Lice Exposure Protocol
advertisement

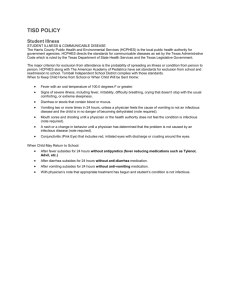
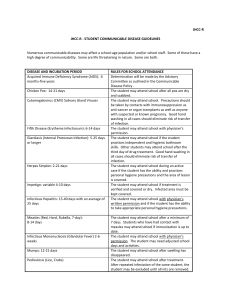
PAGE 1 OF 8 MANAGEMENT OF ILLNESS OR EXPOSURE TO COMMUNICABLE/INFECTIOUS DISEASE TABLE OF CONTENTS Procedure for Reporting Exposure or Illness Notification of Local Health Authority Employees/Patients with a BBP Disease Treatment of Exposure TB Exposure Chicken Pox/Varicella Zoster, Measles, or other Vaccine Preventable Diseases Exposure Meningitis Exposure Pertussis Exposure Influenza Exposure Lice or Scabies Exposure Bloodborne Pathogen (BBP) Exposure Hazardous Substance Exposure Summary of Recommendations for Personnel Exposed to Infectious Diseases Tuberculosis Exposure Protocol Varicella/Herpes Zoster Protocol Measles, Mumps, Rubella and other Vaccine Preventable Diseases Protocol Neisseria Meningitis Exposure Protocol Pertussis Exposure Protocol Influenza Exposure Protocol Lice Exposure Protocol Scabies Exposure Protocol Bloodborne Pathogen (BB) Exposure Protocol 2-3 3 3-4 4 4-5 5 5-6 6 6 6-7 7 7-8 Attachment A Attachment B Attachment C Attachment D Attachment E Attachment F Attachment G Attachment H Attachment I Attachment J Management of Illness or Exposure to Communicable/Infectious Disease I. EH8660-585 Revised: 12/13 Page 2 of 8 POLICY Employees, Licensed Independent Practitioners (LIPs), students/trainees and volunteers will report to their supervisor immediately if they have contracted and/or been exposed to infectious/communicable diseases or are identified as potentially having an infectious disease. Employees will not report to work with symptoms of illness, especially cough or sore throat with fever, rash, drainage from the eye, diarrhea with fever or other undiagnosed potentially contagious illness. Employees with, or exposed to, infectious/communicable diseases will be restricted as outlined in the table in ATTACHMENT A. Employees, LIPs, students, volunteers, other employers, patients, visitors, and contractors will be notified by verbal or written notice if they have been exposed to a suspected or confirmed infectious disease case in the course of their duties. Employees of other agencies or organizations reporting to Lodi Health through the ED, Occupational Health Medicine Clinic, the Urgent Care Clinic or other clinics within the Lodi Health organization with an exposure will be treated according to established standards. II. PROCEDURE A. Employees, LIPs, students/trainees and volunteers, identified as potentially having an infectious disease or illness, will be reported to and followed, as indicated, by the Employee Health Department. The employee will be sent home immediately and instructed to contact the Employee Health Department by telephone for instructions for return to work. 1. 2. 3. Employees, LIPs, students/trainees and volunteers may be referred to the Employee Health Nurse if assessment, testing, immunization and/or prophylaxis/treatment and counseling as indicated. The Employee Health Nurse in consultation with the Infection Preventionist and department Medical Directors and Administration will monitor for trends, establish screens, and determine testing and treatment as indicated by protocol, CDC, OSHA, Cal-OSHA, and/or the Department of Public Health (California and Federal). Return to work is based on ATTACHMENT A criteria. B. Employees, LIPs, students/trainees, volunteers and visitors, identified as potentially exposed to suspect or confirmed infectious disease cases will be contacted and treated as indicated in the protocols (see ATTACHMENTS B-J). C. The Employee Health Nurse, Infection Preventionist, or Department Director may determine if a release to return to work is required. 1. D. A copy of the release will be sent to Employee Health and Human Resources. Employees ill on the job may be seen by the Employee Health Nurse or Urgent Care/ED physician if indicated. Management of Illness or Exposure to Communicable/Infectious Disease E. Employees will report any potentially communicable illnesses or any exposures to communicable diseases to the Employee Health Department and Infection Prevention immediately. 1. 2. 3. 4. 5. F. 2. 3. 4. Initial screening and base line testing is provided at Lodi Health Laboratory free of charge to LIP; all others are billed for the services. Follow-up testing can be done through Lodi Health lab services but may be charged to nonemployee or sent to the clinicians worker’s compensation carrier. Should the non-employee choose to use a lab service other than Lodi Health lab services, the clinician will be financially responsible for that service. The treating provider will give appropriate post-exposure counseling. The non-employee may choose to continue with Lodi Health for follow-up counseling and testing or may go to their own physician/occupational health service. NOTIFICATION OF LOCAL HEALTH AUTHORITY A. Employee Health Services and/or the Infection Preventionist and/or the physician confirming a diagnosis of a communicable disease is responsible for submitting the Confidential Morbidity Report (C.M.R.) to the Preventive/Public Health Services, Morbidity Unit. 1. 2. IV. Employee Health Services will conduct an investigation when notification is received. When indicated, the department director/supervisor will be contacted to generate a list of employees, visitors, patients who may have been exposed. The Employee Health Nurse and Infection Preventionist, if needed, will conduct follow-up investigations on exposed contacts to ensure treatment/resolution. An investigation will be conducted by Employee Health and Infection Prevention, if needed, to determine the cause of the exposure and any practices that may require revision to prevent future exposures. Investigation and follow-up documentation will be completed by Employee Health Services to include requirements outlined in CCR Title 8 § 5199. Documentation is completed utilizing: a. Exposure Analysis & Post Exposure Evaluation Form, and b. Exposure Incident Evaluation Form Lodi Health will provide testing for Bloodborne Pathogen (BBP) exposure for non Lodi Health Employees including: LIP, students, and pre-hospital personnel employees according to regulation and established guidelines. 1. III. EH8660-585 Revised: 12/13 Page 3 of 8 If Employee Health Service is the diagnosing unit, they will file a C.M.R. If the disease is diagnosed by a private physician, he/she will be responsible for filing the C.M.R. EMPLOYEES/PATIENTS WITH A BBP DISEASE A. Employees with AIDS, known to be HIV positive, a Hepatitis B carrier, Hepatitis C positive or other potentially communicable disease will be evaluated according to the type of work performed including direct patient contact. 1. The Employee Health Nurse will review placement and precautions with the employee and complete the Work Clearance and Counseling for Healthcare Workers with HCV, HBV and/or HIV Form. Management of Illness or Exposure to Communicable/Infectious Disease 2. V. These employees will not be permitted to perform procedures or work in positions that require working with sharps without the ability to see the sharp while it is in contact with the patient. (Blind Procedures) TREATMENT OF EXPOSURE A. Follow protocols for specific exposure. (ATTACHMENTS B-J) 1. B. C. If there is no protocol, contact Employee Health or after hours the ER physician on duty for immediate treatment needs. Provide and/or ensure immediate first aid is given. 1. VI. EH8660-585 Revised: 12/13 Page 4 of 8 Eye wash, wash exposed area; remove from immediate danger, etc. Compile a list of those potentially exposed. TB A. Exposure is defined as contact within three feet of a patient diagnosed with pulmonary tubercle Bacillus (tuberculosis) without using respiratory protection equal to or greater than an N95 respirator. B. Department Managers will have potentially exposed employees complete TB Exposure protocol (ATTACHMENT B) and/or send list of names to Employee Health. C. Employee Health, in cooperation with affected Department Managers, will contact potentially exposed employees. D. Upon receipt of employee contact list, Employee Health Services will: 1. 2. 3. 4. 5. 6. 7. 8. 9. E. Sends notices, protocol and testing forms to those potentially exposed informing them of the exposure and the need for baseline and follow-up testing. Instruct employees to report any symptoms as outlined on the TB surveillance form. Do Baseline TSTs on employees who have not had a PPD in the last three months. Do Follow-up TST at least 12 weeks post-exposure if confirmed positive TB. Have employees with a history of a positive PPD test complete the TB History and Respiratory Symptom Review portion of the Tuberculosis Surveillance Form. Provide employee with conversion from a negative to a positive skin test, a PA and lateral chest x-ray. a. Until the results are obtained, the employee may continue to work if they have no signs or symptoms consistent with TB disease. Offer counseling and treatment for latent TB according to CDC and PHD guidelines. Report conversion to Public Health Department. Record all procedures and results in Employee Health Record. If an employee develops signs and symptoms consistent with TB disease, a posterior anterior and lateral check x-ray will be done and the employee will be removed from work until a negative chest x-ray is received. Management of Illness or Exposure to Communicable/Infectious Disease 1. 2. VII. If the chest x-ray is positive, the employee will be referred to a pulmonologist or other appropriate medical doctor for diagnosis and treatment. The employee will be able to return to work when they have completed two weeks of successful drug therapy and are no longer symptomatic. a. A release from the treating physician must be provided prior to return. F. Post-exposure testing is done regardless of annual testing and does not change that mandated annual date. Employees failing to comply with testing requirements within two weeks of notification will not be allowed to work until testing and clearance is obtained. G. Employers of pre-hospital personnel are notified of potential exposure and positive culture results by the Public Health Department, Employee Health, or the Infection Preventionist as needed. CHICKEN POX/VARICELLA ZOSTER, MEASLES OR OTHER DISEASES FOR WHICH IMMUNITY IS PRESENT IN MOST PEOPLE A. Have employee complete and follow the instructions on the protocol ATTACHMENT D. 1. The Employee Health Nurse will review Employee Health Records to determine if the employee has immunity to the specific disease. B. Employees with immunity are not considered exposed. C. Those employees without immunity, or those with no documentation of immunity, will be contacted and immunization, testing or prophylaxis will be provided according to Lodi Health Policy, CDC, and/or Public Health. D. Employee may be restricted from work based on CDC and Public Health guidelines and Lodi Health policy. (ATTACHMENT A) 1. VIII. EH8660-585 Revised: 12/13 Page 5 of 8 Employee Health will adjust restrictions as indicated by the specific disease based on CDC and Public Health guidelines. MENINGITIS A. Exposure is defined as intensive contact with a patient with meningococcal disease (N. meningitides). There is a negligible risk of disease following casual contact. Intensive contact would occur in unprotected: 1. 2. 3. 4. 5. 6. B. Mouth to mouth resuscitation. Suctioning without using proper precautions. Participation in intubation. Oral or fundoscopic examination. Assisting with vomiting patient. Other mucus membrane contact with respiratory secretions. Have the employee complete and follow the instructions on the Meningitis Exposure Protocol Form. (ATTACHMENT E) Management of Illness or Exposure to Communicable/Infectious Disease C. IX. Inform the Pharmacy Department that there has been a confirmed exposure. PERTUSSIS A. Exposure is defined as intensive contact with a patient with Pertussis. There is a negligible risk of disease following casual contact. Intensive contact includes unprotected: 1. 2. 3. 4. 5. 6. B. 2. XI. Mouth to mouth resuscitation. Suctioning without using proper precautions. Participation in intubation. Oral or fundoscopic examination. Assisting with vomiting patient. Other mucus membrane contact with respiratory secretions. Data on the need for post exposure antimicrobial prophylaxis in Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine (Tdap)-vaccinated HCP are inconclusive. Some vaccinated HCP are still at risk for B pertussis. Tdap vaccination may not preclude the need for post exposure antimicrobial prophylaxis. 1. X. EH8660-585 Revised: 12/13 Page 6 of 8 Post exposure antimicrobial prophylaxis is recommended for all HCP who have unprotected exposure to pertussis and are likely to expose a patient at risk for severe pertussis (e.g., hospitalized neonates and pregnant women). Other HCP can receive post exposure antimicrobial prophylaxis or be monitored daily for 21 days after pertussis exposure and treated at the onset of signs and symptoms of pertussis. C. Have the employee complete and follow the instructions on the Pertussis Protocol Form. (ATTACHMENT F) D. Inform the Pharmacy Department that there has been a confirmed exposure. INFLUENZA EXPOSURE A. Large droplet spread through coughing and sneezing is believed to be the primary mode of transmission. Contact with surfaces may also be a source of transmissible particles. Exposure is defined as contact within three feet of a patient diagnosed with influenza without use of respiratory or contact protection. B. Have the employee complete and follow the instructions on the Influenza Protocol Form. (ATTACHMENT G) C. Inform the Pharmacy Department that there has been a confirmed exposure. LICE OR SCABIES EXPOSURE AND TREATMENT A. Definition of exposure to LICE: Occurs when an employee comes into direct contact with another person with lice. Contact must be close head to head, or sharing of same fabric covered chair, lab coats, or other personal items. Time is not a factor to determine exposure. Management of Illness or Exposure to Communicable/Infectious Disease B. Definition of exposure to SCABIES: Occurs when an employee comes into direct skin to skin contact with another person with scabies. Occasionally, transmission may occur when there is contact with heavily contaminated clothing or bed sheets. C. Any employee, who suspects exposure by any source, will immediately notify their director or supervisor. D. Provide the potentially exposed employee(s) with the Scabies or Lice protocol to complete and follow the instructions. (ATTACHMENT H or I) E. If the source of exposure is a patient, the director or supervisor will: 1. 2. 3. F. XII. Initiate isolation of the patient. Notify Infection Prevention immediately with patient name and room number. Have potentially exposed employees complete the protocol and follow the instructions. a. Contact the Pharmacy Department to let them know employees may be reporting for medication. Employees with lice or scabies are relieved from direct patient contact and patient care areas until 24 hours after effective treatment. BLOODBORNE PATHOGEN (BBP) EXPOSURE A. Obtain and complete the BBP Exposure Protocol (ATTACHMENT J) for exposures that include: 1. 2. 3. 4. XIII. EH8660-585 Revised: 12/13 Page 7 of 8 Needle stick, cut or puncture with a device contaminated with another’s blood or bloody fluid. Mucous-membrane contact to eye, nose or mouth with another’s blood or bloody fluid. Contact with large amounts of blood or prolonged contact with blood, or bloody fluids on broken or non-intact skin. Human bite if visibly bloody oral secretions and employee skin is broken. B. Provide employee with signed copies of handouts. Forward originals to Employee Health. C. Instruct the employee to call Employee Health the next work day. HAZARDOUS SUBSTANCE EXPOSURE – CHEMICALS OCCUPATIONALLY RELATED ALLERGIES AND/OR SKIN SENSITIVITIES A. Definition: Intermittent or chronic skin conditions, respiratory, or other condition, which may be related to glove use, latex exposure, chemical use/exposure or other irritants in the work place. B. Employees who have been or feel they have been exposed to a hazardous substance, chemical or other irritant in the workplace will immediately report to their supervisor or seek emergency treatment if in distress. Management of Illness or Exposure to Communicable/Infectious Disease C. The supervisor/director will provide emergency care as indicated and have the employee report to the Emergency Department or Urgent Care Clinic for evaluation and treatment. 1. 2. D. FORMULATED: REVIEWED: REVISED: EH8660-585 Revised: 12/13 Page 8 of 8 Have the employee take a copy of the MSDS sheet for the hazardous substance for physician information. The physician can refer to MSDS sheet and/or call UC Davis Poison Control – 1-800-342-9293 for additional treatment and testing indicated for specific agents. Employees with hand or skin related problems will report to their department director, manager or supervisor for referral to Employee Health for evaluation and treatment. APRIL, 1988 4/01, 4/04, 9/04, 10/07, 11/10, 6/11, 2/13 Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT A Page 1 of 4 SUMMARY OF RECOMMENDATIONS AND WORK RESTRICTIONS FOR PERSONNEL EXPOSED TO OR INFECTED WITH INFECTIOUS DISEASES Disease / Problem Restrict from Direct Patient Contact and Patient Environment Restrict from Work Duration Until discharge ceases and 24 hours of effective treatment. Conjunctivitis, infectious All Yes Cytomegalovirus infections No No All Yes Until symptoms resolve and infection with Salmonella is ruled out. Immunocompromised patients No Until symptoms resolve All Yes Until antimicrobial therapy completed and 2 cultures obtained > 24 hours apart are negative. Infants, neonates, and immunocompromised patients and their environments. No Until symptoms resolve. *Diarrhea disease Acute stage (Diarrhea with other symptoms; fever, abdominal cramps, bloody stools) Convalescent stage Salmonella spp. Diphtheria Enteroviral infections Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT A Page 2 of 4 Disease / Problem Restrict from Direct Patient Contact and Patient Environment Streptococcal infection, Group A All Yes Until 24 hours after adequate treatment is started. Hepatitis A All Yes Until 7 days after onset of jaundice, showing clinical improvement. Hepatitis B Acute No No exposure prone procedures may be performed. Until antigenemia resolves. Hepatitis B Chronic antigenemia No Same as acute illness Hepatitis C, NANB No Same as acute Hepatitis B Herpes Simplex Genital No No All No Until lesions heal Immunocompromised nursery, OB, Peds, Oncology, food handling. No Until lesions heal Hands (herpetic whitlow) Orofacial Restrict from Work Human immunodeficiency virus No Same as acute Hepatitis B Lice (Pediculosis) Yes Yes Duration Period of infectivity has not been determined. Until treated and observed to be free of adult and immature lice. Management of Illness or Exposure to Communicable/Infectious Disease Disease / Problem Measles (Rubeola) Active Restrict from Direct Patient Contact and Patient Environment Restrict from Work EH-8660-585 ATTACHMENT A Page 3 of 4 Duration All Yes Until 7 days after the rash appears. Post exposure (Susceptible personnel) All Yes From the 5th through the 21st day after 1st exposure and/or 4 days after the rash appears. Meningococcal infections Mumps Active All Yes Until 24 hours after start of effective therapy. All Yes Until 9 days after onset of parotitis. All Yes From the 12th through the 26th day after exposure or until 9 days after onset of parotitis. All Yes No No From the beginning of the catarrhal stage through the 3rd week after onset of paroxysms or until 5 days after start of effective antimicrobial therapy. All Yes Until 5 days after start of effective antimicrobial therapy. Rubella Active Post exposure (Susceptible personnel) All Yes Until 5 days after the rash appears. All Yes From the 7th to the 21st day after exposure and/or 5 days after rash appears. Scabies All Yes Until 24 hours after effective treatment. Post exposure (susceptible personnel) Pertussis Active Post exposure (Asymptomatic personnel) Post exposure (Symptomatic personnel) Management of Illness or Exposure to Communicable/Infectious Disease Disease / Problem Staphylococcus aureus (Active, draining skin lesions.) Restrict from Direct Patient Contact and Patient Environment Restrict from Work EH-8660-585 ATTACHMENT A Page 4 of 4 Duration All No All No Yes No All Yes, personnel may not work with a temperature of 100o or more and cough. Until acute symptoms resolve and there is temperature less than 100o for at least 24 hours without antipyretics. All Yes Until all vesicles dry and are crusted. Post exposure (susceptible personnel) All Yes From the 10th through the 21st day after exposure or if varicella occurs until all lesions dry and crust. Zoster (Shingles/Herpes) Localized, in healthy person. Immunocompromised patients No, cover lesions. Until lesions dry and crust. Yes Until lesions dry and crust. Tuberculosis Active Latent (TST Conversion) Viral respiratory infections, acute febrile Varicella (chickenpox) Active Generalized or localized in immunosuppressed personnel. 2. No Until 3 cultures 24 hours apart are negative and medically cleared. From the 10th through the 21st day after exposure or if varicella occurs until all lesions dry and crust. Centers for Disease Control and Prevention, Guidelines for Infection Control in Health Care Personnel, 1998: Recommendations of the Hospital Infection Control Practices Advisory Committee. Centers for Disease Control and Prevention, Immunization of Health-Care Workers: Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC). MMWR, December 26, 1997. 46(RR-18):1-42. Post exposure (susceptible personnel) 1. All Until lesions resolve. All Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT B Tuberculosis Exposure Protocol Print Name Exposure Date Dept. MR# Tuberculosis is caused by Mycobacterium tuberculosis, the tubercle bacillus. The mycobacteria can be found in many organs but transmission occurs when it is present in the lungs or larynx. TB is spread when an infected person coughs, or otherwise aerosolizes particles. Depending on the environment, these particles can remain suspended in the air for hours. If another person inhales air containing the droplet nuclei, transmission may occur. People at highest risk of becoming infected with TB are close contacts – persons who had prolonged, frequent or intense contact with a person with infectious TB. Close contacts may be family members, roommates, friends, and coworkers. HIV immunocompromised contacts have the strongest risk for development of TB if infected. A TB skin test (TST) is performed to determine if a person has been infected with TB. If the skin test is positive, a chest X-ray will be performed to determine if there is active TB disease. Only 10% of people infected with TB will develop active disease. Employees at Lodi Health are tested annually and three months after an exposure to active TB. Please answer the following questions and follow the instructions following. YES NO NA Was source patient's mouth and nose covered when coughing or creating droplets when you were in the same room with him/her? Did you wear a facemask or shield when within three feet of the patient? Did you use a protective facemask if CPR was initiated? If you have answered YES or NA to all of the above questions, you are not likely to have been exposed to TB. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to TB. Employee Signature Date There is no vaccine available against TB. Early identification of TB through screening and timely evaluation and treatment strategies for patients and health care workers with known or suspected TB is the main TB control strategy. What will happen next: If the source patient cultures are positive for Mycobacterium tuberculosis and if you answered NO to any of the questions above: a. If you have not had a TST done in the last three months, you will be contacted to have a baseline TST. b. You will be contacted to have a TST three months after the last date of exposure. References: American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Infectious/Communicable Disease EH-8660-585 ATTACHMENT C Varicella/Herpes Zoster (Chicken Pox/Shingles) Protocol Print Name Exposure Date Dept. MR# Chicken Pox is a viral disease spread by direct contact with vesicular fluid, aerosolized vesicular fluid, secretions from the respiratory tract or contact with objects soiled with vesicular fluid or secretions. Shingles is spread by much the same route but because there are fewer vesicles there is a lower rate of transmission. Shingles are not transmitted by contact with respiratory secretions. You were tested for Chicken Pox antibodies prior to starting work at Lodi Health and were notified and offered two doses of varicella vaccine if you were found to lack immunity. If you were offered vaccine but declined, please answer the following questions and follow the instructions following. YES NO NA Was source patient's mouth and nose covered when coughing or creating droplets when you were in the same room with him/her? Did you wear a facemask or shield when within three feet of the patient? Did you wear gloves for direct contact with respiratory, oral, nasal secretions, or clothing? Did you use a protective facemask if CPR was initiated? If you have answered YES or NA to all of the above questions, you are not likely to have been exposed to Chicken Pox or Shingles. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to Chicken Pox or Shingles. Employee Signature Date If you answered NO to any of the questions above, please complete the bottom section of this form. If you do not have immunity, Varicella vaccine is effective in preventing or modifying the severity of chicken pox if given within three-five days of initial exposure. Please report to Employee Health or obtain vaccine from pharmacy and have administered by licensed healthcare provider. Please read and initial the following: I am not pregnant or lactating. I do not have an immunosuppressive disease. I have received and reviewed the medication information sheet. I understand I must monitor for an elevated temperature and rash for 10-21 days from last exposure. I understand if I develop a fever or rash during the 10-21 days, I must not come to work or expose others. Varicella Vaccine .5cc, sq, Site _______ Lot # ______________ Exp Date _______ By _______________________ Employee Signature References: Date American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT D Measles, Mumps, Rubella (MMR) and other Vaccine Preventable Diseases Protocol Print Name Exposure Date Dept. MR# Vaccine preventable diseases such as Measles, Mumps, or Rubella are rarely a risk for healthcare workers. If a potential exposure occurs, have potentially exposed employees complete this form and return it to Employee Health. Employee Health will determine if there are any potentially exposed employees who may require additional immunization. Please advise employees they will be contacted by Employee Health if treatment is indicated. You were tested for MMR antibodies prior to starting work at Lodi Health and were notified and offered vaccine if you were found to lack immunity. If you were offered vaccine but declined, please answer the following questions and follow the instructions following. YES NO NA Was source patient's mouth and nose covered when coughing or creating droplets when you were in the same room with him/her? Did you wear a facemask or shield when within three feet of the patient? Did you use a protective facemask if CPR was initiated? If you have answered YES or NA to all of the above questions, you are not likely to have been exposed. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure. Employee Signature Date If you answered NO to any of the questions above, please complete the bottom section of this form. If you do not have immunity, MMR vaccine is effective in preventing or modifying the severity of MMR if given within three-five days of initial exposure. Please report to Employee Health or obtain vaccine from pharmacy and have administered by licensed healthcare provider. Please read and initial the following: I am not pregnant or lactating. DO NOT GET MMR if you are pregnant or planning to become pregnant within the next three months. I do not have an immunosuppressive disease. I have received and reviewed the medication information sheet. I understand I must monitor for an elevated temperature and rash for 5-14 days from last exposure. I understand if I develop a fever or rash during the 5-14 days, I must not come to work or expose others. MMR .5cc, sq, Site _______ Lot # ______________ Exp Date _______ By _______________________ Employee Signature References: Date American Public Health Association, Control of Communicable Diseases Manual, 19th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT E Neisseria Meningitis Exposure Protocol Print Name Exposure Date Dept. MR# Neisseria meningitidis is transmitted through close contact with the respiratory secretions of patients with meningococcemia or meningococcal meningitis, or through handling laboratory specimens. The risk of acquiring disease from casual contact, routine patient care, cleaning patient room, delivering food trays, etc. it is negligible. YES NO NA Was source patient's mouth and nose covered when coughing or creating droplets when you were within three feet of him/her? (Respiratory Droplets) Did you wear a facemask or shield when within three feet of the patient? Did you use a protective facemask if CPR was initiated? If you have answered YES or NA to all of the above questions, you are not likely to have been exposed to meningitis. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to meningitis. Employee Signature Date If you answered NO to any of the questions above, read the information below, complete the bottom section of this form and if you decide to take the medication, take this completed form to Pharmacy. Ciprofloxacin or Rifampin is the recommended medication for prophylactic treatment for Neisseria meningitidis. Please read and initial the following: I am not pregnant or lactating. I do not have liver disease and do not take hepatotoxic agents. I do not have renal disease. I do not have an immunosuppressive disease. I understand thrombocytopenia has occurred with high dose intermittent therapy. I understand that repeated doses of antibiotics can reduce sensitivity. I understand that the therapeutic effects of other drugs may be decreased while taking antibiotics. I understand that while taking this medication my urine, feces, saliva, sweat and tears may be redorange and can cause staining of contact lenses. I have received and reviewed the medication information sheet. I understand the above information and (circle one) consent/decline to take Ciprofloxacin or Rifampin as a prophylactic treatment for meningitis exposure. Employee Signature Date Take this form to Pharmacy to receive prophylactic medication: If pregnant, employee must contact OB/GYN for script. Pharmacy please dispense the following: Ciprofloxacin 500 mg PO x 1 dose - Contraindicated in Pregnancy-Refer to OB/GYN OR - If allergy to Ciprofloxacin Rifampin 600 mg PO q 12 hours x 2 days - Contraindicated in Pregnancy-Refer to OB/GYN Pharmacist Signature: _________________________________ References: American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT F Pertussis (Whooping Cough) Exposure Protocol Print Name Exposure Date Dept. MR# Pertussis (Whooping Cough) is caused by the bacteria Bordetella pertussis and is transmitted by direct contact with discharges from respiratory mucous membranes of infected people, by droplets during coughing, medical procedures, etc. It is rarely spread through the air or contaminated objects. To evaluate your level of exposure please answer the following questions and follow the instructions following. YES NO NA Was source patient's mouth and nose covered when coughing or creating droplets when you were within three feet of him/her? (Respiratory Droplets) Did you wear a facemask or shield when within three feet of the patient? Did you wear gloves for direct contact with respiratory, oral, or nasal secretions? Did you use a protective facemask if CPR was initiated? Have you had the Tetanus with Pertussis vaccine within the last 10 years? Do you work in an area other than OB? If you have answered YES or NA to all of the above questions, you are not likely to have been exposed to Pertussis. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to Pertussis. Employee Signature Date If you answered NO to any of the questions above, read the information below, complete the bottom section of this form and if you decide to take the medication, take this completed form to Pharmacy. Zithromax (Azithromycin), Erythromycin or Clarithromycin are the recommended medication for prophylactic treatment for Pertussis. Please read and initial the following: I am not pregnant or lactating. I do not have liver disease and do not take hepatotoxic agents. I do not have renal disease. I do not have an immunosuppressive disease. I understand that repeated doses of antibiotics can reduce sensitivity. I understand that the therapeutic effects of other drugs may be decreased while taking antibiotics. I have received and reviewed the medication information sheet. I understand the above information and (circle one) consent/decline to take the prophylactic treatment for this pertussis exposure. Employee Signature Date Take this form to Pharmacy to receive prophylactic medication: if pregnant, employee must contact OB/GYN for script. Pharmacy please dispense the following: Zithromax 500 mg by mouth for one day, 250 mg by mouth for four days. OR - If allergy to Zithromax Erythromycin 500 mg by mouth four times a day for 14 days - Contraindicated in Pregnancy-Refer to OB/GYN Pharmacist Signature: _____________________________________________ References: American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT G Page 1 of 2 Influenza Exposure Protocol Print Name Exposure Date Dept. MR# Influenza is an acute viral disease of the respiratory tract characterized by fever, cough (usually dry), headache, body aches, extreme fatigue, stuffiness, and sore throat. Cough is usually severe and can last two weeks, other symptoms resolve in two-five days. It is believed the primary spread is by coughing and sneezing by infected persons. The human influenza virus may persist for hours on solid surfaces, particularly in cold, dry climates. Communicability is greatest in the first three-five days of illness but is longer in children and immunocompromised persons. To evaluate your level of exposure please answer the following questions and follow the instructions following. YES NO NA Was source patient's mouth and nose covered when coughing or creating droplets when you were within six feet of him/her? (Respiratory Droplets) Did you wear a facemask or shield when within six feet of the patient? Did you wear gloves for direct contact with respiratory, oral, or nasal secretions? Did you use a protective facemask if CPR was initiated? If you have answered YES or NA to all of the above questions, you are not likely to have been exposed to Influenza. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to influenza. Employee Signature Date If you answered NO to any of the questions above, read the information below. GET VACCINATED If you did not receive the seasonal influenza, it is advised you receive it. The vaccine is effective in preventing or modifying the severity of influenza if given within three-five days of initial exposure. If you decide to get the vaccine, please complete the information below and report to Employee Health or obtain vaccine from pharmacy and have administered by licensed healthcare provider. Please read and initial the following: I have never had a serious allergic reaction or other problem after receiving the vaccine. I have not had Guillain-Barre syndrome within six weeks following a previous dose of influenza vaccine. I understand I must monitor for an elevated temperature and cough for five-seven days from last exposure. I understand if I develop a fever and cough, I must not come to work or expose others. Influenza Vaccine .5cc, sq, Site _______ Lot # ______________ Exp Date _______ By _______________________ I consent to receive the vaccine: Employee Signature Date Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 (EH) ATTACHMENT G Page 2 of 2 MONITOR FOR SYMPTOMS Report to Employee Health and your manager the abrupt onset of fever >101oF, body aches, headache, extreme tiredness, dry cough, sore throat, and runny nose. STAY HOME. IF YOU HAVE A HIGH RISK CONDITION, GET PROPHYLAXIS WITHIN 48 HRS OF EXPOSURE OR ILLNESS CDC does not recommend routine prophylaxis following influenza exposure. Antiviral agents to reduce the duration and severity of symptoms are recommended for those with conditions that confer a higher risk of severe influenza. Conditions include: chronic pulmonary or cardiovascular (not hypertension), renal, hepatic, neurological, hematologic, metabolic disorders including diabetes mellitus, immunosuppressive illness, pregnancy or morbid obesity (BMI >39). Employee Signature Date Take this form to Pharmacy to receive medication: if pregnant, contact OB/GYN for script. Pharmacy, please dispense the following: Tamiflu 75 mg twice daily for five days if symptoms present and within two days of onset OR Tamiflu 75 mg once daily for 10 days if no symptoms, has high risk condition and within two days of exposure. Pharmacist Signature: _____________________________________________ References: American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 (EH) ATTACHMENT H Lice Exposure Protocol Print Name Exposure Date Dept. MR# Lice: Head lice are small insects that live in people's hair and feed on their blood. Lice glue their eggs, or "nits," to hair so that the nits do not get brushed off. Lice die quickly (within two days) without feeding so they cannot live very long away from a person. Nits take six to nine days to hatch, and seven or more days for the lice to become egg-laying adults. People can give head lice to each other when they share combs, hats, clothing, barrettes, helmets, scarves, headphones, or other personal items. There is no preventive treatment for lice; a health care worker must observe for symptoms and be treated if they occur. To evaluate your level of exposure, please answer the following questions and follow the instructions following. YES NO NA Did you have direct unprotected skin-to-skin contact with the infested patient? Did you handle the infested clothing or bedding of an infested patient? Do you have visible lice or nits? If you have answered NO or NA to all of the above questions, you are not likely to have been exposed to Lice nor are you currently infested. Please monitor for symptoms AND REPORT TO Employee Health if they should develop. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to lice. Employee Signature Date If you answered Yes to the last two questions above, read the information below, complete the bottom section of this form and if you decide to take the medication, take this completed form to Pharmacy. Permethrin 5% topical solution is the recommended medication for treatment of Lice. Please read and initial the following: I am not pregnant or lactating. This medication is deemed safe during pregnancy and lactation. I understand all household members must be treated at the same time to prevent re-infestation. I understand all bedding and worn clothing must be changed and washed after treatment. I understand itching will persist for up to two weeks and does not mean treatment has failed. I understand that over treatment should be avoided as some of these medications are toxic. I understand treatment may need to be repeated. I have received and reviewed the medication information sheet. I understand the above information and (circle one) consent/decline to treat my self and household for lice. Employee Signature Date Take this form to Pharmacy to receive the medication: Pharmacy dispenses the following: Permethrin 5% topical solution for employee and household contacts Pharmacist Signature; _____________________________________________ References: American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT I Scabies Exposure Protocol Print Name Exposure Date Dept. MR# Scabies is an infestation of the skin with the microscopic mite Sarcoptes scabiei. Infestation is common, found worldwide and affects people of all races and social classes. Scabies spreads under crowded conditions where there is frequent skin-to-skin contact. Healthcare workers are at risk when there is direct skin-to-skin contact with an infested patient or handling infested clothing or bedding. There is no prophylaxis to prevent infestation, the healthcare worker must observe for symptoms and be treated if they occur. To evaluate your level of exposure, please answer the following questions and follow the instructions following. YES NO NA Did you have direct unprotected skin-to-skin contact with the infested patient? Did you handle the infested clothing or bedding of an infested patient? Do you have red pimple like irritation, burrows, or rash of the skin, especially in the webbing between fingers, toes, skin folds or shoulder blades? Do you have intense itching over the most of the body, especially at night? If you have answered NO or NA to all of the above questions, you are not likely to have been exposed to scabies nor are you currently infested. Please sign below and return this form to Employee Health. I have reviewed the above and do not meet the evaluation criteria for potential exposure to scabies. Employee Signature Date If you answered Yes to the last two questions above, read the information below, complete the bottom section of this form and if you decide to take the medication, take this completed form to Pharmacy. Permethrin 5% topical solution is the recommended medication for treatment scabies. Please read and initial the following: I am not pregnant or lactating. This medication is deemed safe during pregnancy and lactation. I understand all household members must be treated at the same time to prevent re-infestation. I understand all bedding and worn clothing must be changed and washed after treatment. I understand itching will persist for up to two weeks and does not mean treatment has failed. I understand that over treatment should be avoided as some of these medications are toxic. I understand treatment may need to be repeated. I have received and reviewed the medication information sheet. I understand the above information and (circle one) consent/decline to treat my self and household for scabies. Employee Signature Date Take this form to Pharmacy to receive the medication: Pharmacy dispenses the following: Permethrin 5% topical solution for employee and household contacts Pharmacist Signature; _____________________________________________ References: American Public Health Association, Control of Communicable Diseases Manual, 19 th ed. Forward Completed Form to Employee Health Management of Employee Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT J Page 1 of 2 Bloodborne Pathogen Exposure Protocol Employee Name Exposure Date ________________ Home Dept. Source Name _____________________ MR# _________ EXPOSED EMPLOYEE Immediately: Wash punctures or cuts with soap and water. Flush splash to the nose, mouth, or skin with water. Irrigate eyes with clean water, saline or sterile irrigates. Do not squeeze or milk wound as it may cause an immune response that increases the risk of HIV multiplication. Using a caustic agent such as bleach or hydrogen peroxide is not recommended. Did you get stuck or cut by a sharp object that had been in contact with another person’s body fluids or did YES NO another person’s body fluids come in contact with your non-intact skin or mucous membranes (nose, mouth or eyes)? Was the body fluid, blood, or cerebrospinal, synovial, pleural, peritoneal, pericardial, amniotic or other fluid YES NO visibly bloody? If you answered NO to either of these questions, this is not considered an exposure to bloodborne pathogens (BBP). No further testing or treatment related to BBP is indicated. If you answered YES to either question. contact your Shift Supervisor or the Hospital Supervisor for evaluation and treatment. SUPERVISOR Identify source and obtain verbal consent for testing and complete Source Risk Assessment (L:\LMH\FORMS\Employee Health\Attachment J Forms\Source Risk Assessment.doc). If the patient declines, use blood already in the lab. If the source is a baby, the mother is tested. Contact Registration to create Employee Health accounts for Employee and Source. Order: Exposure Panel-Source L:\LMH\FORMS\Employee Health\Attachment J Forms\Exposure Source Lab Form.doc Exposure Panel-Employee L:\LMH\FORMS\Employee Health\Attachment J Forms\Exposed Employee Lab Form.doc Complete BBP Exposure Report/Log with exposed employee. (L:\LMH\FORMS\Employee Health\Attachment J Forms\Exposure Log Incident Report.doc.) Print and send to EH. Print CDC document: Exposure to Blood – What Healthcare Personnel Need to Know. (L:\LMH\FORMS\Employee Health\Attachment J Forms\Exp_to_Blood.pdf.) Give to Employee. Obtain Source Rapid HIV results If source patient is HIV negative and no HIV exposure in the last 6 weeks, post-exposure prophylaxis (PEP) is not indicated. Contact the employee and let them know the results and that Employee Health will contact them with the remaining test results (Hepatitis B & C). If source patient HIV results are positive: Speak to employee face to face to discuss post-exposure prophylaxis (PEP) and complete PEP Information and Consent Form. (L:\LMH\FORMS\Employee Health\Attachment J Forms\PEP Consent and Side Effects.doc) Contact National HIV/AIDS Clinicians’ Consultation Center PEPline 1-888-448-4911 with any questions regarding PEP. They are an awesome resource and are happy to talk to you and the employee 24/7. If employee agrees to PEP, take this protocol to pharmacy, obtain meds and have them take the first dose. Enough medicine will be provided to get them through a long weekend. (4 Days). Employee Health will contact the employee on the next business day. Have the Employee sign the bottom of this form and return all documents to Employee Health. Completed? YES NO YES YES YES NO NO NO YES YES NO NO HIV Results Neg Pos Source Pos and EE Wants PEP? YES NO PEP Provided? YES NO Management of Employee Illness or Exposure to Communicable/Infectious Disease EH-8660-585 ATTACHMENT J Page 2 of 2 PHARMACIST: Please dispense per BBP Protocol. Raltegravir 400 mg po twice daily #8 Truvada Take 1 tablet po once daily #4 Please provide written and verbal instructions. Pharmacist Signature: EXPOSED EMPLOYEE I have been advised of the risks and benefits of PEP for HIV exposure and have been advised that the exposure I sustained: Warrants taking the medication. I will will not take it for the prescribed time. Does not warrant taking the medication. I understand Employee Health will contact me with the remaining source results and any further tests or treatment. Employee signature: _________________________________________________ Date: ___________________________ Return Completed Forms to Employee Health Services for Follow up