Therapeutic devices
advertisement

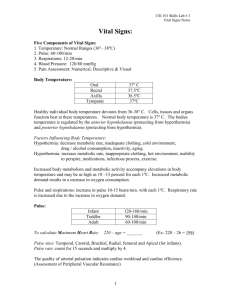
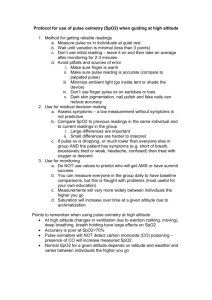
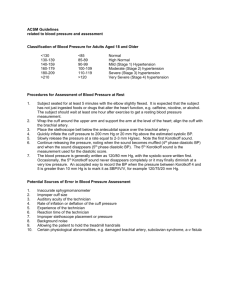
B1-lecture Bioengineering: Definition: Interdisciplinary science which applies engineering methods and techniques to problems in biology and medicine. Any application of the engineering principles of measurement, modeling, or control which impacts on health care delivery. Goals:“Your goal is not to foresee the future, it is to enable it.” (Antoine de Saint-Exupéry, Le Petit Prince) . Characteristics: - merging of different disciplines - merging of medical and engineering methods - practical (must be effective - must solve medical problems effectively). Bioengineering: Life scienses biology, physiology, biochemistry, immunology BIOMATERIALS, IMAGE ANALYSISBIOMECHANI CSBIOINSTRUMENTATION Chemistry, physics, matematics, matematics electronics, mechanics Physical sciences Engineering scienses Categories of medical devices Therapeutic devices Monitoring (measuring) clinical devices Therapeutic devices: 1.Circulation (electrotherapy, defibrillators, pacemakers) 2.Respiration (respirators) 3.CNS (anesthesia) 4.Invasive (surgical) devices (aspiration, vacuum, hand tools, sterilizators, operating tables) 5.General vital functions (incubators) Monitoring (measuring) clinical devices: 1.Circulation, haemodynamics - Pressure - Action potential (ECG) - Heart rate, frequency - Cardiac (circulatory) sounds 2. Respiration 3.Intensive care, monitor systems 4.ThermometryBasics of measurement •Measurement = assignment of numerals to represent physical properties •Two types of measurements for data –Qualitative = non-numerical or verbally descriptive:•Nominal = no order or rank (e.g. list)•Ordinal = allows for ranking but differences between data is meaningless (e.g. alphabetical list)–Quantitative = numerical ranking •Interval = meaningless comparison (e.g. calendar)•Ratio = based on fixed or natural zero point (e.g. weight, pressure)Factors that affects measurements: 1.Error = normal random variation and not a mistake (usually it is caused by the limitation of machine). If you have a non-changing parameter and you measure this repeatedly, the measurement will not always be precisely the same, but will cluster around a mean (Xo). The deviation around Xo = error term, where you can assume your measurement is Xo as long is deviation is small. 2.Validity = statement of how well the instrument measures what it is supposed to measure.3.Reliability = statement of a measurement’s consistency of getting the same values of measurand on different trials4.Repeatability = getting the same value when exposed to the same stimulus 5. Accuracy = freedom from error, how close is a measurement to a standard. Ex. mercury manometry vs aneroid devices*; indirect blood pressure vs catheter*; mean value of normal distribution is close to true value6. Precision = exactness of successive measurements. It has small standard deviations and variance under repeated trials. * see later 1.Make measurements several times 2.Make measurements on several instruments 3.Make successive measurements on different parts of instruments (different parts of ruler, Bürker’s chamber, image analyzer, etc.) Non invasive cardiovascular monitoring Definition: Monitoring procedures or modalities that do not involve breaching of the skin and/or mucosa Indication: Cardiovascular diseases, diagnosis - all patients who need cardiovascular monitoring Advantages: •Indicated for all patients •Do not require sophisticated equipment •Easy to set up •Absence of major complications•Limitations: •Low data reliability in sick patients •Pulse oximetry, non-invasive blood pressure •Unable to obtain sophisticated data (cardiac output)Modalities: •Clinical observations •Pulse •Blood pressure •Electrocardiogram •Pulse oximetry Clinical observations: •General condition, mental state •Dyspnoea, tachypnoea •Capillary refill, peripheral circulation •Jugular venous pressure (JVP) Pulse •It has been used for thousands of years by medical practitioners •It requires no equipment •It is applicable to all patientsLimitations –It is non-specific –Wide inter- and intra-observer variation –Need good clinical experience –Initial assessment of patient –Peripheral vascular disease –Post major vascular repair Pressure measurements = understanding the patient’s (cardiovascular) condition.Sine qua non of correct circulatory diagnosis, treatment (= success of clinical practice)Indirect or Direct Manual or Oscillotonometry (‘electric’) •Mercury manometer•Aneroid manometer1905: Nikolai Korotkoff (Russian army surgeon) observed the sounds made by the constriction of the artery (characteristic sounds at certain points in the inflation and deflation of the cuff). Korotkoff sounds are caused by the abnormal passage of blood through the artery, corresponding to the systolic and diastolic blood pressures. Profile of Korotkov (Korotkoff) sounds Mercury manometer - the gold standard of indirect pressure measurement: Aneroid technique: The metal bellows expands as cuff pressure increases and is read by a needle on its dial. Users can not be certain the device is accurate even when the needle is positioned at zero when the cuff is deflated. Calibration: use a Y connector and compare an aneroid device to an accurate mercury manometer. Manual blood pressure: •Korotkoff IV vs V sound –Korotkoff IV is a better indication of diastolic pressure according to theory –However Korotkoff V is the commonly recommended measuring point except in pregnant patients because •It is associated with less inter-observer variations •It is easier to detect by most observer•Korotkoff sounds vs invasive blood pressure –Korotkoff IV is on average 8 mmHg above the invasively measured diastolic blood pressure –Korotkoff V is on average 2 mmHg above the invasively measured diastolic blood pressure Standardized technique1. No caffeine in the preceding hour. 2. No smoking or nicotine in the preceding 15-30 minutes. 3. No use of substances containing adrenergic stimulants such as phenylephrine or pseudoephedrine (may be present in nasal decongestants or ophthalmic drops). 4. Bladder and bowel comfortable. 5. Quiet environment. Comfortable room temperature. 6. No tight clothing on arm or forearm. 7. No acute anxiety, stress or pain. 8. Patient should stay silent prior and during the procedure. The patient should be calmly seated for at least 5 minutes, with his or her back well supported and arm supported at the level of the heart. - His or her feet should touch the floor and legs should not be crossed. - The patient should be instructed not to talk prior and during the procedure. •Use a mercury manometer or a recently calibrated aneroid or a validated electronic device.•Aneroid devices should only be used if there is an established calibration check every 6-12 months.–Position cuff at the heart level–Arm should be supported –Pressure is related to height ( Δp = ρgΔh ! ).–Manometer should be leveled, the column of mercury must be vertical, and at the observers eye level. The patient must not watch the reading. –Place stethoscope over the brachial artery –To exclude possibility of auscultatory gap, increase cuff pressure rapidly to 20-30 mmHg above level of disappearance of radial pulse –Drop pressure by 2 mmHg / sec •Appearance of sound (phase I Korotkoff) = systolic pressure –Record measurement –Drop pressure by 2 mmHg / beat •Disappearance of sound (phase V Korotkoff) = diastolic pressure –Record measurement –Take 2 blood pressure measurements, 1 min apart•For initial readings, take the blood pressure in both arms and subsequently measure it in the arm with the highest reading. •Thereafter, take two measurements on the side where BP is highest.The standing blood pressure is used to test for postural hypotension, if present, which may modify the treatment. For patients > 65 / diabetics / treated with antihypertensives: check if there are postural changes while taking blood pressure reading, i.e. after 1-5 min in the standing position and under circumstances when the patients complains of symptoms suggestive of hypotension. Interpretation: •It was shown that the mean pressure obtained by oscillotonometry correlates best with other means of blood pressure monitoring •It is also the parameter that is most reproducible.Problem: Bruises and petechiae under the cuffLimitations: Inaccurate / unreliable in shock patients Inaccurate / unreliable in patients with arrhythmias The algorithm of measurement assumes a regular pulse, so the reading is un-reliable in patients with irregular pulse.Pulse pressure (PP) = systolic pressure – diastolic pressure = measurement of the amplitude of the blood pressure waveNormal 35 - 40 mmHg < 30 mmHg pulse hard to detect Decreasing pulse pressure early sign of inadequate circulating blood volume 1. Current data underscores the role of increased arterial stiffness in the development of cardiovascular events. 2. Changes in the circulation tend to affect primarily the systemic vascular resistance at the level of the smaller vessels. 3. In younger people, the increase in vascular resistance is reflected by an elevation in both systolic and diastolic pressure. 4. In time, however, the relative contribution of increased vascular resistance to elevated blood pressure lessens, and the role of large-vessel stiffness increases. Emergency Medicine ww.emedmag.com It provides information on- Heart rate- Atrial, ventriculal rhythm- Status of myocardial oxygenation - ST segment analysis- Myocardial diseases- Electrolyte disturbance- Serum K+ level affects the ECG in a predictable and dose related manner- Drug toxicity (digitalis, tricyclic antidepressant, anti-cholinesterase, etc.)Pulse oximetry Continuous non-invasive method for measuring arterial oxygen saturation and pulse rate The success of pulse oximetry depends on its ability to measure the saturation of the arterial blood by analysis of infrared absorption of vascular bed throughout the whole pulsatile pulse cycle.Pulse oximetry = photoplethysmograph The photoplethysmograph (PPG) is an optical means of conducting a plethysmography. So what is a plethysmography? PG is a term for a set of noninvasive techniques for measuring volume changes in parts of the body (even the whole body) Commonly measured volume changes are: - caused by breathing (lung and chest expansion) - caused by blood being forced into vessels (such as arteries, veins and capillaries) - caused in the heart as it pumps The two main techniques (the methods are flexible):- Volume displacement plethysmography - Electrical impedance plethysmography It is also possible to acquire a PG using ultrasonic or X -Ray imaging A photoplethsymograph refers to a technique whereby localised volume changes due to an optically absorbant/scattering substance (e.g . blood ) are measured. Uses spectrophotometry based on the Beer-Lambert law (linear relationship between absorbance and concentration of an absorbing species) A = a(λ) * b * cA is the measured absorbance (fraction of light absorbed)a(λ) is wavelength-dependent absorptivity coefficientb is the path lengthc is the analyte concentration Principle of operation: infrared absorption by oxygenated and de-oxygenated haemoglobin at two different wavelengths. Differentiates oxy- from deoxyhemoglobin by the differences in absorption at 660nm and 940nmLimitations •Patient movement •Ambient light •Peripheral circulatory dysfunction •Sats below 85% increase the importance of error in the reading •Calibration is performed by company on normal patients breathing various gas mixtures•Skin pigmentation •Darker color may make the reading more variable due to optical shunting. •Dark nail polish has same effect: blue, black, and green polishes underestimate saturations, while red and purple have no effect •Hyperbilirubinemia has no effect Carbon monoxide poisoning: CO has 200-250 greater affinity for the Hbg molecule than O2, binds at the O2 binding site and prevents on-loading of O2.Carboxyhemoglobin can not be distinguished from oxyhemoglobin by pulse oximetry - erroneously high reading may present Suspect the presence of carboxyhemoglobin in patient with: - smoke inhalation - intentional and accidental CO poisoning - heavy cigarette smoking Treat carboxyhemoglobin with high flow O2 irregardless of the pulse oximetry reading!Affect of anemia (low quantities of erythrocytes or hemoglobin) is debated Normal value of hemoglobin is 11-18 g/dl Values as low as 5 g/dl may result in 100% SpO2 Anemic patients require high levels of oxygen to compensate for low oxygen carrying capacities! Severe peripheral vasoconstriction may prevent oximetry detection •Shivering may result in erroneous oximetry motion •Pulse rate on oximeter must coincide with palpable pulse rate to be considered accurate Treat the patient according to hypothermic guidelines and administer oxygen accordingly! Interpreting pulse oximetry: Assess and treat the patient not the oximeter.Use oximetry as an adjunct to patient assessment and treatment evaluation Never withhold O2 if the patient has signs or symptoms of hypoxia or hypoxemia irregardless of oximetry readings!