mucus controlling
advertisement

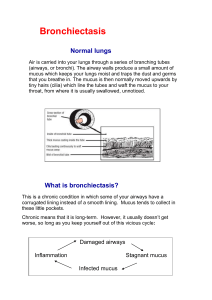
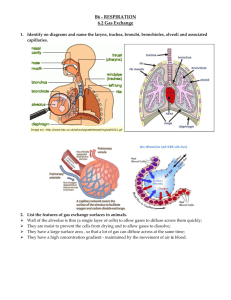
Mucus Controlling Agents Drug Control of Mucus I. One of the major defense mechanisms of the lung is the selfrenewing, self-cleansing mucociliary escalator a. Mucus seems to serve protective purposes i. Lubrication ii. Waterproofing iii. Protection against osmotic changes iv. Protection against inflammatory changes b. Failure of this system results in mechanical obstruction of the airway, with thickened, adhesive secretions II. Historically, drug therapy for respiratory secretions has been aimed at liquefying thick mucus to a watery state III. Diseases associated with abnormal mucociliary function a. Bronchitis i. ATS definition: daily, productive cough for 3 consecutive months each year for 2 consecutive years ii. Hypertrophy of submucosal glands iii. Increased number of goblet cells b. Bronchiectasis i. dilation and distortion of bronchi leading to impaired clearance c. Cystic fibrosis i. increased viscosity of secretions leading to impaired clearance ii. retention of secretions leads to chronic bacterial infection d. Asthma i. increased mucus production 1. during acute episode 2. may be a chronic feature of asthma Clinical Indication for Use I. To reduce accumulation of airway secretions a. improvement in pulmonary function b. improvement in gas exchange c. prevention of repeated infection d. prevention of airway damage Identification of Agents Drug Acetylcysteine 10% Brand Name Mucosil-10 Adult Dosage SVN: 6-10 ml tid or qid Use Secretion mobilization Acetylcysteine 20% Mucomyst, Mucosil-20 SVN: 3-5 ml of 20% solution tid or qid Direct Instillation: 1-2 ml Secretion mobilization Dornase alfa Pulmozyme Cystic fibrosis Aqueous solutions: Water, saline (0.45%, 0.9%, 5-10%) N/A SVN: 2.5 mg ampule, one ampule qd SVN: 3-5 ml USN: 3-5 ml Sputum induction, secretion mobilization Physiology of the Mucociliary System I. Components of the mucociliary system a. Surface epithelial cells b. Pseudostratified, columnar, ciliated epithelial cells c. Surface goblet cells d. Clara cells in the distal airways e. Submucosal glands i. Serous cells ii. Mucous cells II. Mucociliary Escalator a. Primary defense mechanism against mucus obstruction in the airways b. Lines the nasal cavity, oropharynx and the conducting airways III. Mucus Production a. Submucosal glands i. found in the cartilaginous airways ii. produce the majority of the mucous blanket iii. secretions from the mucous cells and serous granular cells mix together and are secreted through a ciliated duct onto the airway lumen iv. under parasympathetic (vagal) control 1. respond to cholinergic stimulation a. increased mucus production v. also respond to sympathetic stimulation vi. histology of the lining of the tracheobronchial tree ep=surface epithelial cells LP=lamina propria d = ducts of submucosal glands b. Goblet cells i. Found in the cartilaginous airways ii. interspersed among the ciliated columnar cells (5:1) iii. Not directly innervated by the nervous system 1. respond to irritation 2. may respond to sympathomimetic agents IV. The Mucous Blanket a. Terms i. Mucus - total secretion from the mucous membranes 1. surface goblet cells 2. submucosal glands ii. Sputum - mucus plus saliva iii. Viscosity – resistance to flow iv. Elasticity - property of deforming under force, then resuming its previous state b. Two layers i. Gel 1. on top near airway lumen 2. behaves partially as a fluid a. has viscosity b. flows forward under applied force (cilia) 3. behaves partially as a solid a. has elasticity b. gel is stretched and elastic recovery moves it forward ii. Sol 1. adjacent to the epithelial lining 2. has some viscosity but no elasticity 3. watery airway surface fluid V. Ciliary System a. Mucociliary transport results from the movement of the mucous gel by the beating cilia b. A ciliary beat is made up of an effective (power) stroke and a recovery stroke i. effective stroke 1. the cilia moves in an upright position to contact the underside of the gel layer and move it forward ii. recovery stroke 1. the cilia swing back around to the starting point through the sol layer c. Approximately 200 cilia per cell d. Beat 660-1080 per minute VI. Factors Affecting Mucocilary Transport a. COPD b. Parasympatholytics (Atropine) c. Narcotics d. Endotracheal suctioning e. Cigarette smoke f. Atmospheric pollutants g. Hyperoxia h. Hypoxia VII. Nature of Mucus Secretion a. Healthy individuals produce 100 ml/24 hours b. Clear viscoelastic substance c. Most reabsorbed in the bronchial mucosa d. About 10 ml reaches the glottis i. Swallowed or aspirated e. Increased in disease states f. Milk not found to increase mucous production g. Functions to transport and remove trapped inhaled particles, cellular debris, or dead and aging cells VIII. Characteristics of Infected Mucus a. The DNA from WBC debris changes mucus from clear to opaque b. The enzyme myeloperoxidase (cellular breakdown) changes mucus to yellow or green IX. Structure of mucus molecule a. Complex, high-molecular-weight macromolecule i. Polypeptide backbone (protein) formed by a string of amino acids ii. Carbohydrate side chain b. Forms a flexible strand cross-linked with disulfide bonds and sometimes hydrogen bonds c. Constituents of Mucus i. 95% H2O ii. 3% protein and carb iii. 1% lipids iv. <0.03% DNA Mucus Controlling Agents I. Terms Associated With Drug Therapy of Respiratory Secretions Term Definition Mucoactive Any agent that has an effect on mucus secretion Mucoregulatory An agent that reduces mucus hypersecretion to normal levels Mucolytic An agent that breaks down the structure of mucus, usually reducing viscosity and elasticity Mucokinetic An effect of improving the mobilization and clearance of mucus Mucospissic An effect of increasing the viscosity and elasticity of mucus secretion Expectorant An agent improving expectoration of respiratory secretions, usually by stimulation of bronchial gland output II. Options for controlling mucous hypersecretion a. Remove causative factors where possible i. Treat infections ii. Stop smoking iii. Avoid pollution and allergens b. Optimize tracheobronchial clearance i. bronchodilators ii. bronchial hygiene 1. hydration 2. DB&C 3. PD&P iii. Improve airflow by exercise and nutrition rehabilitation iv. Reduce inflammation 1. antibiotics 2. corticosteroids v. Use mucoactive agents as indicated 1. mucolytics 2. expectorants III. Mucolytic Agents a. Acetylcysteine i. Brand Names 1. Mucomyst 2. Mucosil-10 3. Mucosit-20 ii. Indications 1. treat thick secretions (inhaled or instilled (topical) 2. treat acetaminophen overdose (oral) a. to prevent hepatic injury iii. Administration 1. SVN: 3-5 ml of 20% solution tid or qid 2. SVN: 6-10 ml of 10% solution tid or qid 3. Direct instillation: 1-2 ml of 10% or 20% solution iv. Mode of Action 1. the sulfhydril group substitutes for the disulfide bond in the mucoprotein complex to decrease viscosity and elasticity 2. See text, page 179, Figure 9-9 v. Hazards 1. bronchospasm a. More likely with 20% solution b. Always administer with a fast-acting betaadrenergic agent 2. stomatitis – inflammation of the stoma 3. nausea – disagreeable odor from hydrogen sulfide 4. rhinorrhea – irritation 5. mechanical obstruction of the airway vi. Handling 1. open vial should be refrigerated a. discard after 96 hours 2. May change to light purple color due to the preservative EDTA a. Does not affect safety or efficacy b. Dornase Alfa (Pulmozyme) (1994) i. Viscolytic enzyme 1. Clone of human enzyme that digests extracellular DNA ii. Indication 1. to preserve or improve lung function in cystic fibrosis 2. to decrease frequency and severity of respiratory infections iii. Mode of Action 1. breaks down DNA in infected secretions a. infected secretions contain DNA (neutrophils) which increases viscosity 2. retained secretions cause infection iv. Administration 1. 2.5 mg (1 ampule) daily, 2.5 ml v. Handling 1. protect from light a. protective foil pouch 2. refrigerate 3. can not be mixed with other medications vi. Common Adverse Effects 1. voice alteration 2. pharyngitis 3. laryngitis 4. rash 5. chest pain 6. conjunctivitis IV. Expectorants a. Sodium Bicarbonate i. Administration 1. 2% solution for inhalation or tracheal irrigation 2-5 ml ii. Mode of Action 1. increases pH of bronchial secretions 2. weakens side chain bonding to decrease viscosity and elasticity iii. Caution 1. may cause local bronchial irritation pH>8.0 a. No systemic pH change 2. No clinical evidence for use b. Aqueous Solutions i. Sterile water ii. Saline solutions 1. hypotonic (0.45%) 2. isotonic (0.9%) 3. hypertonic (5-10%) iii. Administration 1. SVN: 3-5 ml as ordered 2. USN: 3-5 ml as ordered iv. Use 1. sputum induction a. cause vagally mediated irritation to increase coughing and mucus production 2. no evidence that they decrease mucus viscosity by topical hydration or mixing a. gel surface is resistant to addition or removal of H2O b. short term 3-5 ml adds < 1 ml of liquid to lung c. continuous treatment with USN can add large amount of H2O to lung and cause watery secretions Goal of Future Research Agents to restore mucus to normal viscosity and elasticity FOR NOW: Best advice is probably GOOD SYSTEMIC HYDRATION