Nursing Process - LaGuardia ePortfolio
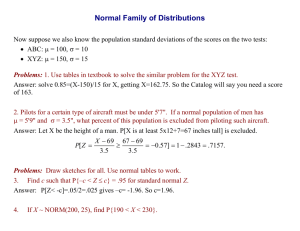
advertisement

1 LAGUARDIA COMMUNITY COLLEGE City University of New York SCR 210 NURSING PROCESS TOOL Student Name: Louise Margaret Tomas Clinical Date: 05/08/2008 Biographical Data : Client’s Initials: E.J Room: 303 Bed 1 Sex: F Age: 89 years old Religion: Catholic Occupation: Retired Cultural/Ethnic Background: African American Admitting Date: 05/01/08 Reason for Admission: Possible Sacral Osteomylelitis Data - Label S for Subjective, O for Objective R E S T & A C T I V I T Y A. Rest: (Usual, alterations assoc. with illness/hospitalization) Hours of sleep each night – Unable to access because client is confused and not responding (S) Difficulty falling asleep; early awakening; nap during day; Client was observed napping during the day. (O) manifestations of sleep deprivation Assistive measures: warm milk, medication, etc. - No assistive measures were observed. (S) B. Activity Degree of mobility of all joints; condition of joints – Client is immobile so unable to demonstrate. Client feels pain while moving joints (O) Ability to flex and extend limbs against graduated resistance- Unable to Flex and extend limbs against graduated resistance(O) Hand grasp- bilateral; coordination - Pt. demonstrates normal coordination and bilateral ability to grasp my hands. (O) Ability to stand, assistance needed; posture, gait, balance –Pt is on complete bed rest so not able to stand, complete assistance needed for ADL’s so I couldn’t assess her posture and gait. Might be very poor gait.(O) Assistance needed to transfer, stand, walk and use of assistive devices (cane, crutches, walker, wheelchair)Unable to access because pt is on complete bed rest(O) Ability to perform ADL : Pt need complete assistance for Data Analysis Admitting Diagnosis: Possible Sacral Osteomylelitis Secondary Diagnosis: Not Applicable Surgical Procedure: None Date: N/A Health History: Sacral Decubiti; Dementia; Hypertension (Provide reference) Rest: As people get older tend to take longer to fall asleep, awaken more easily and frequently, and spend less time in deep sleep. Older people are more likely to be awakened because of environmental factors such as noise, pain, nocturia. (Brunner & Suddarth, pg. 235) Pain Chronic pain (chest, joint) clients may interfere with sleep, fatigue and muscle tension and may also affect ADL function. Immobilized body parts produce discomfort or suffering. Once clients suffers from pain there can be serious impairment of functional status, mobility, ADL, social activities and activity tolerance may be reduced. (P&P p 1236) Immobility Reduced mobility will slowly decrease endurance, strength; muscle mass and this long term immobility can develop contracture. (P&P p 1427-1429) Activity: Intact musculoskeletal and neurologic systems are Nursing Diagnosis Risk for disturbed sleep pattern related to hospital environment and joint pain. Risk for disuse syndrome related to immobility, decrease muscle strength, decrease ROM Activity intolerance related to joint pain and muscle weakness as evidence by client exhibiting a pained look on her face when I was flexing her lower extremities. 2 ADL’s (O) Restrictions imposed by health problems/therapeutic modalities- Client has been put on bed rest since she is confused. (O) Other factors that may affect mobility: Fatigue, weakness (O) E L I M I N A T I O N A. Urinary Voiding (Usual, alterations associated with illness and hospitalization) Client has a Foley catheter in place. (O) Frequency, urgency, dysuria - Could not assess since client was confused and unresponsive. (O). Urine: quantity, color, clarity, odor, Sp. G.- Pt has catheter bag and it has 300cc, yellowish in color Lab: urinalysis: BUN: 15 (norm= 8-20 mg/dL); creatinine: 0.8 (norm= 0.6-1.2 mg/dL); Assistive devices (indwelling, external catheter) Structural adaptations; urinary diversions: Pt has foley catheter(O) Retention/bladder distention- No distention observed. (O) Other factors that may affect normal urinary elimination - HTN, medications, sedentary lifestyle. (O) B. Bowel Evacuation patterns (Usual, alterations associated with illness & hospitalization) – Unable to assess. Last BM – 05/08/2008 (O) Stool: quality, color, consistency, presence of blood, mucusStool was brown soft and mushy in texture; no mucus or blood was observed. (O) Assistive measures: laxative, enemas, suppositories - essential for maintenance of safe mobility and performance of ADL’s. Age–related changes that affect mobility include alterations in bone remodeling, leading to decreased bone density, loss of muscle mass, deterioration of muscle fibers and cell membranes, and degeneration in the function and efficiency of joints. (Brunner & Suddarth, pg. 235) FUNCTIONAL INCONTINENCE Functional incontinence is involuntary , unpredictable passage of urine in a client with intact urinary and nervous system. Changes in environment; sensory, cognitive, or mobility deficits. Symptoms include urge to void that causes loss of urine before reaching appropriate receptacle. (P&P, p. 1394) Age and Immobility People may have special problems with incontinence because of physical limitations and environmental barriers. Older persons with restricted mobility have greater chances of being incontinent because of their inability to reach toilet facilities in time. (P&P, p. 1329) and also lose muscle tone in the perineal floor and anal sphincter. Although the integrity of the external sphincter may remain intact, older adults may have difficulty controlling bowel evacuation and are at risk for incontinence. (P&P, p. 1377) Self-care deficit related to pain, and weakness as evidenced by complete assistance is needed in performing in ADL’s Impaired urinary elimination related to immobility, age, decreased muscle tone as evidenced by client is in complete bed rest and has Foley catheter. 3 None. (O) Bowel sounds- Presence of normal bowel sounds (b/w 520/min) in all 4 quadrants. (O) Abdomen: distension, firmness, tendernesss - The abdomen is firm but not distended or tender. No protrusions nor distortions noted (O) Structural adaptations; Ostomies - Pt has no ostomies. (O) Other factors that may affect normal bowel elimination Nutrition, medications and inadequate exercise. Urinary: About one third of elderly people show no decrease in renal function. Therefore, changes in renal function may be a combination of aging and pathological conditions such as hypertension. Older adults who take medications may experience serious consequences due to decline in renal function because of impaired absorption, decreased ability to maintain fluid and electrolyte balance, and decreased ability to concentrate urine. (Brunner & Suddarth pg. 233) Immobility and constipation Clients confined to bed are often constipated. Physical activity promotes peristalsis, whereas immobilization depresses peristalsis. Weakened abdominal and pelvic floor muscle impairs the ability to increase intraabdominal pressure and to control the external sphincter. muscle tone may be weakened or that impairs nerve transmission so patient are more prone to constipate.(P&P p 1337) Diet, Age and Constipation Regular daily food intake helps maintain a regular pattern of peristalsis in the colon. Fiber, the indigestible residue in the diet, provides the bulk of fecal material. Diet with low residue which move more slowly through the intestinal tract and can’t create sufficient residue of waste products to stimulate the reflex for defecation. With aging, stool passes through the intestines at a slower rate and the perception of stimuli that produce the urge to defecate often Risk for constipation r/t immobility, age medication, diet, low fluid intake 4 diminishes.(P&P p 1377) A C C E P T A N C E A C C E P T A N C E Affect: withdrawn, sad, cheerful, angry, blank expression- Client is confused and unresponsive to questions. (O) Ability to communicate (verbal & non-verbal) – Client was not able to communicate. (O) Barriers to communication: language, facility, aphasia, tracheotomy/E.T. tube, perceptual impairments, developmental disorders, etc.- Client is confused and unresponsive. (O) Primary language /ability in English- English (O) Understanding of health status/reason for hospitalizationUnable to assess. Any manifestation of anxiety/describe behavior- Unable to assess. Coping mechanisms used- Unable to assess. Self concept/body image; self esteem- Unable to assess. Family constellation/role within family; living arrangements; significant others – Unable to assess. Stage of growth and development: achievement of developmental tasks; give evidence- Unable to assess. Family situation: recent changes or crises - Unable to assess. Hobbies- Unable to assess. (O) Level of education – Unable to assess.(O) Cultural/ethnic influences – Unable to assess (O) Formal religion; spiritual needs- Unable to assess. (O) Economic situation (socioeconomic status) - Unable to assess. (O) Occupation: specific role – Unable to assess. Support systems: church groups, AA, etc. Unable to assess. (O) Patterns of sexual function (alterations associated with illness) - Unable to assess. (O) Stress and coping: Common stressors of old age include normal aging changes that impair physical function, activities and appearance; disabilities from chronic illness; social and environmental losses related to income and decreased ability to perform previous roles and activities; and deaths of significant others. (B & S, pg. 229) Anxiety Anxiety may increase or decrease the ability of a person to pay attention. Anxiety is uneasiness or uncertainty resulting from anticipating a threat or danger. When faced with change or the need to act differently, a person feels anxious when there in no one to take care them. (P&P, p. 456) Powerlessnes related to hospitalization and limited mobility as evidenced by pt unable to perform ADL’S. Anxiety related to situational crisis (hospitalization and illness) as evidenced by client’s nonverbal complaint of pain and discomfort. 5 Menstrual history and pattern- Unable to assess. (O) Reproductive history/disorders; menopause historyUnable to assess. (O) Urethral, vaginal discharge- None recorded in chart. (O) S A F E T Y S A F E T Y Allergies: Manifestation- Penecillin and Tynenol Stage of consciousness: alert, confused, drowsy, lethargic, stuporous, and comatose – Client is confused and lethargic. (O) Orientation: person, place, time Unable to assess. (O) Ability to recognize & respond to environmental hazardsUnable to assess. (O) Memory: immediate, recent, remoteRecent: Unable to assess (O) Immediate: Unable to assess. (O) Remote: Unable to assess. (O) Pupillary response: PERRLA - Pt pupils are equal, round and respond to light. (O) Senses: taste, touch, smell, pain, sight, hearingTaste: Unable to assess. (O) Touch: Client sensed when she was touched; but moving her head towards the person who touched her. (O) Pain: Pt feels pain when we are giving her AM care, mostly on the lower extremities(S) Sight: Unable to assess; but no assistive devices were observed Hearing: Client moved head towards my voice when I spoke to her. (O) Assistive devices: glasses, lens, hearing aid – None were observed. (O) Risk for fall “ Risk for falls is significantly higher in older clients “ balance and mobility problems” “ sensory impairment”(visual and hearing problem) (P&P pg 966) Hospitalization: An illness that requires hospitalization or a change in lifestyle is an imminent treat to wellbeing. Older people admitted to the hospital are at high risk for disorientation, confusion, change in level of consciousness, and other symptoms of delirium as well as fear and anxiety. (Brunner & Suddarth, pg. 248) Risk for injury r/t altered vision, poor gait, unknown environment and age . Disturbed sensory perception r/t altered vision AEB client’s confused state. Risk for infection r/t IV Intravenous Infusions: There are numerous hazards that a pt. can infusing in left arm and encounter when receiving IV therapy due to the Foley catheter. introduction of microorganisms. These include local complications like phlebitis, infiltration, hematoma or clotting of the needle and systemic 6 S A F E T Y Symmetry of facial expressions, tongue, smileSymmetrical facial expressions, tongue. (O) Condition of hair, nails, mucous membranes of mouth, nose, and conjunctiva, tongueHair: clean, gray. (O) Nails: Clean, intact, and no cracking on fingernails but toe nails are dry and thickened.(O) MM of mouth, nose, conjunctiva & tongue: pink, intact, and moist. (O) Condition of skin: describe wounds, stages of decubiti, I.V. sites, dressings, scars, rashes, nodules, ecchymosis – Client had a IV line infusing in her Left arm. (O) Stage IV sacra; decubiti ulcer (8x10 cm; 3cm depth). (O) Other factors that may affect skin integrity – Immbobility. (O) Condition of breasts: symmetry, contour, puckering, nipple discharge, gynecomastia- Pt breasts are symmetrical with no abnormalities seen on assessment. (O) Comfort status: itching, burning, nausea, hunger, pain (character, location, onset, duration, relief measures)Unable to assess. (O) Other factors that may affect comfort status – Hospitalization; immobility; (O) Fluid status: IV type and rate, medication added -1000 ml 0.45% NaCl at 50 cc/hr; 5%dextrose I&O: Date: 03/11/08: Intake : IV: not recorded PO: ? S A F Output : Urine: 300cc; Other: none E 05/07/08 Intake: IV: 1000 cc PO: 300 cc of water and 80% of lunch T Output: Urine: Y Skin turgor, rapid weight gain or loss, condition of mucous membranes of mouth- Skin turgor is normal. The MM of the mouth is pink and intact. No weight changes reported. (O) Other factors that may affect fluid and electrolyte status – Medications, nutrition (O) complications which are more serious like infections. (Brunner & Suddarth pg. 290) Skin: With aging changes in appearance and function of the skin include: thinner dermis, decreased subcutaneous fat, decreased blood supply, loss of resiliency and wrinkling. The skin becomes drier and susceptible to injury and infection. (Brunner & Suddarth pg. 233) Dry feet nails A normal healthy nail is transparent, smooth, and convex, with pink nail bed and translucent white tip. Disease can cause changes in the shape, thickness and curvature of the nail.(P&P p. 695). Some people have dry feet because of a decrease in sebaceous gland secretion, dehydration, pf epidermal cells and poor condition of footwear. If foot or mails problems stay unresolved the client can easily become disabled and risk for infection on cracked nails (Brunner & Suddarth p. 1013) Fluid and electrolyte imbalance: Illnesses, trauma, surgery and medications can affect the body’s ability to maintain fluid electrolyte and acid-base balance. Tissue trauma causes fluids and electrolytes to be lost from damaged cells. Medications and other diseases can also result in abnormal losses of electrolytes and fluid loss or retention.Older adults have decreased thirst sensation which may affect their oral intake of fluids. Their kidneys have decreased glomerulus’s filtration rate and the Risk for deficient fluid volume r/t age, medication, loss of fluids through abnormal routes(indwelling tubes) and deviation affecting access of fluids . 7 S A E F T Y Lab data and Diagnostic tests: Lab: electrolytes: Na: 142(135-145 mEq/L); K: 4.1 (3.5-5.5 mEq/L); Cl: 107 (96-108 mEq/L); Ca: 9.1 (8.5-11.0 mg/dl) ; Albumin:2.7 ( 3.5-4.9g/dl); Bilirubin: Not recorded. (0.1-1.2 mg/dl); Alk. Phosphatase: Not recorded(30-110 u/l) WBC: 8.2 (norm= 5.0-11.0); culture reports: total cholesterol: Not recorded; LDL: Not recorded (norm= < 130mg/dL); HDL: 48 (norm= 3585mg/dL); triglycerides: Not recorded. (norm= 40150mg/dL); liver function test, etc.- N/A Other significant lab data (include significant data not specified, such as serum levels of drugs, endocrine testes, etc.) N/A Diagnostic tests results (scans, MRI, echo, etc.) – N/A Risks Associated with Diagnostic and Therapeutic Modalities (Some examples include anticipation of common problems identified with: perioperative care, use of restraints, nasogastric tube feeding, blood therapy, total parenteral nutrition, chest tubes, central lines, surgical procedures, etc.)- - Pt at risk for infection due to invasive medical procedures (IV on L arm and Foley catheter.(O). Body temperature patterns x 2 days05/01/2008: 97.6 F 05/02/2008: 97.1 F Recent exposure to infections- IV site on L arm and foley catheter(O) Manifestations of active infection- swelling, redness, pain on old IV site.(O) Immunization: inquire about status including TD, Hepatitis B, Flu, and Pneumococcal-No records of immunization in the charts. number of filtering nephrons. These changes may mean that in the presence of sodium depletion or overload the older adult may not able to maintain homeostasis and the imbalance instead can be worsened. Medications can cause fluid and electrolytes imbalance. Nurses can closely examine laboratory values and knowledge of the clients about side effects and adherence to medication schedule.(P&P,1149). All clients with cathetrization should have 2000-5000 ml oral or IV intake .A high fluid intake produces large amount of urine that flashes the bladder and keps the catheter fre of sediment.( Brunner & Suddarth ,1350) Foley catheter Catheterization of the bladder involves introdusing a rubber or plastic tube through the urethra and into the bladder.The catheter provides continuose flow of urine if client is unable to control micturation or those with obstructions.Bladder catheterization carries risk of UTI,blockege and thrauma to the urethra.When inserting the indwelling catheter closed urinari drainage system is maintained to prevent infections.The bag should be hang on the bed frame not touching the floor below the level of thr bladder.Urine in the bag can become midium for bacteria and infection is likely to develop if thr urine flows back in the bladder.Break in the system can lead to infection .Sites at risk are the site of catheter insertion,the drainage bag ,the tube junctionand the junction between the tube and the bag.(P&P,1350) 8 Medications: major risks associated with side effects/interactionVitamin C 1000mg PO daily Cozaar 50mg PO daily Atenol 50 mg PO daily Gentomyacin 1000 mL IVPB O X I G E N A T I O Alcohol and/or unprescribed drug use: Unable to assess. Discharge Planning: ) 1. Where will the client be going after discharge? Unable to assess. (O) 2. If returning to home, inquire about home environment: adequate space, stairs to climb, cooking facilities, hazards. N/A 3. Ability to manage health problem, knowledge base, motivation, constraints, role of significant others, teaching needs, affordability of medications, supplies and equipment. Unable to assess. (O) 4. Medical follow-up: understands need for, transportation to PMD, clinic, and labs. Need complete assistance. 5. Anticipated need for referral: Social Worker, Visiting Nurse, and other Home Care Services. Unable to assess. (O) Chest pain, describe- Unable to assess. (O) Nails, lips skin, mucus membranes: color/temperature Pt. nail beds, lips and MM are pink and intact. Skin is cold to touch, clammy and diaphoretic. (O) Capillary refill: upper extremities: 4 seconds (O) Pulse - rate, rhythm, quality (rate pattern x 2 days)05/01/2008: 88 05/02/2008: 74 The respiratory system changes throughout the aging process and it is important for nurses to be aware of these changes when assessing patients . Nurses should be aware that the older adult is at risk for aspiration, and infection related to these changes. (Brunner & Suddarth p728) LABS: Impaired gas exchange r/t alveolar-capillary membrane changes AEB abnormal breathing rate, dyspnea and restlessness 9 N O X Y G E N A T I O N O X Y G E N A T I O N Rhythm was Compare apical / radial pulses - Apical: 76 Radial: 77 Peripheral pulses: presence, volume, compare bilaterally (brachial, radial, femoral, political, posterior tibia, dorsal pedals) – All peripheral pulses are present but very weak (O) Homan's sign- Negative (O) Edema: degree and location/measure abdominal girth p.r.nPt has no edema. (O) Distention of neck veins- No distension of neck veins noticed. (O) Blood pressure pattern x 2 days05/01/2008: 163/82 05/02/2008: 172/88 Other factors that may effect the cardiovascular system – immobility, non productive cough(O) Activity tolerance – Client is bed bound. (O) Orthopnea- Client is in semi-fowlers. (O) Shape of chest- Chest symmetrical ,normal(O) Respiration-rate, rhythm, depth, patterns, use of accessory muscles, symmetry of chest movements, rate pattern x 2 days05/01/2008: 18 05/02/2008: 18 There is symmetry of chest movements. (O) Breath sounds: clear, course, crackling, wheezing- clear breath sound s. (O) Location of adventitious sounds – none. (O) Cough: frequent, infrequent, dry, loose, barking, productive, etc.Client was not observed coughing. (O) Sputum: color, tenacity, amount, color- Client had no sputum. (O) Assistive measures: oxygen therapy (kind), tracheotomy, ventilator with E.T. tube, etc. – N/A History of smoking tobacco/marijuana: amount, RBC: cellular component of blood involved in transport of oxygen and carbon dioxide. Hemoglobin: iron-containing protein of RBCsdelivers oxygen to tissues. Decreased level of hemoglobin reflects the presence of fewer than normal RBCs in circulation. As a result, the amount of oxygen delivered to tissues is also diminished. Hematocrit: Is percentage of total blood volume consisting of RBCs. Decreased hematocrit may indicate anemia or acute massive blood loss. PT and APTT: Indicates time taken for clotting to occur. Lengthen PT and PTT may indicate risk for bleeding. Albumin: In the blood, albumin acts as a carrier molecule and helps maintain blood volume and blood pressure. (Brunner & Suddarth p1045, Taber’s p66, p1796) ) Cardiac output in the older adults may be affected by increased arterial wall tension and moderate myocardial hypertrophy due to an increased systoloc blood pressure(P&P,1069). If left ventrical failure is significant the amount of blood ejected from left ventrical drops and decreases cardiac output.Assesment fundinggs may include decreased activity tollerance,breatlessness,dizziness and confusion as a result of tissue hypoxia.(P&P,1078) Lack of movement and exercise places clients at higher risk for reparatory complications. The most common respiratory complications are Ineffective breathing patern r/t anxiety,decreased energy/fatigue as evidence by use of accesory muscle to breath and deapth of breating Decreased cardiac output r/t altered stroke volume AEB clammy skin, altered peripheral pulses prolonged capillary refill and confusion 10 durationUnable to assess. Other factors that may affect the respiratory system – Medication, HTN, Lab: RBC count: 3.23 (norm= 4.0-5.50); Hgb.: 10.1 (norm= 12-15.g/dL); Hct.: 29.3 (norm= 35-47); Platelet: 449 (norm=150-450); ABG's: Ph: 7.45 (7.35-7.45) Pco2: 37.1(35-45) PO2: 80.2 (75-100) HCO3: 24.4(22-26) cardiac enzymes: Unable to assess. (O), ; PT: Not recorded(norm= 11-12.5); APPT: Not recorded. (norm=); INR: 2.9(norm= 3.0-4.5); Guaiac Tests: no record Pulse oximetry results: 96% (O); EKG report: Normal Sinus Rhythm; performed on x-ray/lung scans: None recorded in chart. pulmonary function tests: N/A atelectasis (collapse of alveoli) and hypostatic pneumonia (inflammation of the lung from stasis or pooling of secretions). Both decreases oxygenation, prolong recovery, and add to the client’s discomfort. (P&P 1428)Encourage early ambulation after surgery walking causes client to assume a position that do not restrict expansion of the lungs and stimulates an increased RR .(P&P,1638) General appearance: muscular, wasted, emaciated, obese, well nourished-Client is emaciated. (O) Height and weight patterns of gain or loss- Not able to determine Weight: compare current weight with ideal weight- lb (O) Condition of teeth & gums, ability to chew and swallowClient’s gums were pink and spongy; gag reflex was present. Client had no teeth and no dentures were observed. (O) Usual eating patterns: describe the patient’s usual diet for breakfast, lunch and dinner on a week day and on a weekend day; identify usual number of servings of CHO, protein, milk, vegetables, fruits and fats on a regular day and frequency of intake of fast foods, fried foods, deserts, etc.- observation of lunch only: client is on soft mechanical cardiac diet. (O) N Intake of caffeine, alcohol, sodium, processed foods, fiber- With clients need assistance with feeding it is important to protect client’s safety, independence and dignity. The nurse should asses client ‘s risk for aspiration. Client with more risk for aspiration needs more assistance with feeding. Position client in upright seating position. this client should not use a straw .In addition the rate of feeding is slower and more frequent chewing and swallowing through the meal is need it(P&P,1296-1298) The American Heart association dietary guidelines are intended to reduce risk factors for the development. Dietarian therapy following myocardial infarction includes initial reduction in kilocalories ,soft textured foods and amounts of fats ,sodium, and cholesterol that conform to N U T R I T I O N U Risk for ineffective airway clearance r/t pain and immobility. Feeding self-care deficit r/t weakness, muscoloskeletal impairment, fatigue as evidence by inability to ingest food safely ,inability to chew and complete a meal Nutrition less than body requirements r/t to excessive intake in relation of metabolic need AEB weight less than 10 % under ideal for 11 T R I T I O N Client was observed eating 85% of lunch. (O) Cultural/religious preferences Not able to determine Alterations in eating patterns associated with illness & hospitalization- Client is not able to feed self; assistance is needed. (O) Diet ordered/knowledge of compliance- .- Cardiac pureed diet ,no salt Appetite: assess usual intake and the last 2 days- Client eats 80% of her meals. (O) Lab: total protein:, serum albumin: also consider relationship of Hgb. to nutritional statusGlucose levels – blood:, urine glucose:, acetone in urine: Assistive measures for nutrition (i.e. tube feedings, TPN, etc.)- N/A Are current nutritional needs being met in terms of calories, protein, vitamin, calcium, etc.? Provide objective data to support your decision. If feeding by nasogastric, gastrostomy tubes or TPN: estimate caloric intake for 24 hours # 1 Priority Nursing Diagnosis Ineffective tissue perfusion r/t decreased hemoglobin concentration in blood, decreased Hct, substance abuse aeb confusion, memory impairment and extremity weakness # 2 Priority Nursing Diagnosis Impaired gas exchange r/t alveolar-capillary membrane changes AEB tachycardia, decreased carbon dioxide AHA recommendations. Magnesium and folic acid appeared to be important for primary prevention . Nursing intervention for hypertension ,coronary artery disease and CHF include weight reduction and limiting fat and salt intake.(P&P,250) Caloric intake to the point of obesity overloads the cells of the body with lipids .By requiring more energy to maintain the extra tissue obesity place a strain on the body’s cardiovascular system(Brunner & Suddarth p101) Outcomes - In 48 hrs, client will demonstrate adequate tissue perfusion aeb increased strength in extremities, able to remember recent events, loss of confusion Outcomes -Pt lung fields maintain clear and remain free of signs of respiratory distress by the end of hospital stay. height and frame Implementation 1)Assess skin color and temperature, vital signs, capillary refill and mental status. 2) Teach the client to recognize signs and symptoms of ineffective tissue perfusion such as change in skin color and temperature. 3) Administer 2 L oxygen nasal cannula Implementation 1. Monitor respiratory rate, depth, pattern and breathe sounds q2h. 12 -Pt will maintain adequate oxygenation and gas levels within normal parameters during hospital stay. -Pt will have adequate peripheral perfusion during hospital stay. 2. Administer supplemental O2. 3. Teach client to cough and deep breathing exercise q2 hours.