13. Pulmonary embolism, deep venous thrombosis
advertisement

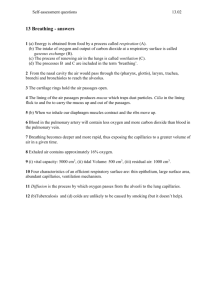
11. Shortness of breath Definition. Hyperventilation. Non-pulmonary causes: metabolic acidosis, anxiety Initial evaluation. Overall look, vital signs, O2 sat, lung exam, ABG, CXR, ancillary data (meds, WBC, EKG), comorbid conditions Red flags: looks tired, RR 40s, O2 sat <85%, pH <7.25, pCO2 >70 ABG. Calculate A-a gradient (see Formulae section) Hypoxemia. Altitude Alveolar hypoventilation (pneumonia, edema) V/Q mismatch. Hypoxemia sensitive to 100% O2 (COPD, pulmonary embolism) Shunt. Hypoxemia refractory to 100% O2 (pulmonary edema, pneumonia, atelectasis) Decreased diffusion Hypercarbia. pCO2 = VCO2 / (VE VD) Increased VCO2 Decreased VE (min ventilation): decreased RR or VT Increased VD (dead space) Increased carbohydrate intake Increased metabolic production of CO2 Differential diagnosis Pulmonary edema, CHF, asthma/COPD, pneumonia/aspiration, mucus plug, pulmonary embolism, ARDS, interstitial lung disease, pneumothorax, empyema/pleural effusion, anxiety/panic Pulmonary edema, CHF Consider ischemia (cause or effect), valvular disease (MR, MS, AS), tamponade COPD. Increased FiO2 leads to increased pCO2 from: Retention problem not solved Worsening V/Q mismatch Haldane effect (deoxygenated hemoglobin having a greater affinity for CO2 than oxygenated hemoglobin) Decreased hypoxic drive Conservative treatments CHF: L M N O P (Lasix – morphine – nitrates – O2 – positioning) COPD: Nebulizers, steroids, antibiotics Asthma: consider Heliox Pneumonia: antibiotics (ceftriaxone/azithro, levoflox metronidazole, vanco/cefepime), chest PT, suctioning Mucus plug: suctioning/bronch (page thoracic surgery for rigid bronch if pulmonary not available) Pulmonary embolism: anticoagulation Pneumothorax/pleural effusion/empyema: chest tube (page general surgery) Oxygen delivery. Nasal cannula: FiO2 ~3% per L (caution in “mouth breathers”) Face mask: FiO2 28%-98%, 15L maximum Face tent: if pt claustrophobic, FiO2 is variable Non-rebreather: FiO2 up to 100%, 45 L maximum (limited by RR) High flow O2: FiO2 up to 100%, for patients with very high RR Also consider noninvasive ventilation from BiPAP or CPAP machine. Jose Florez, M.D., Ph.D. MGH Medical Housestaff Manual 41 12. COPD Evaluation Look for precipitants (URI/pneumonia, medical noncompliance, CHF, occupational or environmental exposures, pneumothorax) Check for most recent PFTs (FEV1, FEV1/FVC ratio, TLC, DLCO) to assess severity of disease Check previous ABGs between exacerbations for evidence of CO2 retention Look for use of accessory muscles, ability to speak in full sentences, vital signs, oxygen saturation, wheezing, rhonchi, tympany to percussion (pneumothorax), or dullness (pneumonia), acrocyanosis, diaphoresis. Changes in level of consciousness and decrease in wheezing merit an ABG to look for hypercapnia secondary to respiratory fatigue. Labs: CBC, chem 7 CXR: use to evaluate for presence of pneumonia or pneumothorax Blood and sputum cultures: only if you suspect pneumonia as a cause of the exacerbation. PFTs are not useful in the acute setting. Could consider PFTs after exacerbation is over. Treatment Oxygen to maintain a goal oxygen saturation of 88-93% in patients known to retain CO2 or PaO2 of 60-70 mm Hg). If oxygen sats are acutely raised to >95% in this patient population it may precipitate respiratory failure due to worsened V/Q mismatch, the Haldane effect on the Hb-CO2 dissociation curve, and decreased respiratory drive. Albuterol 2.5/5 cc q1-2h during the acute phase is the first line of treatment. As symptoms improve, may switch to less frequent regimen (albuterol nebs q4h with albuterol q2h PRN) Ipratropium (Atrovent) nebulizer 0.5 mg q4-6h along with albuterol has been demonstrated to have a synergistic effect in improving airflow during COPD flares. Corticosteroids have been demonstrated to have a role in decreasing morbidity in patients with COPD flares. A high dose would be Solu-Medrol 125 mg IV q6h x 24-48h and then switch to prednisone 60 mg PO qd. Taper prednisone dose according to improvement in symptoms and airflow movement during physical exam. Antibiotics may have a role in treatment of infection causing flares or shortening the hospital stay in those without obvious infections. A trial of azithromycin 250 mg PO qd x 5 d and/or a second/third generation cephalosporin (cefuroxime/ceftriaxone) is reasonable. The role of theophylline on acute COPD flares is controversial. Trial of BiPAP, consider in patients who have decrease in level of consciousness, mental status changes, RR >30 and ABG with pO2 <45, and pH <7.35. If patient does not improve or tolerate BiPAP then consider intubation and transfer to the MICU for further care. Jose Florez, M.D., Ph.D. Vinicio de Jesus-Perez, M.D. MGH Medical Housestaff Manual 42 13. Pulmonary embolism, deep venous thrombosis Background Risk factors include stasis (inactivity, bed rest, CHF), hypercoagulability (malignancy, factor V Leiden, lupus anticoagulant, see below), and vascular injury (surgery, trauma). Clinical signs and symptoms are nonspecific in both DVT and PE, and interpretation of diagnostic testing heavily influenced by the level of clinic suspicion (pre-test probability). History Symptoms and signs of both DVT and PE are nonspecific, and they are frequently asymptomatic. Symptoms of DVT include calf pain, edema, venous distension, and pain with dorsiflexion on the foot (Homans’s sign). Symptoms of PE may vary with the size of the infarct; these include dyspnea, chest pain, cough. With infarction, patients may complain of hemoptysis and/or pleuritic chest pain. Modified Wells criteria developed to address problem of non specificity (Ann Intern Med 2001;135:98-107) Note that low, moderate, and high categories do not strictly correlate with PIOPED criteria). Modified Wells criteria Signs/symptoms of DVT Alternative diagnosis less likely than PE Heart rate >100 Immobilization (bedrest 3 days) Surgery within 4 weeks Previous DVT/PE Hemoptysis Malignancy 3 pts 3 pts 1.5 pts 1.5 pts 1.5 pts 1.5 pts 1 pt 1 pt Pretest probability Low <2 pts Moderate 2-6 pts High >6 pts % with PE 1.3% 16.2% 40.6% Differential diagnosis For DVT, includes musculoskeletal injuries, Baker’s cyst, and lymphatic or venous insufficiency. For PE, includes other pulmonary processes such as pneumothorax, pneumonia, asthma, pleural effusion, pleurisy; cardiac processes such as MI, CHF, pericarditis, pericardial tamponade; also consider GI and musculoskeletal diagnoses Laboratory evaluation and testing Deep venous thrombosis Venous ultrasound (color flow Doppler with compression ultrasound) has high sensitivity (89-100%) and specificity (89-100%) compared to venography (gold standard) for proximal DVT, slightly less for calf DVT. Sensitivity is much lower in asymptomatic patients (33%). In situations where there is low clinical suspicion for PE and nondiagnostic lung scans, negative serial leg studies over two weeks are sufficient to safely withhold anticoagulation in patients with adequate cardiopulmonary reserve, especially when the D-dimer is negative (see below). Pulmonary embolism EKG findings and vary and include (Chest 1997;111:537): Normal EKG 9-24% (12-50%) T wave inversions from V1-V4 (42-68%) S1Q3T3 pattern (S in I, Q in III >1.5 mm with T wave inversion in III) (12-52%) Sinus tachycardia (26-90%) Complete or incomplete RBBB (15-40%) CXR is abnormal in the majority of patients with PE, but findings are nonspecific and include elevation of a hemidiaphragm, atelectasis, or an effusion. Classic signs of “Hampton’s hump” (pleural-based infiltrate) and “Westermark’s sign” (decreased vascularity) are suggestive but are rare. ABG classically shows hypoxemia and an elevated A-a gradient, However ABG was not helpful in distinguishing patients with PE in the PIOPED study. MGH Medical Housestaff Manual 43 13. Pulmonary embolism, deep venous thrombosis Lower extremity non invasive studies. In PIOPED, <30% had signs or symptoms of deep venous thrombosis. 29% of patients with V/Q or angiographic evidence of pulmonary embolism had positive LENI (Ann Intern Med 1997;126:775) D-dimers are usually elevated in pulmonary embolism (>500 ng/mL). ELISA assay used at MGH; more sensitive and specific than latex agglutination assay In some studies, the NPV has been as high as 96%; in patients with a high pre-test probability of PE, however, D-dimers have been <500 ng/mL in as much as 16%. In cancer, the lower NPV (78.9% in one study) limits its utility (because of high prevalence of DVT). Many experts agree that in patients where there is low clinical suspicion, a D-dimer <500 ng/mL allows the work-up to be considered negative and stopped. V/Q scanning is sensitive but nonspecific. A normal scan virtually excludes pulmonary embolism, but abnormalities can be caused by atelectasis, asthma, COPD, etc. PIOPED PIOPED study (JAMA 1990;263:2753) Clinical probability shows proportion with pulmonary embolism V/Q scan category High Inter. Low using pulmonary angiograms as the High 95% 86% 56% standard. Clinical probability determined by Intermediate 66% 28% 15% Low 40% 15% 4% overall impression, not by algorithm Normal/near normal 0% 6% 2% CT angiogram accuracy evolving. A sensitivity of 60-80% and specificity of 80-95% for segmental or larger pulmonary emboli has been reported. The advantage of CT is that an alternative diagnosis is found in up to 1/3 of patients tested; contrast load is a concern, however, especially if PA-angiogram follows. Remember that patients must be able to perform a 20 s breath hold. Pulmonary angiogram remains the gold standard: morbidity 5%, mortality less than 0.5% (usually related to catheter insertion or contrast reactions). Echocardiogram can be helpful in risk-stratifying patients. Right ventricular dysfunction is associated with hemodynamically significant PEs and worse outcomes; some experts recommend lysis or thrombectomy in this setting. McConnell’s sign (RV dysfunction with apical sparing) may be useful to distinguish RV dysfunction due to PE as opposed to other causes. Troponin. Troponins can be elevated in pulmonary embolism from acute RV shear stress, RV microinjury, and microinfarction. Elevated troponin T (>0.01 ng/mL) associated with worse outcome and death. May be helpful in triaging patients (Chest 2003;123:1947) Treatment The mainstay of treatment for both DVT and PE is anticoagulation. Therapeutic anticoagulation must be achieved within 24 hours or the risk of extension and/or recurrence increase substantially (up to three months later). Consider referral to Anticoagulation Management Services Deep venous thrombosis Patients are given LMWH and warfarin is started. LMWH may not be appropriate for patients with renal failure, obesity (given weight-based dosing), or patients where invasive procedures may be planned (e.g., surgery). Dalteparin is the LMWH on formulary at MGH; dosed at 100 U/kg SC MGH Medical Housestaff Manual Pilot referral program Anticoagulation Management Services Outpatient care (Clinics One, Suite 144) Phone 617-726-2768 Fax 617-726-2546 Pager 30104 Transition Care, White 806B Phone 617-726-9616 Fax 617-724-2976 Pager 30103 44 13. Pulmonary embolism, deep venous thrombosis q12 hours (round to nearest 500, max 10,000 U). Enoxaparin is 1 mg/kg s.c. q12h. LMWH continued for at least 5 days and not stopped until INR is therapeutic for at least two days. Consider unfractionated heparin in patients who have significant renal impairment, imminent procedures, or at extremes of weight Unfractionated heparin is bolused at 80 U/kg and infused starting at 18 U/kg, with a goal PTT at 6084. Patients are eligible for outpatient treatment with low molecular weight heparin (LMWH) if the following criteria are met: no ilio-femoral involvement of clot, expected compliance, weight between 50-150 kg (110-250 pounds), Cr<2, normal platelet count, low risk for bleeding, no need for surgery Long-term anticoagulation in next 24 hr. Patients with social needs or Reversible or time-limited risk factors, at least 3 months significant co-morbidities can be treated at a First episode of idiopathic DVT/PE, at least 6 months subacute facility. Recurrent idiopathic DVT/PE or a continuing risk factor For LMWH, anti-Xa levels usually do not need (e.g. cancer, antithrombin deficiency, anticardiolipin to be monitored (see anticoagulation section). antibody syndrome), 12 months or longer Duration of therapy continues to be individualized for Thrombolytic therapy is approved for proximal protein C or S deficiency, multiple thrombophilic DVT to reduce post-phlebitic complications. Pulmonary embolism conditions, homocystinemia, and homozygous factor V Leiden From Sixth ACCP Consensus Conference on Antithrombotic Therapy 2001 Similar to DVT. Enoxaparin is approved for use in DVT with or without PE, but most PE patients are observed in-hospital. At MGH, dalteparin (Fragmin) can be considered as an off label use for PE for patients who are hemodynamically stable. In absence of hemodynamic compromise, role of thrombolysis is controversial; goal of thrombolysis (within 14 days) is to prevent long-term pulmonary complications; some consider RV dysfunction on echo to be an indication. If anticoagulation is strongly contraindicated, an IVC filter should be placed to reduce further embolism. Thrombectomy by surgery is occasionally used to remove large, hemodynamically significant clots. Hypercoagulable workup Thrombolysis FDA-approved dose Alternative Following are thrombophilic states that drugs dose may warrant testing for in patients who 250,000 U bolus over 1,500,000 U Streptokinase present with DVT or PE: 20 min over 1 hr Activated protein C resistance. Most 100,000 U/hr over 24commonly due to factor V Leiden. 72 hr Roughly 20% of patients with venous 4,400 U/kg bolus, 3,000,000 U Urokinase 4,400 U/kg/hr for 12 hr over 2 hr thromboembolism carry this mutation. 100 mg over 2 hours 0.6 mg/kg TPA Prothrombin G20210A mutation. over 3-15 min Roughly 7% of patients with venous thromboembolism carry this mutation. Antiphospholipid antibody syndrome. Hyperhomocysteinemia. Less common are antithrombin deficiency, protein C deficiency, protein S deficiency. Cost $350 $2000-$2700 $2000-$4200 Wells Messersmith, M.D. Andrew Yee, M.D. MGH Medical Housestaff Manual 45 14. Noninvasive ventilation Background Non-invasive ventilation involves respiratory assistance without use of an endotracheal tube or laryngeal mask airway. In recent years, non-invasive methods of ventilation have become important alternatives to intubation for supportive respiratory care. Types of non-invasive ventilation Refer to Am J Resp Crit Care Med 2001;163:540 and N Engl J Med 1997;337:1746. Continuous positive airway pressure (CPAP). Delivers a set, constant positive pressure that is greater than atmospheric pressure throughout both inspiration and expiration. At end-expiration CPAP keeps alveoli from collapsing. Bilevel positive airway pressure (BiPAP). Delivers positive pressure during inspiration and expiration, with increased pressure during inspiration to assist ventilation by increasing tidal volume. Hence there is support during inspiration and CPAP to keep airspaces open at end-expiration (BiPAP includes CPAP). Two pressures are set on machine: IPAP (inspiratory positive airway pressure) is the pressure applied during inspiration and is synonymous with PSV of mechanical ventilation (IPAP = PS + PEEP). EPAP (expiratory positive airway pressure) is the pressure applied during expiration (EPAP = PEEP = CPAP). Effects of CPAP. Typical settings 5-12 cm H2O. Alveolar recruitment and prevents alveolar collapse. V/Q mismatch. Decreases afterload by increased intrathoracic pressure on the left ventricle. May decrease preload due to increased intrathoracic pressure on the IVC esp. in hypovolemia. Reduces cardiogenic pulmonary edema by resisting increased pulmonary capillary pressures. Effects of NPPV (BiPAP). Typical settings IPAP 6-14 cm H2O, EPAP 3-5 cm H2O. Effective tidal volumes, respiratory rate determined by patient. Respiratory work and reduces breathing fatigue. Alveolar recruitment and prevents alveolar collapse. V/Q mismatch. Clinical indications See also N Engl J Med 1997;337:1746. Generally CPAP useful for hypoxemia, BiPAP useful for hypercapnia or mixed picture Acute CHF (CPAP favored). OSA (CPAP favored unless hypoventilation also present). Severe COPD (BiPAP). Pneumonia, ARDS/ALI (CPAP favored but note contraindications). Contraindications Hemodynamic instability. Respiratory arrest. Refractory hypoxemia (PaO2 <60 mmHg at 100% O2. Risk of airway compromise/aspiration. Life-threatening arrhythmia. Copious secretions. Poor mental status . Refractory to prior NPPV attempts. Ed Bajwa, M.D. MGH Medical Housestaff Manual 46 15. Mechanical ventilation Ventilator cycling Volume-cycling. Note any mode except PSV can be either volume- or pressure-cycled Delivers a constant tidal volume with a fixed inspiratory flow and time Peak airway pressures depends on lung compliance Preferred for patients who require a fixed VE Pressure-cycling Delivers a positive pressure breath at a constant airway pressure Inspiratory time is fixed on the ventilator and inspiratory flow is variable Preferred in patients with acute lung injury, ARDS to avoid over distension from high alveolar pressures Ventilator modes Controlled mechanical ventilation (CMV). Breathing fully determined by ventilator, no patient input; used for fully anesthetized patients without spontaneous respiration. Variables. Tidal volume (TV) (if volume-cycled, sometimes called volume-control ventilation or VCV), peak inspiratory pressure (PIP) (if pressure-cycled, often called pressure-control or PCV), and respiratory rate (RR). Use. Patients not spontaneously breathing, requiring full ventilatory support. Intermittent mandatory ventilation (IMV). Gives patients a set minimum RR but allows spontaneous breaths in between mandatory breaths. Variables. Mandatory RR, TV (if volume-cycled), or PIP (if pressure-cycled); spontaneous breaths by patient do not get any additional support from ventilator Use. Not used much at MGH, once thought to be good for weaning but not shown to be helpful Assist/control ventilation (A/C). Ventilator delivers a fully augmented breath when patient attempts to inspire, also delivers a certain number of mandatory breaths if patient not taking sufficient number of breaths. Variables. TV (volume-cycled) or PIP (pressure-cycled) are determined by the ventilator. Use. Sedated patients with some spontaneous breathing. Pressure support ventilation (PSV). Supports the patient’s own breathing efforts by deliver pressure to augment patient’s spontaneous breaths. Patient controls the RR, inspiratory time, I:E ratio. Use. Patients spontaneously breathing, requiring minimal vent support, commonly used to wean patients off mechanical ventilation by gradually decreasing amount of support. Clinical indications for intubation Am J Med 1990; 88:268 Hypercapnia ( pCO2 >50 mm Hg + arterial pH <7.35) Severe COPD Status asthmaticus Respiratory muscle fatigue (insp force <25 mm H2O) Central hypoventilation (e.g. from brainstem injury, obtundation, narcosis) Hypoxia ( pO2 <60 mm Hg with FiO2 >0.6) Pulmonary edema Pneumonia ALI/ARDS Pulmonary embolus (massive) Airway protection/management Delirium tremens Status epilepticus Airway compromise (aspiration, neck infection, laryngeal edema, obstructing mass, etc.) Acid-base disturbances Metabolic/resp acidosis (to improve elimination of acid) Therapeutic hyperventilation (to reduce elevated ICP) How to treat low PaO2 (“patient desatting”) Increase PEEP MGH Medical Housestaff Manual 47 15. Mechanical ventilation PEEP improves blood oxygenation by preventing alveoli from collapsing at end-expiration and thus improving V/Q matching. Watch for hemodynamic effects: may decrease afterload by compressing LV, may decrease preload by compressing IVC (especially prominent if patient hypovolemic) Useful in cardiogenic pulmonary edema because PEEP can overcome increased pulmonary capillary pressures. Increase FiO2 Be careful of O2 toxicity, FiO2 >60% for prolonged periods can potentiate free-radical mediated lung injury How to treat high PaCO2 (“patient underventilated”) If volume-cycled, increase TV If pressure-cycled, increase inspiratory pressures Use caution; high volumes or pressures can cause VALI (ventilator-associated lung injury). In general, Pplat <30 is safest (or whatever volume setting produces a Pplat of <30). Increase RR RR should not be increased above 25-35 maximum, or patient will not have time to exhale, resulting in breath-stacking and potentially auto-PEEP. Lung protective strategies (N Engl J Med 2000;342:1301-1308) Patients with acute lung injury and ARDS did better with lower tidal volumes (initial 6 mL/kg and plateau pressure of <30 cm H2O) compared to “traditional” initial tidal volumes (12 mL/kg and plateau pressure <50 cm H2O) Mortality 31.0% with lower tidal volume strategy compared to 39.8% at 180 days Common problems ARDS/ALI. Definition PaO2/FiO2 <200 (<300 for ALI), acute onset of respiratory distress, bilateral infiltrates on CXR, and absence of CHF (e.g. wedge pressure <18 mm Hg), Use lung protective strategy (N Engl J Med 2000;342:1301); see above. Auto PEEP. Excessive amounts of PEEP due to insufficient expiration, resulting in adverse hemodynamic effects and overdistention. To correct, adjust set PEEP and expiratory time. Weaning from mechanical ventilation Although weaning has been the traditional approach to taking a patient off mechanical ventilation, recent data has shown that daily spontaneous breathing trials can reduce the duration of mechanical ventilation of patients. (N Engl J Med 1996;335:1864; N Engl J Med 1995;332:345). Based on this, the following approach to extubation/weaning is suggested: Assess underlying disease and decide whether mechanical ventilation is required for treatment Conduct a spontaneous breathing trial—using the parameters below, determine if extubateable Either extubate if indicated or start weaning by the methods explained below Parameters predicting ability to wean/extubate (N Engl J Med 1991; 324:1445-50) Maximal inspiratory pressure < 15 cm H2O Minute ventilation VE <15 L/min Tidal volume >325 mL TV/kg > 4 mL/kg MGH Medical Housestaff Manual PPV NPV 0.59 0.55 0.73 0.67 1.00 0.38 0.94 0.85 48 15. Mechanical ventilation Dynamic compliance (CD) 0.65 Static compliance (CS) 0.60 PaO2/ PAO2 >0.35 0.59 Rapid Shallow Breathing Index (RR/TV <105 breaths/min/L) 0.78 CROP = [CD x Pmax (PaO2/ PAO2)] / RR 0.71 The Rapid Shallow Breathing Index is commonly used at MGH. 0.58 0.53 0.53 0.95 0.70 Methods of weaning Respiratory therapy and nursing are very helpful in managing ventilation wean and extubation. Weaning via pressure support ventilation is most commonly used method at MGH. T-piece (spontaneous breathing) trial. Short breathing trials of increasing times while completely disconnected from the ventilator (T-piece not generally used at MGH), i.e. no pressure support. CPAP trial. Similar to spontaneous breathing trial but patient is connected to the ventilator, i.e. pressure support set generally at 5 cm H2O, other variables (e.g. RR, TV) determined by patient. (Most commonly used at MGH). Note that some patients may develop pulmonary edema after extubation as they may rely on the positive pressure to decrease preload. SIMV. RR is set but allows spontaneous breathing between mandatory breaths, wean by decreasing mandatory rate (not generally used at MGH) Pressure support ventilation. Allows spontaneous breathing with ventilator assisted breaths, wean by decreasing pressure support to CPAP trial level For example reducing pressure support over time to 5 cm H2O and then performing CPAP trial. There is conflicting evidence on which ventilation weaning method is superior (see below) N Engl J Med 1995;332:345, spontaneous breathing trial weaned faster. Once-daily trial of spontaneous breathing led to extubation about three times more quickly than intermittent mandatory ventilation and about twice as quickly as pressure-support ventilation. Multiple daily trials of spontaneous breathing were equally successful. Am J Resp Crit Care Med 1994;150:896 study, Pressure support ventilation appears to reduce time spent on a ventilator. Weaning time significantly shorter with PSV (5.7 ± 3.7 days) than with IMV (9.9 ± 8.2 days) or trials of spontaneous breathing (8.5 ± 8.3 days). Consider extubation from mechanical ventilation to non invasive ventilation (e.g. BiPAP or CPAP). Ed Bajwa, M.D. MGH Medical Housestaff Manual 49