BREAST CLINIC REFERRAL - Barts Health NHS Trust
advertisement

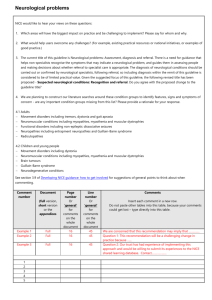
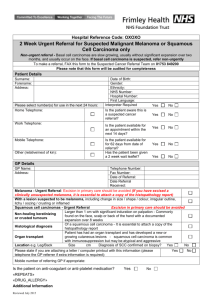
BRAIN / CNS Suspected Cancer Referral (2 Week Wait Referral) To support NICE guidance 2005 Please FAX within 24 hours to Cancer Pathways department: 020 8928 8836 Section 1 PATIENT INFORMATION (Please complete in BLOCK CAPITALS) Date of Referral Date of Birth NHS number UBRN SURNAME FIRST NAME Miss Mrs Ms Mr Other:_________ / / / / - - Home Tel. M[ ]F [ ] Mobile/Daytime Tel. Address Transport Y N Interpreter Y N Language Ethnicity Post Code Section 2 PRACTICE INFORMATION (Please use practice stamp if available) Referring GP Locum Practice Address Y N Telephone Fax Post Code Section 3 CLINICAL INFORMATION (please TICK all applicable entries) Please enclose print outs of CURRENT medications and PAST MEDICAL HISTORY Signs and symptoms for urgent referral [ ] Focal Seizures and other neurological features [ ] Papilloedema [ ] New onset early morning headache and drowsiness with early morning vomiting and ataxia [ ] Progressive focal neurological signs on examination suggestive of an intracranial tumour If your patient does not meet any of these criteria, or symptoms/signs of brain tumour is suspected or unsure if tumour or other brain pathology, or if the patient has severe symptoms please contact the neurological SPR or consultant to discuss the referral (see local contacts at the top of the guideline) INVESTIGATIONS Medical History, Known Allergies and Medication Discussed urgent suspected cancer referral with patient: Y N Comments/other reasons for suspecting a brain tumour Hospital use only: (Tick where appropriate) Date Appointment Booked: Target Dates 2ww 62/7 / / / / / / Date of Referral receipt: Database: / Patient confirmed: / A separate letter only need accompany if you feel it necessary Approved by the North East London Cancer Network April 2006 LOCAL CONTACT DETAILS If you wish to discuss any clinical issues concerning this referral please contact: Dr Anish Bahra Consultant Neurologist 020 8539- Ext 6687 If you wish to discuss any other aspect of this referral please contact the Cancer Pathways Office on 020 8535 6856/ 020 8535 6768 x4348 x4350 CRITERIA FOR URGENT SUSPECTED CANCER REFERRAL1 Please FAX the referral form within 24 hours Refer a patient who presents with symptoms suggestive of brain or CNS cancer to an appropriate specialist, depending on local arrangements. Discuss any concerns about a patient’s symptoms and/or signs with a local specialist. If rapid access to scanning is available, consider as an alternative to referral. Re-assessment and re-examination is required if the patient does not progress according to expectations. Urgently refer patients with: Symptoms related to the CNS in whom a brain tumour is suspected including: o Progressive neurological deficit (e.g. Hemiparesis) o New onset seizures o Headaches with vomiting and papillodema o Mental changes o Cranial nerve palsy / unilateral sensorineural deafness Early morning headaches of recent onset accompanied by features suggestive of raised intracranial pressure, e.g. vomiting, drowsiness, posture related headache (worse when lying down), or by other focal or nonfocal neurological symptoms (e.g. blackout, change in personality or memory) A new, qualitatively different, unexplained headache that becomes progressively severe and of up to two weeks duration Refer urgently patients previously diagnosed with any cancer who develop any of the following symptoms, e.g. recent-onset seizure, progressive neurological deficit, persistent headaches, new mental or cognitive changes or new neurological signs. Consider urgent referral to an appropriate specialist in patients with rapid progression of: o Subacute focal neurological deficit o Unexplained cognitive impairment, behavioural disturbance or slowness, or a combination of these o Personality changes confirmed by a witness and for which there is no reasonable explanation even in the absence of the other symptoms and signs of a brain tumour Please do not use the proforma for non urgent referrals Refer the patient by means of a routine referral letter Investigations In a patient with new, unexplained headaches or neurological symptoms, undertake a neurological examination guided by the symptoms, but including examination for papilloedema. Note that the absence of papilloedema does not exclude the possibility of a brain tumour. When a patient presents with seizure, take a detailed history from the patient and an eyewitness to the event. Carry out a physical examination, including cardiac, neurological and mental state, and developmental assessment, where appropriate. 1 Based on Referral Guidelines for Suspected Cancer (NICE, 2005) Notes in grey refer to the evidence grading used in the NICE guidelines, for more information see www.nice.org.uk/cg027NICEguideline