Title: Can plaque morphology and composition, and coronary risk
advertisement

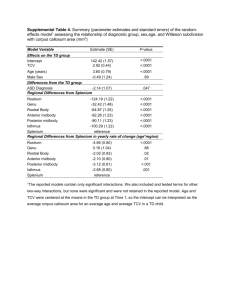
ONLINE APPENDIX Adjudicated Cause of Cardiac and Non-cardiac Deaths The adjudicated cause of cardiac and non-cardiac deaths in our cohort was as follows: (1) Cardiac deaths were adjudicated as fatal myocardial infarction (n=0), sudden cardiac death (n=3), worsening heart failure (n=6), and other cardiac death (n=3); (2) Noncardiac deaths were adjudicated as vascular death (n=0), non-hemorrhagic stroke (n=0), other (n=16), and unknown death (n=2). Sensitivity Analysis for Incomplete Follow-Up Methods Complete follow-up, defined as >90 days or through the end of the study period was not available for 71 (7.9%) patients. In order to evaluate the effects of incomplete follow-up, sensitivity analyses utilizing several approaches were conducted. First, right-point imputation was conducted wherein all patients with incomplete follow-up were imputed to have no events through the end of the study period. Although, the overall event rate among patients with complete follow-up was low (6.7%), this assumption was unlikely to be true. A second, more robust approach utilizing multiple imputation was also conducted. The primary outcome and time to this event were multiply-imputed with 25 imputations (relative efficiency >99.7%). Because event times were approximately exponentially distributed, they were log transformed prior to imputation. Cox proportional hazard models were fit to the imputed or multiply-imputed data. Parameter estimates for multiply-imputed data sets were then combined (1). Results Right-point imputation, which assumes that none of the patients with incomplete data experienced events during the follow-up period generated estimates for hazard ratios comparable to analysis of non-imputed data (Supplemental Table 1). Although calcium score (CAC) contained incremental prognostic information beyond clinical risk (Model 2), once coronary flow reserve (CFR) was incorporated (Model 4), CAC was no longer a significant predictor of the primary outcome (Model 4). 1 Multiple imputation resulted in imputation of between 1 and 9 MACE events, implying event rates of 1.4-12.7% among patients with incomplete follow-up, compared to 6.7% among those with complete follow-up. This approach also resulted in risk estimates that were essentially identical to those based on non-imputed data (Supplemental Table 1). References 1. Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons, Inc. 1987. 2 Online Table 1. Multivariable Survival Analysis (CAC zero vs ≥1) Model Model 1: Clinical risk score* Model 2: Clinical risk score Model 3: Clinical risk score + CFR Model 5: Clinical risk score + CAC + CFR + CAC Analysis Fit statistic p-value Fit statistic p-value Fit statistic p-value Fit statistic p-value Global χ2 19.0 ref 19.9 0.35 44.5 <0.0001 44.8 <0.0001 (vs. model 1) <0.0001 (vs. model 2) 0.54 (vs. model 3) AIC 588.6 ref 589.6 N/S 565.1 <0.0001 566.7 <0.0001 (vs. model 1) <0.0001 (vs. model 2) N/S (vs. model 3) c-index 0.632 ref [0.550-0.714] 0.638 0.57 [0.554-0.722] 0.719 0.004 [0.647-0.791] 0.719 0.003 (vs. model 1) [0.648-0.791] 0.007 (vs. model 2) 0.95 (vs. model 3) Covariate Duke clinical risk score Hazard ratio 1.06 [1.03-1.10] Hazard ratio <0.0001 1.06 Hazard ratio 0.003 [1.03-1.09] 1.06 Hazard ratio 0.0002 [1.03-1.10] 1.06 0.001 [1.02-1.09] (per 10%) CAC (≥1 vs. 0) 1.35 0.35 1.22 [0.72-2.51] CFR (per 10% increase) 0.54 [0.65-2.31] 0.82 [0.76-0.89] <0.0001 0.82 <0.0001 [0.76-0.89] A log transformation of the Duke clinical risk score and CFR was used for the analyses to adjust for the rightward skew of the data and to reduce heteroscedasticity. CAC was dichotomized as present or absent. Global χ2 indicated likelihood ratio chi-squared statistic for the entire model. AIC refers to Akaike Information Criterion. P-values for model fit statistics (i.e. global χ2, AIC and c-index) are for comparisons with model 1, unless specified. C-indices are calculated for 3-year event date. CAC = coronary artery calcium, CFR = coronary flow reserve. *The components to calculate Duke clinical risk score consist of age, sex, typical angina, atypical angina, history of myocardial infarction, ECG Q-wave, ECG ST-T wave changes, smoking, dyslipidemia, diabetes, age×sex, history of myocardial infarction×ECG Q-wave, age×sex, age×dyslipidemia, and sex×smoking (interaction).11 4 Online Table 2. Multivariable Survival Analysis (CAC <400 vs. ≥400) Model Model 1: Clinical risk score* Model 2: Clinical risk score Model 3: Clinical risk score + CFR Model 5: Clinical risk score + CAC + CFR + CAC Analysis Fit statistic p-value Fit statistic p-value Fit statistic p-value Fit statistic p-value Global χ2 19.0 ref 22.7 0.05 44.5 <0.0001 46.5 <0.0001 (vs. model 1) <0.0001 (vs. model 2) 0.14 (vs. model 3) AIC 588.6 ref 586.8 0.18 565.1 <0.0001 565.0 <0.0001 (vs. model 1) <0.0001 (vs. model 2) 0.75 (vs. model 3) c-index 0.632 ref [0.550-0.714] 0.623 0.46 [0.542-0.705] 0.719 0.004 [0.647-0.791] 0.712 0.006 (vs. model 1) [0.641-0.783] 0.003 (vs. model 2) 0.22 (vs. model 3) Covariate Duke clinical risk score Hazard ratio 1.06 [1.03-1.10] Hazard ratio <0.0001 1.06 Hazard ratio 0.0005 [1.02-1.09] 1.06 Hazard ratio 0.0002 [1.03-1.10] 1.06 0.001 [1.02-1.09] (per 10%) CAC (≥400 vs <400) 1.76 0.05 1.53 [1.01-3.09] CFR (per 10% increase) 0.14 [0.87-2.70] 0.82 [0.76-0.89] <0.0001 0.82 <0.0001 [0.76-0.89] 5 A log transformation of the Duke clinical risk score and CFR was used for the analyses to adjust for the rightward skew of the data and to reduce heteroscedasticity. CAC was dichotomized as <400 or ≥400. Global χ2 indicated likelihood ratio chi-squared statistic for the entire model. AIC refers to Akaike Information Criterion. P-values for model fit statistics (i.e. global χ2, AIC and c-index) are for comparisons with model 1, unless specified. C-indices are calculated for 3-year event date. CAC = coronary artery calcium, CFR = coronary flow reserve. *The components to calculate Duke clinical risk score consist of age, sex, typical angina, atypical angina, history of myocardial infarction, ECG Q-wave, ECG ST-T wave changes, smoking, dyslipidemia, diabetes, age×sex, history of myocardial infarction×ECG Q-wave, age×sex, age×dyslipidemia, and sex×smoking (interaction).11 6 Online Table 3. Sensitivity Analysis No Imputation Hazard Ratio P-Value Right-Point Imputation Hazard Ratio P-Value Multiple Imputation Hazard Ratio P-Value Model 1 Clinical Risk Score (per 10% increase) 1.06 [1.03-1.10] <0.0001 1.06 [1.03-1.09] 0.0001 1.06 [1.03-1.09] <0.0001 Clinical Risk Score (per 10% increase) 1.05 [1.02-1.08] 0.003 1.05 [1.01-1.08] 0.006 1.05 [1.02-1.08] 0.004 CAC (per 2-fold increase) 0.02 1.09 [1.01-1.17] 0.02 1.08 [1.01-1.16] 0.02 0.0002 1.05 [1.02-1.09] 0.0006 1.06 [1.03-1.09] 0.0003 Model 2 1.09 [1.01-1.17] Model 3 Clinical Risk Score (per 10% increase) 1.06 [1.03-1.09] CFR (per 10% increase) 0.82 [0.76-0.89] <0.0001 0.83 [0.77-0.89] <0.0001 0.82 [0.76-0.89] <0.0001 Model 4 Clinical Risk Score (per 10% increase) 1.05 [1.02-1.09] 0.004 1.04 [1.01-1.08] 0.01 1.05 [1.01-1.08] 0.006 CAC (per 2-fold increase) 1.06 [0.98-1.13] 0.14 1.06 [0.99-1.14] 0.11 1.06 [0.98-1.13] 0.15 CFR (per 10% increase) 0.83 [0.76-0.89] <0.0001 0.83 [0.77-0.90] <0.0001 0.83 [0.76-0.90] <0.0001 CAC = coronary artery calcium, CFR= coronary flow reserve Online Table 4. Risk Reclassification Pre-test Model (=Clinical Risk Score) Post-CAC Model Post-CFR Model Post-CAC&CFR Model Annual Risk Annual Risk Annual Risk <2% 2-6% >6% <2% 2-6% >6% <2% 2-6% >6% 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 0 (0) 2-6% 2.4 (3) 53.1 (76) 14.7 (21) 0 (0) 40.6 (61) 26.0 (39) 2.5 (4) 32.1 (50) 29.4 (46) >6% 0 (0) 9.5 (14) 59.9 (86) 2.8 (4) 15.6 (22) 54.0 (75) 4.0 (6) 5.1 (7) 62.0 (87) Events Group Annual Risk <2% Event NRI 0.025 0.043 0.131 No Events Group Annual Risk <2% 80.0 (92) 7.0 (8) 0 (0) 69.0 (79) 18.0 (21) 0 (0) 67.0 (77) 20.0 (23) 0 (0) 2-6% 43.6 (11) 301.9 (77) 46.3 (12) 143.0 (36) 186.4 (47) 66.0 (17) 147.5 (37) 180.9 (45) 69.6 (17) >6% 0 (0) 96.5 (34) 186.1 (66) 14.2 (5) 107.4 (38) 158.0 (57) 24.0 (9) 109.9 (39) 147.0 (52) Non-Event NRI 0.116 0.237 0.255 Reclassification table for censored data using method of Steyerberg and Pencina20 from 3-year event data. NRI = net reclassification index. Numbers in parenthesis reflect percentage of pre-test subpopulation. 8 Online Table 5. Net reclassification improvement and integrated discrimination index Baseline Model Addition Net reclassification Clinical risk score Clinical risk score Clinical risk score Clinical risk score Clinical risk score +CAC +CFR +CAC +CFR +CAC +CFR +CFR +CAC 0.324 [-0.045-0.734] 0.461 [0.098-0.848] 0.587 [0.225-0.948] 0.467 [0.111-0.863] 0.386 [0.025-0.755] 0.141 [-0.003-0.286] 0.280 [0.048-0.502] 0.386 [0.213-0.585] 0.270 [0.077-0.457] 0.136 [-0.012-0.332] 0.013 [0.009-0.019] 0.101 [0.073-0.145] 0.099 [0.070-0.143] 0.086 [0.059-0.125] -0.003 [-0.010-0.004] 0.296 [0.209-0.384] 2.306 [1.760-2.927] 2.245 [1.702-2.862] 1.505 [1.137-1.932] -0.018 [-0.063-0.025] improvement (Continuous) Net reclassification improvement (2 & 6%) Integrated discrimination index Relative integrated discrimination index Log transformation of the Duke clinical risk score, CFR and CAC + 1 were used for the analyses to adjust for the rightward skew of the data and to reduce heteroscedasticity. Estimates are presented with 95% confidence intervals. The net reclassification improvement across clinically meaningful risk categories of <2%, 2-6% and ≥6% per year was used for analysis. CAC = coronary artery calcium, CFR= coronary flow reserve 9