Supplementary Methods - Word file (60 KB )
advertisement

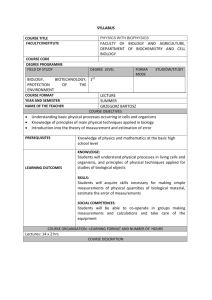
Nature 2005-04-04381B-Z Supplementary Materials: Methods for Enhanced Bacterial Clearance and Sepsis Resistance in Caspase-12 Deficient Mice Maya Saleh1, 2, John C. Mathison3, Melissa K. Wolinski1, Steve J. Bensinger1, Patrick Fitzgerald1, Nathalie Droin1, Richard J. Ulevitch3, Douglas R. Green1, ¶ and Donald W. Nicholson4, ¶. 1 Department of Cellular Immunology, La Jolla Institute for Allergy and Immunology, San Diego, CA92121, USA 2 Present address: Department of Medicine, McGill University, Montreal, Canada H3A 1A1 3 Department of Immunology, The Scripps Research Institute, San Diego, CA92037, USA 4 Merck Research Laboratories, Rahway, NJ 07065-0900, USA ¶ contributed equally to this work and share senior authorship 1 Methods Materials Brefeldin A, thapsigargin, tunicamycin, A23187 and LPS (E. coli 0111:B4, cat # L-2630) were purchased from Sigma. Pam3CSK4 (Synthetic lipoprotein) was from InvivoGen, polyI:C (double stranded) was from Amersham (Piscataway cat #27-4729-01), LPS Re595 (Salmonella Minnesot) was purified by phenol chloroform petroleum ether extraction from washed lyophilized bacteria as described in (1), Resiquimod R848 was from Novartis, CpG was from Research Genetics (now part of Invitrogen) and muramyl dipeptide MDP (Ac-muramylAla-D-glu-NH2) was from Bachem Americas (www.bachem.com, cat # G1055). Brain heart infusion agar plates with 5 % sheep blood were from Hardy Diagnostics (cat # W185). Brain heart infusion agar (modified powder) was from Beckton Dickinson (cat # 299069). Rabbit polyclonal antibodies against bacterial -galactosidase were from Abcam (cat # ab616). Rat monoclonal antibodies against mouse caspase-12 and caspase-11 were from Sigma. Generation of Caspase-12 knockout mice Caspase-12 knockout mice were generated by Deltagen (San Carlos, CA) under a consortium agreement involving Merck & Co. A targeting construct was engineered to disrupt the caspase-12 gene in ES cells by homologous recombination. A segment of exon 2 was targeted for replacement by a cassette consisting of the -galactosidase (-gal) gene and the neomycin (neo) resistance gene, shifting caspase-12 downstream amino acid sequence out of the open 2 reading frame. Positive clones were selected in 350 g/ml G418 (Gibco) and 0.2 nM of FIAU (Moravek Biochemicals) and confirmed both by Southern blot and PCR. ES cells were injected into C57BL/6J blastocysts and resulting male chimeras were bread to C57BL/6J females in order to obtain caspase-12+/- mice, which were then intercrossed to obtain caspase-12-/- mice on a mixed C57BL/6J129/SvImJ genetic background. The caspase-12-/- mice used in this study were backcrossed to homogeneity to a C57BL/6J background. Preparation of mouse embryonic fibroblasts Pregnant females were euthanized at day 14 of gestation. Embryos were decapitated and eviscerated then digested with trypsin for 10 min at 37 C rotating. Fibroblasts were filtered through 100 m filters, cultured in DMEM supplemented with 10% fetal bovine serum and antibiotics, propagated for 2 passages and then frozen. Preparation of mouse intestinal epithelial cells (IECs) Small intestines were excised, perfused with PBS using a 22-gauge needle, filleted by cutting down the length of the organ to expose the lumen, then cut into smaller pieces and placed into 30 ml RPMI with 10% FBS and antibiotics. DTT (1 l/ml) was added and the tubes were shook at 200-215 rpm for 30 min at 37 °C. Single cell suspension was then obtained by filtering through 100 m syringe filters. Cells were spun at 1500 rpm for 5 min at 4 °C and resuspended in a 30% Percoll solution diluted in RPMI, transferred into 15 ml conical tubes and spun at 1700 rpm for 20 min at 4 °C to separate the layer containing the 3 IECs. The top layer was collected, placed in RPMI, spun again at 1500 rpm for 5 min at 4 °C and used for culture. Cell culture and induction of cell death Mouse embryonic fibroblasts were treated with either PBS only, brefeldin A, tunicamycin, thapsigargin or A23187 at increasing concentrations (as indicated in the figure legend) for 24 hrs at 37 C. Cell death was measured by quantification of propidium iodide stained cells using flow cytometry. Induction of sepsis using the colon ascendens stent peritonitis procedure Mice (age 6-12) weeks were anesthetized using isofluorane. A midline 1.5 cm incision was made in the lower abdomen and the cecum was exposed. Cecal content was gently pressed into the colon, and an anchoring stitch of 7.0 monofilament nylon was placed 1 cm distal to the iliocecal valve in the wall of the colon. A #11 surgical blade was used to make a 1 mm longitudinal cut in the colon immediately distal to the anchor stitch, and an introducer is used to place a 14G stent in the colon wall. The loose ends of the anchoring suture were brought around the stent and tied, and a second anchor stitch was placed 180 degrees to the first. A cotton-tipped applicator was used to press cecal content through the stent, leaving 1-2 mm of content beyond the opening of the stent, and the applicators were used to reposition the cecum and colon back into the abdomen. Saline containing 1 g buprenorphine (0.3 ml total volume) was added through the incision, and the muscle layer was closed using a running 5.0 monofilament nylon suture followed by closure of the skin layer with three 7.5 mm suture clips. Following surgery, the mice were kept under a warming lamp 5 minutes before 4 being returned to the cage. Monitoring was performed five times per day during the first 48 hrs after surgery, observing activity, alertness and temperature. Animals developing severe sepsis become hypothermic within hrs after surgery. Surface temperature measured using an infrared thermometer (Raytek MiniTempFS, Santa Cruz, CA) positioned over the shaved surgical site was a reliable indicator of long-term survival, as animals remaining below 30oC have not been observed to survive beyond 24-48 hrs after the CASP procedure. Animals that are determined to be moribund (temperature <23 °C, showing minimal response to challenge and diminished righting reflex) were euthanized, allowing for collection of blood and for post mortem analysis. Long-term survivors were followed until day 8 after surgery when they were euthanized for final sampling and autopsy. Listeria monocytogenes challenge For in vivo infections, Listeria monocytogenes (LM) strain DP-L4056 (a generous gift from Dr. D. Portnoy, University of California, Berkeley) was grown to mid-logarithmic phase, measured by optical density (A600), in brainheart infusion (BHI) broth. Cells were then pelleted, washed, resuspended and diluted to the appropriate concentration in PBS. Approximately 5 x 104 CFU were injected into the lateral tail vein in a volume of 200 l. Injected bacteria numbers were more accurately determined by spreading bacterial samples on BHI agar plates. 5 Determination of bacterial content in sepsis and Listeria models In the sepsis model, 100 l peripheral blood samples were collected by orbital puncture 12 hrs following CASP. The blood volume was brought up to 0.5 ml with distilled water and serial dilutions of that (1:2, 1:100, 1:1000) were prepared in distilled water and were plated on brain heart infusion blood agar plates. Following a 24-hour incubation of the plates, bacterial colonies were counted and the number of colony forming units (CFU) per ml blood was calculated. In the Listeria model, peripheral blood was collected and analyzed as above on days 1, 2, 3 and 4 following Listeria injection. At the same time points, spleens and livers were also collected and were homogenized in a 10 ml volume of a 0.2 % NP-40 solution. Serial dilutions (1:10, 1:100, 1:1000) were plated on brain heart infusion agar and bacterial counts were assessed as above. Immunohistochemistry Tissues were obtained, fixed in 1% formaldehyde in PBS, and sent to Pacific Pathology (San Diego, CA.) for embedding and sectioning. For immunohistochemical staining, slides were de-waxed at room temperature in Slide Brite solution (Sasco) for 3 changes 5 min each and rehydrated in 3 changes of ethanol (100%, 95%, 70%) 5 min each followed by water. Antigen retrieval was performed using an antigen retrieval kit from Abcam (cat #ab8212) for 20 minute at room temperature in a humidified chamber followed by 2 washes each for 5 min in TBS pH 7.5. Protein blocking of the tissues was done using the ABC kit from Abcam (cat # ab8628) for 5 min at room temperature, followed by 2 washes for 5 min each in TBS pH 7.5. Tissues were then 6 incubated in TBS pH 7.5/ 1% BSA with a primary rabbit polyclonal anti-ßgalactosidase antibodies (1:100, Abcam cat # ab616) for 60 minutes at room temperature or overnight at 4˚C followed by 2 washes 5 min each in TBS pH 7.5. Biotin-labeled anti-rabbit secondary antibodies were then incubated for 1 hr at room temperature and avidin reagent with alkaline phosphatase Vega Red substrate-chromogen mixture from Abcam (cat # ab9099) were utilized. Dehydration and coverslipping in Clarion mounting media (Abcam cat # ab8193) followed. Splenocytes culture and treatments Spleens were extracted in ice cold RPMI with 10 % fetal bovine serum and antibiotics. Splenocytes were dissociated by gently grinding between the frosted sides of two microscope slides. Cells were pelleted and red blood cells were lysed in erythrocyte lysis buffer (Sigma cat # R7757) for 2 min at room temperature. White blood cells were pelleted and resuspended in RPMI and plated at a density of 105 cells per well in 96-well plates. Cells were treated for 24 hrs with PAMcsk4 (100 ng/ml, TLR2), polyI:C (4 g/ml, TLR3), LPS Re595 (S. Minnesot) (100 ng/ml, TLR4), Resiquimod R848 (1:500, TLR7), CpG (0.2 M, TLR9), muramyl dipeptide MDP (10 M or 100 M) with or without cycloheximide CHX (0.5 g/ml). Cells were then treated with 5 mM ATP in fresh media for 20 minutes, washed and further cultured in fresh media for 3 hrs. Bead-based multiplex immunoassays A 10-plex (10 mouse cytokines: Il-1, Il-2, IL-4, IL-5, Il-6, Il-10, IL-12p70, IFN, TNF and GM-CSF) immunoassay kit from LINCOplex was used 7 according to the manufacture’s instructions. Data was obtained and analyzed using the Bio-Plex system from Biorad. Anti-IFN receptor treatment Anti-IFN antibodies and the isotype control antibodies were purchased from PharMingen (cat. # 557530 and 553969, respectively). The antibodies were administered via i.p. injection at a dose of 250 g/mouse one hour prior to induction of sepsis by CASP. Bone marrow chimeras On day 1, recipient mice were irradiated twice with 550 rads of ionizing radiation with a resting time of 6 hrs between the two irradiation treatments, then rested O/N before injection of donor bone marrow cells. On day 2, bone marrow cells were collected in PBS from donor mice femurs using 22-gauge needle to perfuse the femurs. Cells were resuspended by pipeting and passed through 100 m filters to obtain single cell suspension. Cells were counted then incubated for 20 minutes at room temperature with anti-Thy 1.2 antibodies (Miltenyi Biotec, cat # 130-049-101) then passed over a magnetic LS separation column (Miltenyi Biotec, cat # 130-042-401) to deplete T cells. Cells were recounted and 1 million cells were injected in tail vein of recipient mice using a 27-gauge needle. Mice were left for 8 weeks to reconstitute their bone marrow before induction of sepsis. 5 weeks following bone marrow injection, peripheral blood counts were performed and no significant difference was observed among groups. 8 weeks after injection, reconstitution was confirmed by genotyping of peripheral blood cells. 8 THP-1 cell transfection and differentiation THP-1 cells were transfected by electroporation as follows: 2 x 107 cells were resuspended in 300 l complete RPMI media containing 20 mM Hepes and incubated with 20 g DNA (15 g caspase-12 [either wild-type or Cys299Ala mutant] + 5 g GFP) for 5 min on ice before being electroporated at 320 V, 1500 F. Following electroporation, cells were kept on ice for 5 min then grown in 20 ml media for 24 hrs. Four electroporation reactions (i.e. 80 million cells) were pooled for each caspase-12 [either wild-type or Cys299Ala mutant] transfection. The next day, live GFP-positive cells were sorted, pre-treated with 100 ng/ml phorbol myristate acetate (PMA) for 6 hrs then treated with TLR ligands for 24 hrs. Cells were then treated with 5 mM ATP in fresh media for 20 minutes, washed and further cultured in fresh media for 3 hrs. Cell supernatants were then analyzed for cytokine production using bead-based multiplex human immunoassays (described above). Caspase-1 activity assays HEK 293T cells were co-transfected using lipofectamineTM plus reagent (Invitrogen) with Flag-tagged caspase-1 and caspase-12 [either wild-type or Cys299Ala mutant]. 24 hrs after transfection, cell lysates were prepared in caspase activation buffer (20 mM Pipes pH 7.4, 100 mM NaCl, 1 mM EDTA, 10 mM DTT [added fresh], 0.1 CHAPS, 10 % sucrose and protease inhibitors), and 100 g lysates were assayed for cleavage of 100 M of the caspase-1 substrate WEHD-AFC. Kinetic measurements of AFC release were recorded every 9 minute for 30 min at room temp using a fluorescent plate reader (excitation of 400 nm and emission of 505 nm). Cell-free inflammasome activation assay As in 11, THP-1 cells were pre-stimulated with 1 g/ml LPS for 1 hr. Cells were harvested and washed with PBS, then lysed by swelling in 5 volumes of ice-cold hypotonic buffer W (20 mM HEPES-KOH [pH 7.5], 10 mM KCl, 1.5 mM MgCl2 1 mM Na EDTA, 1 mM Na EGTA, 0.1 mM PMSF, and the Roche protease inhibitor cocktail) and incubation on ice for 15 min. The cellular membrane integrity was then disrupted by passage 15 times through a G22 needle. Cell lysates were centrifuged, and the supernatants, following filtration (0.45 M), were used for this in vitro IL-1 cleavage assay. The lysates were incubated for 20 min on ice with either GST (control) or GST-rat caspase-12, then shifted to 30 °C and incubated for 60 min. IL-1 processing was monitored by Western analysis with a specific antibody against the mature form of IL-1 (Cell Signaling, cat. # 2021). Co-immunoprecipitation experiments HEK 293T cells were co-transfected using lipofectamineTM plus reagent (Invitrogen) with Flag-tagged caspase-1, caspase-5, caspase-9 C-A, and caspase12. 24 hrs after transfection, cell lysates were prepared in buffer B 150 (20 mM Tris-HCl pH 8.0, 150 mM KCl, 10% glycerol, 5 mM MgCl2, 0.1 % NP-40 and protease inhibitors) and caspases-1, 5, 9 were immunoprecipitated using Flag M2 agarose beads (Sigma) at 4 °C for 2 hrs, followed by three washes of the beads with lysis buffer. Immunoprecipitates were eluted from the beads using Flag 10 peptides (Sigma) and were processed for Western blot analysis using anti-mouse caspase-12 antibodies or anti-Flag antibodies (both antibodies from Sigma). NF-B activation assays HEK 293T cells were co-transfected using lipofectamineTM plus reagent (Invitrogen) with B–luc and -gal reporter plasmids, and a pcDNA3.1 empty vector or a plasmid encoding either human Csp-12L 5 or rat caspase-12. Twentyfour hrs after transfection, cells were treated with 10 ng/ml TNF for 6 hrs or were left untreated. Cell extracts were next prepared and relative luciferase activity was measured. For the MEFs, cells were transfected with B–luc and gal reporter plasmids, as above, and treated, 24 hrs after transfection, with TLR ligands for 6 hrs before assaying for B–luc activity. Statistical Analysis Log rank test and Fisher’s exact test were used to compare sepsis survival among caspase-12+/+ and caspase-12-/- mice. Student t-test was used for statistical analyses of apoptosis, bacterial clearance as well as cytokine production assays. References 1. Mathison, J. C., Wolfson, E. & Ulevitch, R. J. Participation of tumor necrosis factor in the mediation of gram negative bacterial lipopolysaccharide-induced injury in rabbits. J Clin Invest 81:1925-1937 (1988). 11