Supplementary Table 1 | IBD medication monitoring for elderly IBD
advertisement

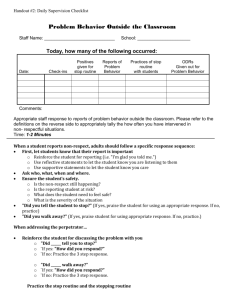
Supplementary Table 1 | IBD medication monitoring for elderly IBD patients 1–7 IBD medication Potential adverse events Monitoring strategy 5-ASAs Nephrotoxicity Routine monitoring of creatinine Potential use with caution for patients with underlying severe renal disease Diarrhea/exacerbation of Paradoxical hypersensitivity diarrhea can occur in colitis symptoms mesalamine treated patients If persistent symptoms, trial of medication discontinuation or switching agents (particularly with sulfasalazine) Corticosteroids Serious infection Construct steroid-sparing exit strategy with first steroid taper Avoid repeated steroid tapers No maintenance steroids Vaccinations (influenza, pneumonia, zoster if appropriate) Osteopenia/osteoporosis Calcium + Vitamin D supplementation (recommended 1000-1200mg of calcium daily, 400-800 IU of Vitamin D daily) Consider 25-OH Vitamin D testing and repletion if low Regular weight-bearing exercise Bone densitometry – recommended for patients >50 years, > 3 months of steroid exposure Avascular necrosis If persistent joint pain of hips, knees, shoulders, consider imaging with magnetic resonance imaging (MRI) or bone scan Glaucoma/cataracts Annual ophthalmologic exams Steroid-induced Routine blood glucose monitoring, particularly if prediabetes/hyperglycemia existing history of diabetes Maintain tight glycemic control with oral hypoglycemic ± insulin Registered dietitian consultation Myopathy Monitor for proximal muscle weakness Routine physical activity, consider physical therapy and occupational therapy consultation if prolonged steroid use Hypertension Routine blood pressure checks, consult with primary care physician for adjustments to medical therapy if persistently elevated Thiopurines Serious infection Vaccinations Hold immunosuppression if severe infection requiring hospitalization Myelosuppression Thiopurine methyltransferase (TPMT) testing prior to thiopurine initiation Review medication list for potential interactions (e.g. allopurinol) Routine complete blood count (CBC) monitoring every 1-3 months Thiopurine metabolite testing Hepatotoxicity TPMT testing Routine liver function monitoring every 1-3 months Thiopurine metabolite testing – consider dose-adjusted IMM plus allopurinol therapy Skin cancer (nonmelanoma) Lymphoma Ciprofloxacin Achilles tendinitis/tendon rupture Clostridium difficile Anti-TNF agents Serious infection Immunogenicity, loss of response Anti-TNF induced lupus Psoriasis Congestive heart failure (CHF) Routine dermatologic evaluations Appropriate sun protection, including scalp and eye protection No screening mechanism, but monitor for “B”symptoms: fevers, night sweats, unintentional weight loss; also, unexplained fatigue and weakness Routine office visits, full physical exam to check for peripheral adenopathy Routine CBC monitoring for persistent cytopenias Stop therapy if new diagnosis, consult with oncology first prior to starting therapy if prior history of lymphoma Avoid concomitant use - Increased risk in elderly on concomitant steroids Check for pain with palpation along Achilles tendon, particularly with plantar flexion MRI or ultrasound if high clinical suspicion Increased risk of C. difficile infection among the elderly on antibiotics Low threshold for testing if increased diarrheal symptoms (regardless of antibiotic exposure) Initial treatment with metronidazole for mild first episode, but low threshold to escalate to vancomycin if non-response Vancomycin for moderate to severe disease (with or without IV metronidazole) Vaccinations If severe symptoms, consider evaluation for atypical or opportunistic infections such as histoplasmosis, coccidiomycosis or Pneumocystis jiroveci Tuberculosis screening prior to anti-TNF initiation (indeterminate result may occur while on chronic steroids) Hepatitis B testing (surface antigen and antibody) Anti-TNF level and antibody testing Dose adjustment or switch depending on presence or absence of antibodies Smoking cessation counseling Monitor for swollen, painful, stiff joints Testing for drug-induced lupus: anti-nuclear antibodies (ANA), double-stranded DNA antibody (dsDNA), antihistone antibodies Rheumatology consultation Discontinue or switch anti-TNF agents Dermatology consultation if progressive skin lesions present Limited affected area or mild symptoms trial of topical therapy first If extensive affected area or severe psoriasis, switch or discontinued anti-TNF Possible role for ustekinumab Contraindicated for Class III or IV heart failure Pre-treatment consultation with cardiology for patients with class I or II heart failure or pre-disposing Demyelinating disorders Skin cancers (melanoma) Malignancy conditions to CHF Contraindicated for patients with central demyelinating conditions Consult with neurologist for patients with possible history of demyelinating disorders Neurology referral if symptoms if ataxia, paresthesias, etc. with no other explainable cause Routine dermatologic evaluations Appropriate sun protection, including scalp and eye protection Continue routine cancer screening programs – e.g. breast, colon and prostate (if appropriate) Consultation with oncology prior to initiation if current, recent or remote history if malignancy 1. Ding, T. et al. BSR and BHPR rheumatoid arthritis guidelines on safety of anti-TNF therapies. Rheumatology 49, 2217–2219 (2010). 2. Lichtenstein, G. R., Hanauer, S. B. & Sandborn, W. J. Management of Crohn's disease in adults. Am. J. Gastroenterol. 104, 465–83 (2009). 3. Widdifield, J. et al. Serious infections in a population-based cohort of 86,039 seniors with rheumatoid arthritis. Arthritis Care Res. 65, 353–361 (2013). 4. Zhang, J. et al. Association between vaccination for herpes zoster and risk of herpes zoster infection among older patients with selected immune-mediated diseases. JAMA 308, 43– 49 (2012). 5. Moscandrew, M., Mahadevan, U. & Kane, S. General health maintenance in IBD. Inflamm. Bowel Dis. 15, 1399–1409 (2009). 6. Kappelman, M. D. et al. Direct health care costs of Crohn's disease and ulcerative colitis in US children and adults. Gastroenterology 135, 1907–1913 (2008). 7. Wolff, J. L., Starfield, B. & Anderson, G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch. Intern. Med. 162, 2269–2276 (2002).