Glutaraldehyde Usage Guidelines
advertisement
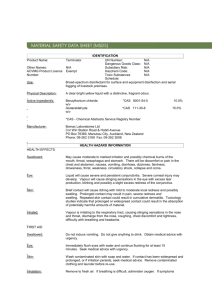
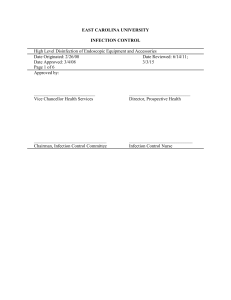
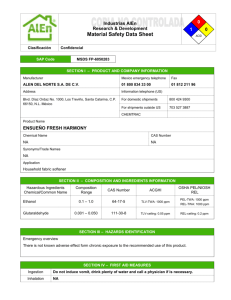
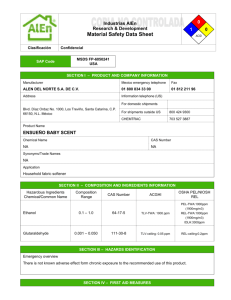
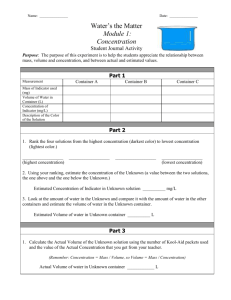
EAST CAROLINA UNIVERSITY INFECTION CONTROL POLICY Glutaraldehyde Usage Guidelines Date Originated: 03-21-07 Date Approved: 03/21/07 Page 1 of 10 Approved by: Date Reviewed: 9/21/10 _____________________________ Chairman, Infection Control Committee ____________________________ Infection Control Nurse 1 Purpose: To prevent the transmission of infection to patients or employees by ensuring proper use of glutaraldehyde for high level disinfection/sterilization. Personnel responsible for the cleaning and disinfection of equipment and instruments must be familiar with the guidelines in this policy. I. Definitions A. Cleaning- the physical removal of soil and organic material from objects, usually done with water, detergents or enzymatic products. Meticulous cleaning must precede disinfection and sterilization procedures, since materials that remain on the surfaces of instruments interfere with the effectiveness of these processes. B. Low Level Disinfection- a process that can kill most bacteria, some viruses and some fungi, but it cannot be relied on to kill resistant organisms such as tubercle bacilli or bacterial spores. C. High Level Disinfection- the destruction of all microorganisms with the exception of high levels of bacterial spores. High level disinfectant/sterilant refers to a chemical germicide that has been cleared by the FDA as capable of destroying all microorganisms, including all bacterial spores. When used at a shorter exposure time it destroys all viruses, vegetative bacteria, fungi, mycobacterium and some, but not all, bacterial spores. Several factors influence the effectiveness of disinfection, including (1) the presence of organic matter, (2) proper choice of disinfectant for the object to be disinfected and (3) the concentration and exposure time of the disinfectant solution. D. Material Safety Data Sheet (MSDS) - a descriptive sheet that accompanies a chemical or chemical mixture, providing the identity of the material; physical hazards, such as flammability; acute and chronic health hazards associated with contact with or exposure to the compound. E. Minimum effective concentration (MEC) - the lowest concentration of active ingredient necessary to meet the label claim of a reusable high-level disinfectant/sterilant. F. Sterilant- a chemical germicide that has been cleared by the FDA as capable of destroying all microorganisms, including all bacterial spores. G. Sterilization- a process that results in the complete elimination or destruction of all forms of microbial life. The Spaulding Classification identifies sterilization as the standard for medical devices that enter the vascular system or sterile tissue. H. The Spaulding Classification System- divides medical devices into categories based on the risk of infection involved with their use. Used by the FDA, CDC and profession medical organizations to aid in determining the degree of disinfection or sterilization required for medical devices 1. Critical: A device that enters normally sterile tissue or the vascular system. These devices should be sterilized. 2 2. Semi critical: A device that comes into contact with intact mucous membranes and does not ordinarily penetrate sterile tissue. These devices should receive at least high-level disinfection. 3. Non critical: Devices that do not ordinarily touch the patient or touch only intact skin. These devices may be cleaned by low level disinfection. I. Threshold limit value ceiling (TLV-C) - the airborne concentration of a substance that should not be exceeded during any part of the work experience. J. Use-Life- a statement by the manufacturer indicating the maximum number of days a reusable high-level disinfectant/sterilant might be effective. II. Using Glutaraldehyde for high-level disinfection A. Clean instruments 1. Contaminated instruments must be thoroughly cleaned prior to disinfection or sterilization since residual organic matter will decrease the effectiveness of the glutaraldehyde solution. 2. To remove debris, thoroughly clean all instrument surfaces and lumens of hollow instruments with a mild protein dissolving detergent. 3. Following cleaning, rinse instrument surfaces and lumens with large amounts of fresh water to remove residual detergent. 4. Remove excess moisture or air dry prior to disinfecting or sterilizing. This will help prevent water from diluting the glutaraldehyde. B. Personal protective equipment (PPE) 1. Don PPE, including disposable gloves, eye protection, face mask and liquid proof gown. If working with glutaraldehyde for less than 15 minutes, latex gloves may be worn. Changing latex gloves every 15 minutes or double gloving provides up to a four-fold increase in permeation time compared with single latex gloves. 2. One hundred percent nitrile or 100% butyl rubber gloves are recommended for the best protection from glutaraldehyde. 3. Neoprene and polyvinyl chloride (PVC) gloves are not recommended as these materials absorb and retain glutaraldehyde. C. Activate solution 1. Add the entire contents of the activator vial to the solution in the container. Shake well. 3 2. Test the product for MEC. Use 14 day test strip for 14day solution and 28 day test strip for 28 day solution. 3. Record the date of activation and expiration date on the solution container, in a log book, and on any secondary containers. 4. Do not use activated solution beyond stated 14 or 28 day reuse life. D. Storage 1. Store in original or properly labeled container with date of expiration written on label. 2. Keep container tightly closed and store at room temperature. E. Disinfecting 1. Immerse clean instruments completely in the solution. 2. High-level disinfection is achieved with a soaking time of at least 20 minutes at 20˚C (room temperature). 3. Critical instruments that enter sterile tissue or the vascular system should be autoclaved. If instruments are heat sensitive and can not be autoclaved, cold sterilization with glutaraldehyde can be achieved in approximately 10 hours at room temperature. F. Rinsing and drying 1. Remove instruments from solution and rinse thoroughly with sterile water or potable (drinking) tap water. The quality of the rinse water used is dependant on the intended use of the instrument. 2. For devices that have been sterilized: Remove instruments from solution using sterile technique and rinse thoroughly with sterile water. 3. Equipment should be used immediately or stored in a manner to minimize recontamination. G. Testing 1. It is important to note that the solution may expire prior to the reuse date stated on the label. Do not rely solely on days in use. To determine if the MEC is still present, the solution must be tested with the product specific test strip. 4 2. Test the solution for MEC on each day of use. If the solution is used daily it must be checked daily. Use 14 day test strip for 14day solution and 28 day test strip for 28 day solution. a. Completely submerge indicated pad of the strip into solution. b. Hold for 1 second, and then remove. Do not shake strip. c. Remove excess solution by standing the strip upright on a paper towel. d. Read results at 90 seconds. Do not read past 90 seconds. Pad will be completely red to indicate effective solution. If any yellow remains on the pad apart from the top line, the solution is ineffective and must be discarded. e. Tightly recap test strip bottle after each use. f. Test strip bottle should be dated when opened. Discard any unused test strips 90 days after bottle is opened. 3. Discard the solution according to manufacturer’s time frame, (i.e., 14 days, 28 days or whenever the chemical indicator indicates that the concentration is less than the MEC). 4. The use-life of a reusable high-level disinfectant/sterilant is related to several factors including, but not limited to: dilution, time/temperature, and number of uses. It is essential that the level of active ingredient be at or above that required to kill and/or inactivate the desired microorganisms. 5. The MEC may not be used to extend the use-life claim of the product. 6. Keep a log of the test results. The log should include the date, test results and name of individual performing the test. (Appendix A) H. Disposal 1. In compliance with the United States Environmental Protection Agency (EPA) requirements, glutaraldehyde solutions may be disposed of as an ordinary domestic waste, rather than a hazardous waste. 2. Discard the solution down the sink drain and flush well with a large quantity of water (1quart of glutaraldehyde to 2 gallons of water. 3. Rinse container well with water and discard in regular trash. Do not reuse empty container. 5 I. Safety 1. Glutaraldehyde is an irritant and some individuals develop acute sensitivities such as itching of the skin with slight redness, to redness and swelling or yellowing of the skin with prolonged exposure, or irritation to eyes and nasal membranes, headache, coughing, sneezing, and asthmalike symptoms. 2. Glutaraldehyde can be absorbed by inhalation, ingestion and through the skin. It has a detectable odor 0.04 parts per million volume (ppmv) and is irritating to skin and mucous membranes at 0.3 ppmv. Vapors are released whenever solutions are disturbed. Mixing, adding and removing equipment, or disposing of solution may release vapors. 3. The National Institute for Occupational Safety and Health (NIOSH) has established a recommended exposure limit of 0.2 ppm; therefore, adequate ventilation must be provided in areas where glutaraldehyde is in use. Adequate ventilation as described by the Association for the Advancement of Medical Instrumentation (AAMI) includes the following: Room large enough to ensure adequate dilution of vapors 10 air changes per hour to allow volume flow rate of air moving through the room to be at least 1.0 to 2.0 cubic feet per minute per square foot of floor area. Exhaust located at the source of the discharge of vapors (pulling vapors away from the user’s breathing zone). This can be done by placing the exhaust fan at foot level or on a countertop and venting the vapors to the outside. Fresh air return entering at ceiling level across the room from the exhaust vents. Elimination of cross-draft effects. Care should be taken to ensure that the discharge of the vapors is sufficiently removed from windows, outside air intakes or other such openings to prevent reentry of the discharged air. Air must not be recirculated. In areas where local exhaust systems are not in place, use ductless fume ventilation devices that contain filters to absorb glutaraldehyde vapors from the air. These hoods should achieve at least 100ft. per min. with the airflow directed toward the back of the hood. 6 General room exhaust ventilation is adequate for bench top use of closed, single container of glutaraldehyde. Larger amounts may require additional measures. 4. Notify Employee Health and Safety (EH&S) at 328-6166 of any area using glutaraldehyde. EH&S will perform exposure monitoring to check airborne concentration. 5. Have the Material Safety Data Sheet readily accessible. J. Spill Cleanup 1. Staff should be trained in cleanup procedure of small spill (those that can be cleaned up with paper towels). The following procedure is recommended: Limit access to the spill area Put on appropriate PPE (nitrile gloves, eye protection, gown or full buttoned lab coat, closed toe shoes) Use absorbent material to soak up all the liquid Seal absorbent material and any contaminated clothing in vapor tight plastic bag and place in biohazard container Wash any contaminated surfaces with soap and water. 2. For larger spills that can not be managed by staff, evacuate the area , and call EH&S at 328-6166 3. See EH&S Laboratory Safety Plan for Glutaraldehyde Use (Appendix B) for a summary of information regarding special handling and storage requirements, spill and accident procedures, and hazardous waste disposal. Post the Safety Plan in the area of glutaraldehyde use for quick reference. 4. Persons responsible for high-level disinfection/sterilization must receive device specific training and competency training initially and annually thereafter. 5. Additional information and online training is available at the EH&S website at http://www.ecu.edu/oehs/BSOM/Cidextrainpoint.ppt 7 Appendix A Minimum Effective Concentration Log for: 2.4% Glutaraldehyde Container/Reprocessor: ________________ Date # uses Pass/Fail 8 Initials Comment (solution changed) Appendix B Laboratory Safety Plan for Glutaraldehyde (Cidex) Use Process Hazardous Chemical/Chemical Class Hazardous Equipment Potential Hazards Personal Protective Equipment Engineering and Ventilation Controls Special Use Procedures Special Handling And Storage Requirements Spill and Accident Procedures Hazardous Waste Disposal Decontamination Procedures Animal Care Precautions Chemical Procurement Cidex use for sterilization and high-level disinfection of equipment Glutaraldehyde: poison, irritant, sensitizer Not applicable Absorption through intact skin; ingestion by cross contamination; inhalation of vapors; injection through the skin by a puncture wound; glutaraldehyde will cause skin to become sensitized. Nitrile rubber or butyl rubber gloves; splash proof safety goggles; full buttoned front or back closing lab coat; closed toe shoes General room exhaust ventilation adequate for bench top use of closed, single container of CIDEX Avoid splashes; point open containers containing solution away from face to minimize inhalation. Store in original or properly labeled secondary container; date of expiration should be recorded on container; container should be kept tightly closed and stored at room temperature. Wear suitable personal protective equipment (Nitrile/butyl rubber gloves, splash proof safety goggles, full buttoned front or back closing lab coat, closed toe shoes); use absorbent material to pick up all liquid; seal absorbent paper and any contaminated clothing in vapor tight plastic bag and place in biohazard container; wash any contaminated surfaces with soap and water. Discard solution down sink drain; flush well with a large quantity of water (for 1 quart of CIDEX, use 2 gallons of water); rinse container well with water and discard in regular trash (DO NOT reuse empty container); record all drain disposals on drain disposal log. Not applicable. Not applicable. Purchase no more than required amount for 6-month supply. Use CIDEX test strips to determine efficacy before use; always check expiration dates to ensure effectiveness. 9 10