Side Effects - My Surgery Website
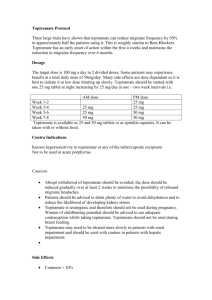
advertisement

PROPHYLAXIS FOR MIGRAINE Guidance Prophylaxis is indicated in patients with frequent migraine or if migraine causes significant disability These medications should be initiated at low dose to minimise side effects and the dose should be gradually titrated upwards depending on patient response and tolerability. A 3-6 month trial is required to determine efficacy. As a general rule only one drug should be used at a time but combination therapy can be useful in patients with difficult to control migraine. A useful combination is nortriptyline and topiramate. Choice may depend on co-morbid conditions and contra-indications First choice for adults is usually ß blockers or tricyclic Second choice for adults is an anti epileptic (caution in women using COP). Risk of teratogenicity should be discussed with the patient First choice for children (<16 years) is Pizotifen Most prophylactic agents won’t work in the presence of medication overuse. Overused medications should be withdrawn. A patient leaflet with information about these drugs is available to download from the NHSG intranet. Adult Patient Prophylaxis Flow Chart Migraine prophylaxis indicated and medication over use headache excluded Propranolol or TCA (Nortriptyline or Amitriptyline) No response to either after 3 month trial at maximum tolerated dose Review contraception Good response, consider stopping after 6-12 months Consider antiepileptic Topiramate Gabapentin Sodium valproate No response to 3 anti epileptics after 3 month trial at maximum tolerated dose Consider referral to headache clinic Prophylactic drugs Beta-blockers o Tricyclic anti– depressants o First choice is propranolol starting at 10mg three times a day. The dose should be increased every 2 weeks aiming for a target daily dose of between 80 -240 mg. There is some evidence that splitting the dose in to 3 divided doses is more effective than using slow release tablets. If propranolol is not tolerated there is some evidence for atenolol 25-100 mg daily or metoprolol 100-200 mg daily. Propranolol is safe to use in pregnancy up to a dose of 60 mg daily. Higher doses should be discussed with an obstetrician. Nortriptyline or amitriptyline 10-150 mg at night. The starting dose is 10mg at night which should be increased every 1-2 weeks aiming for a dose that controls the headache whilst limiting side effects. Some patients require doses approaching 100mg. There is empirical evidence that Nortriptyline is better tolerated than amitriptyline. Amitriptyline is safe to use in pregnancy up to a dose of 50mg. Higher doses should be discussed with an obstetrician. Anti - epileptics These can all be initiated in primary care without specialist advice. Antiepileptics for migraine are contra-indicated in pregnancy, They may interfere with contraception and appropriate contraception should be discussed with women of child bearing age. Topiramate 25mg to 100 mg daily in 2 divided doses. The starting dose is 25 mg daily and built up slowly every 1- 2 weeks. All side effects are dose related. Please see the NHSG topiramate protocol below for more information. Some patients get a fantastic response to topiramate virtually being headache free. Others can’t tolerate side effects. Sometimes it takes 34 months to be effective so it is worth persevering even if there is no initial headache response. . Gabapentin 1200- 2400 mg daily in divided doses. Starting dose is 100 mg three times a day. This can be increased by 100mg every 3-5 days depending on tolerability. Sodium valproate 200-600 mg twice a day. The starting dose is 200 mg twice a day titrated up every 2-4 weeks aiming for a dose of 600 mg twice a day. Other agents with some evidence. 5HT2 antagonists pizotifen 500 mcg – 4.5mg daily (best taken at night time)evidence is poor and often large doses above 3mg are needed in adults which limits its use due to side effects of sedation and weight gain. Usual drug of first choice in children ARB Candesartan 2-16 mg daily.There is some evidence for its use in episodic migraine. It is used as a first choice agent in some Northern European countries due to its high tolerability. It should be reserved for patients failing or not tolerating β blockers, tricyclics or anti epileptics or in patients in whom these medications are contra-indicated. SNRI Venlafaxine 75-150 mg daily has a SIGN grade B recommendation as an effective alternative to tricyclic antidepressants for the prophylaxis of migraine. Topiramate Protocol Three large trials have shown that topiramate can reduce migraine frequency by 50% in approximately half the patients using it. This is roughly similar to Beta-Blockers. Topiramate has an early onset of action within the first 4 weeks and maintains the reduction in migraine frequency over 6 months. Dosage The target dose is 100 mg a day in 2 divided doses. Some patients may experience benefit at a total daily dose of 50mg/day. Many side effects are dose dependant so it is best to initiate it at low dose titrating up slowly. Topiramate should be started with one 25 mg tablet at night increasing by 25 mg/day at one – two week intervals i.e. AM dose PM dose Week 1-2 25 mg Week 3-4 25 mg 25 mg Week 5-6 25 mg 50 mg Week 7-8 50 mg 50 mg Topiramate is available as 25 and 50 mg tablets or as sprinkle capsules. It can be taken with or without food. Contra Indications Known hypersensitivity to topiramate or any of the tablet/capsule excipients Not to be used in acute porphyrias. Cautions Abrupt withdrawal of topiramate should be avoided, the dose should be reduced gradually over at least 2 weeks to minimise the possibility of rebound migraine headaches. Patients should be advised to drink plenty of water to avoid dehydration and to reduce the likelihood of developing kidney stones Topiramate is teratogenic and therefore should not be used during pregnancy. Women of childbearing potential should be advised to use adequate contraception whilst taking topiramate. Topiramate should not be used during breast feeding. Topiramate may need to be titrated more slowly in patients with renal impairment and should be used with caution in patients with hepatic impairment. Side Effects Common > 10% o Paraesthesia in about 50% o Anorexia, nausea o Weight loss o Fatigue o URTI o Diarrhoea Less common < 10% o Cognitive effects such as memory, language and somnolence o Depression and mood alteration Rare < 1 % o Acute myopia secondary to angle closure glaucoma o Choroidal effusions resulting in anterior displacement of the lens and iris Monitoring Response to therapy o Topiramate should be administered for a minimum of 12 weeks o If effective continue for 6 months and then withdraw to establish continued need. (migraine prophylaxis should rarely be used uninterrupted for more than 12 months) o If not effective at adequate dosage or intolerable side-effects, treatment should be withdrawn and alternative therapy considered. Cognitive effects rarely settle so treatment should be withdrawn early if there are significant problems. Treatment Safety o Patients with new onset visual symptoms or signs should have their intra ocular pressure measured urgently. If it is raised they should be referred to the ophthalmology clinic immediately and the topiramate stopped as rapidly as feasible o Patients on long term topiramate should be weighed every 8 weeks and discontinuation of treatment should be considered if weight loss is greater than 10%. o Patients should be monitored for signs of depression and advised to seek medical help immediately if they have suicidal thoughts.