX 1 Factor Cardiac disease Hypertensive disorders Renal disease Endocrine disorders (excluding diabetes) Diabetes type 1&2 Severe and enduring mental health issues and all women with history of puerperal psychosis Haematologic al disorders Previous VTE Previous anaesthetic problems Autoimmune disorders Epilepsy Severe asthma ANTENATAL RISK ASSESSMENT TOOL Potential risk Suggested management plan Increased cardiovascular demands IUGR Referral to high risk clinic for obstetric, cardiac and anaesthetic review- Tues PM (urgent if symptomatic) Request Uterine Artery Doppler’s at anomaly scan May need anticoagulants Consider referral to Guys for fetal cardiac scan Refer for Uterine Artery Doppler's at anomaly scan Refer to antenatal hypertension clinic- Tues PM Superimposed PET IUGR Increased renal demands Altered requirements of pregnancy Poor pregnancy outcome IUGR Macrosomia Poor diabetic control Fetal cardiac abnormalities Deteriorating mental health Child protection issues Refer to joint diabetic/ obstetric clinic- Fri AM (to be seen within 1 week) Serial growth scans Referral for cardiac scan at Guys IUGR IUD Sickle crises Fetal inheritance Recurrence Refer to high risk clinic If haemoglobinopathy: refer to haemoglobinopathy specialist nurse & screen expectant father for trait Anaesthetic risk if reacting to drugs/ difficult to intubate etc Referral to Obstetric/Anaesthetic high risk clinic or consultant anaesthetic review Miscarriage IUD Referral to high risk clinic- Tues AM Increased fits Teratogenicity of medication Increased cardiovascular demands of pregnancy Need for acute treatment/ deterioration Referral to high risk clinic- Tues AM Referral to epilepsy specialist nurse Refer for serial scans and cardiac scan if medicated Refer to obstetrician if increased need for medication or hospital admission Page 1 of 16 Refer to Gateway team Referral to Social services by 28/40 if concerns about child protection Refer to Perinatal Mental Health team Refer to Crisis Intervention Service if acute concerns (office hours only) or Accident and Emergency for review by Psychiatric Liaison Team (outside office hours) Urgent referral to high risk clinic Refer to substance misuse specialist midwife who will arrange care in Seacole (multidisciplinary substance misuse) clinic Social work referral by 28/40 Serial growth scans Offer Hep C testing if ever used IV Substance misuse (including alcohol, excluding cannabis) HIV Referral to high risk clinic for obstetric review - Tues PM Request Uterine Artery Doppler’s at anomaly scan Check thyroid function and refer to joint endocrine clinic as appropriate- Fri AM (urgent if symptomatic) Vertical transmission Long term implications Specific medical issues Refer to specialist midwife. Clinic includes: obstetrician, HIV physician, HIV specialist nurse, Health advisers and neonatologist. MAT/GUI/0310/ANTASS Hepatitis B Obesity (BMI over 30) Underweight (BMI less than 18) Smokers Aged ≤40 years Aged < 18 years Socially vulnerable women (learning disabilities, asylum seekers, child protection issues) Disclosed domestic violence Recurrent (3+) miscarriages Preterm birth Severe preeclampsia, HELLP or eclampsia Rhesus isoimmunisation or other significant blood group antibodies Uterine surgery: caesarean section, Page 2 of 16 Long term implications Transmission to baby Gestational diabetes Raised BP VTE IUGR Anaesthetic risk Difficulty assessing fetal growth / presentation IUGR Anaemia IUGR Abruption Prematurity Anxiety Congenital abnormality/ies Social issues SIDS Child protection issues IUGR Mental health issues Anxiety Abruption Child protection issues Mental health issues Cervical incompetence Miscarriage Premature delivery Autoimmune disorders Preterm birth Maternal anxiety Recurrence IUGR Repeat identified sample (personally take blood and confirm details on blood bottle with woman) and LFTs Refer to hepatologist Offer referral to dietician Refer for GTT at 26/40 If BMI 35 or above refer for anaesthetic review Offer referral to dietician Refer for Doppler’s at anomaly scan Offer carbon monoxide testing Counsel regarding risk Offer referral to smoking cessation Counsel regarding screening tests Lower threshold for referral to obstetricians if other factors arise Refer to Gateway team Refer to Family Nurse Partnership Team (NHS Tower Hamlets) Refer to Gateway team Referral to social services by 28/40 if child protection issues Tick confidentiality box. Do not document in handheld records. Refer to Gateway Midwifery team Give immediate safety advice Consider immediate social work referral if existing children or by 28/40 if primip Referral to obstetrician in early pregnancy Referral to Emergency Gynaecology Unit for early pregnancy scan (7+ weeks) Consider reason for preterm birth and risk of recurrence Offer cervical length scan at 16/40 Offer Doppler's at anomaly scan Refer to obstetrician Consider commencing aspirin 75mg Refer for Doppler's at anomaly scan Refer to obstetricians (urgency dependent on historic gestation of onset and current clinical picture) Fetal anaemia Miscarriage IUD Referral to Fetal Medicine Rupture Repeat c/s Placenta previa Placenta accreta If first pregnancy since CS or 2CS refer to VBAC clinic If has had a subsequent vaginal birth can have VBAC discussion in community If 3 uterine surgeries or classical incision refer to obstetricians MAT/GUI/0310/ANTASS myomectomy, cone biopsy 4th degree tear or persistent urinary or faecal incontinence following birth APH x2 Para 5+ Previous stillbirth or neonatal death of unknown cause Previous stillbirth or neonatal death Recurrence Deterioration Referral to obstetricians Recurrence Consider referral to obstetrician Anaemia Unstable lie PPH Recurrence Anxiety Treat anaemia proactively Refer to obstetricians if unstable lie ≥37/40 Discuss sterilisation should c/s occur Refer to obstetricians GTT at 26/40 Recurrence Anxiety Consider referral to Fetal Medicine Consider referral to geneticist Refer to obstetricians Recurrence Consider aspirin 75mg Referral for Doppler's Refer to obstetricians Monitor growth closely and refer for growth scan if concerns Recurrence Shoulder dystocia C/s GTT at 26/40 Monitor growth closely and refer for growth scans if concerns Recurrence Anxiety Consider referral to fetal medicine Consider GTT at 26/40 Referral to obstetricians GP to remove at 12/40 if easy Urgent referral to Emergency Gynae Unit if pain prior to USS USS and referral to obstetrician Refer to obstetrician- urgency as appropriate due to a recurrent or genetic cause Small for gestational age infant, IUGR or BW less than 2.5kg Large for gestational age, BW 4.5kg+ (4.0kg if South Asian) Congenital abnormality IUCD in situ Fibroid Female genital mutilation/ FGM Previous gestational diabetes First degree Page 3 of 16 Eptopic Miscarriage Premature labour Pain Malpresentation Obstructed labour Premature labour Cancer Difficulty with internal examinations Obstructed labour Refer to obstetricians who will assess need for referral for antenatal reversal at Sylvia Pankhurst Recurrence GTT at 16/40 Gestational diabetes GTT at 26/40 MAT/GUI/0310/ANTASS relative with diabetes Glucosurea once before 20 weeks for twice after 20 weeks or high random blood sugar Rhesus negative with no antibodies Page 4 of 16 Gestational diabetes Refer for GTT Rhesus iso-immunisation Referral for anti D at 28/40 APPENDIX 2 Name: Sign MRN: Gest: Risk assessment completed by: Print Date + /40 / / If yes not suitable for non-hospital birth If O yes refer to consultant midwife or obstetrician for opinion Indications of increased risk suggesting planned birth on labour ward Disease area Medical condition Indications of increased risk suggesting planned birth on labour ward Other factors Additional information Cardiovascular Current Respiratory Haematological Infective Immune Endocrine Renal Neurological Gastrointestinal Psychiatric Other factors Previous compl icatio ns Page 5 of 16 Confirmed cardiac disease Hypertensive disorders Yes □ No □ Asthma requiring increase in treatment or hospital treatment Cystic fibrosis Yes □ No □ Haemoglobinopathies – sickle cell, beta thalassaemia major History of thromboembolic disorders Immune thrombocytopenia purpura, other platelet disorder or platelet count below 100,000 Von Willebrand’s disease Bleeding disorder in woman or fetus Atypical antibodies with a risk of haemolytic disease in the baby Yes □ No □ Group B strep risk factors where antibiotics in labour would be recommended (GBS+ in current pregnancy, previous baby with GBS disease, PPROM in GBS+ woman, choroamnionitis) Hepatitis B/C with abnormal LFTs HIV positive Currently infected with or receiving treatment for: ● Toxoplasmosis ● Genital herpes ● Tuberculosis ● Chicken pox ● Rubella Yes □ No □ SLE Scleroderma Yes □ No □ Any endocrine condition Yes □ No □ Abnormal renal function Renal disease requiring supervision by a renal specialist Epilepsy Myasthenia gravis Previous cerebrovascular accident Liver disease with current abnormal LFTs Psychiatric disorder requiring current inpatient care Additional information Unexplained stillbirth or death or related to intrapartum difficulty PET requiring preterm birth Placental abruption with adverse outcome Eclampsia Uterine rupture PPH requiring additional treatment or blood transfusion Retained placenta requiring manual removal in theatre Caesarean section Shoulder dystocia Previous baby: -With neonatal encepholopathy -Over 4kg Major gynaecological surgery: Myomectomy Hysterotomy Previous 4th degree tear Yes □ No □ Yes □ No □ Yes □ No □ Yes □ No □ Multiple pregnancy Para 5 or more Placenta praevia Pre-eclampsia or pregnancy induced hypertension Preterm labour or preterm rupture of membranes Placental abruption Fibroids Anaemia of less than 10.0g/dl at onset of labour Confirmed intrauterine death Induction of labour Substance misuse (including alcohol dependency) Gestational diabetes requiring medication or with suboptimal BM control or with suspected macrosomia (see diabetes guideline) Malpresentation: breech transverse or oblique lie BMI at booking of greater than 35 Recurrent antepartum haemorrhage Small for gestational age (less than the 5th percentile, reduced growth velocity or current SFH ≥3cm less than gestational age in weeks and no ultrasound performed in last 4 weeks). Abnormal Doppler’s Abnormal fetal heart rate Ultrasound diagnosis of olgio or polyhydramnios Indications for individual risk assessment when planning place of birth Cardiovascular Cardiac disease without intrapartum complications Haematological Atypical antibodies without risk of haemolytic disease of the newborn Sickle cell or thalassaemia trait Infective Hepatitis B/C with normal LFTs Endocrine Unstable hypothyroidism requiring a change in treatment Skeletal/ Spinal abnormalities neurological Previous fractured pelvis Neurological deficits Gastrointestinal Liver disease with normal LFTs Crohn’s disease Ulcerative colitis Previous Neonatal death with a known none recurrent cause compli Pre-eclampsia developing at term cation Placental abruption with a good outcome s Extensive vaginal, cervical or third degree tear or trauma Previous term baby with jaundice requiring exchange transfusion Previous Antepartum bleeding of unknown origin once after 24/40 compli Recreational drug use cation Current out-patient psychiatric care s Maternal age ≥40 years Fetal abnormality pregna ncy Yes □ No □ Yes O No O Yes O No O Yes O No O Yes O No O Yes O No O Yes O No O Yes O No O Yes O No O Page 6 of 16